Epidermoid cyst
An epidermoid cyst or epidermal inclusion cyst[1] is a benign cyst usually found on the skin. The cyst develops out of ectodermal tissue. Histologically, it is made of a thin layer of squamous epithelium.
| Epidermoid cyst | |
|---|---|
| Epidermal cyst in the earlobe | |
| Specialty | Dermatology |
Signs and symptoms
The epidermoid cyst may have no symptoms, or it may be painful when touched. It can release macerated keratin. In contrast to pilar cysts, epidermoid cysts are usually present on parts of the body with relatively little hair.[2] An epidermoid cyst is one type of vaginal cyst.[3]
Occasionally, an epidermoid cyst will present with trigeminal neuralgia.
Although they are not malignant, there are rare cases of malignant tumors arising from an epidermoid cyst.[4]
Causes
Epidermoid cysts commonly result from implantation of epidermis into the dermis, as in trauma or surgery. They can also be caused by a blocked pore adjacent to a body piercing. They are also seen in Gardner's syndrome and Nevoid basal-cell carcinoma syndrome on the head and neck. They can be infected by bacteria and form a pimple-like shape.
Diagnosis

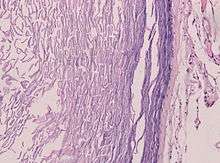

Epidermoid cysts are usually diagnosed when a person notices a bump on their skin and seeks medical attention. The definitive diagnosis is made after excision by a pathologist based on microscopic appearance of a cystic lesion lined by cornified epithelium containing lamellated keratin without calcifications. They can also be seen as isointense lesions on MRI or hyperintensities on FLAIR.
Treatment
Cysts can be removed by excision.[5]
In case of fronto-ethmoidal epidermoid cysts, surgical resection appears to be the mainstay of treatment; however, the extent of resection is dictated by adherence of the tumor capsule to the surrounding vital structures.[6]
Hydrogen peroxide gel (H2O2) was previously recommended for cyst treatment, particularly those on body piercings. However the gel cannot adequately permeate the cyst and was not found to be effective.[7] Hydrogen peroxide is no longer recommended for wound care by doctors as it can damage the healing tissues.[8]
On body piercings, self treatment with a hot saline soak to help drain the cyst and the use of an antibacterial or medicated talcum powder to help dry out the bump and reduce bacterial proliferation is generally recommended until medical advice can be obtained.[9] (Use of talc is no longer recommended due to recently discovered associations with multiple cancers.) Piercings, however, are more likely to be victims of hypertrophic scarring than a cyst. Cheek piercings seem to be the piercing most prone to cysts due to the possible interruption of saliva ducts.
Terminology
Several synonyms exist for epidermoid cysts, including epidermal cyst, infundibular cyst, keratin cyst and epidermal inclusion cyst[10][11]:778[12] Epidermal inclusion cyst more specifically refers to implantation of epidermal elements into the dermis. The term infundibular cyst refers to the site of origin of the cyst: the infundibular portion of the hair follicle. The majority of epidermal inclusion cysts originate from the infundibular portion of the hair follicle, thus explaining the interchangeable,[13] yet inaccurate, use of these two terms.
Another similar and easily confused cyst is the sebaceous cyst. Since L72.0, it is often mixed up with L72.1.
See also
- Intracranial epidermoid cyst
- List of cutaneous neoplasms associated with systemic syndromes
- Proliferating epidermoid cyst
- Verrucous cyst
References
- "Epidermal inclusion cyst information Diseases Database". www.diseasesdatabase.com. 17 February 2018.
- "cysts - British Association of Dermatologists". Archived from the original on 2008-01-10. Retrieved 2007-11-14.
- Zimmern, Francois Haab, Christopher R. Chapple (2006). Vaginal Surgery for Incontinence and Prolapse. Springer Science & Business Media. p. 271. ISBN 1852339128. Retrieved March 2, 2018.CS1 maint: uses authors parameter (link)
- Jehle KS, Shakir AJ, Sayegh ME (2007). "Squamous cell carcinoma arising in an epidermoid cyst". British Journal of Hospital Medicine (London, England : 2005). 68 (8): 446. doi:10.12968/hmed.2007.68.8.24499. PMID 17847698.
- "Minimal excision technique for removal of an epidermoid cyst". Am Fam Physician. 65 (7): 1423–4. 2002. PMID 11996427.
- "Epidermoid Cysts in the Frontal Lobe – A Case Series - Journal of Pioneering Medical Sciences". www.jpmsonline.com. Archived from the original on 27 July 2014. Retrieved 2 April 2018.
- Graziani, F; Vano, M; Tartaro, G; Fanelli, G; Gabriele, M (2003). "The use of hydrogen peroxide in the experimental therapy of cysts. An in vitro analysis". Minerva Stomatologica. 52 (7–8): 373–7, 378–80. PMID 14608258.
- Walsh, L. J. (2000). "Safety issues relating to the use of hydrogen peroxide in dentistry". Australian Dental Journal. 45 (4): 257–69, quiz 289. doi:10.1111/j.1834-7819.2000.tb00261.x. PMID 11225528.
- "Archived copy". Archived from the original on 2014-04-23. Retrieved 2014-04-21.CS1 maint: archived copy as title (link)
- Melton, Jason R. Swanson and Jeffrey L. "Epidermoid cyst". www.meddean.luc.edu.
- Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- "Epidermoid cyst". Retrieved 2007-11-14.
External links
| Classification | |
|---|---|
| External resources |