Empty nose syndrome
Empty nose syndrome (ENS), one form of secondary atrophic rhinitis, is a clinical syndrome in which people who have clear nasal passages experience a range of symptoms, most commonly feelings of nasal obstruction, nasal dryness and crusting, and a sensation of being unable to breathe.[1]
| Empty nose syndrome | |
|---|---|
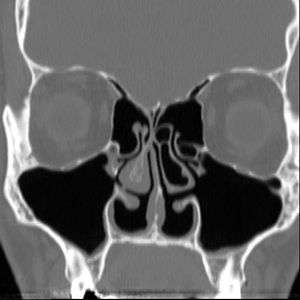 | |
| Altered nasal anatomy after bilateral subtotal inferior turbinectomy | |
| Specialty | Otolaryngology |
ENS can be caused by minor surgical procedure as well as by major nasal surgical procedure:[1][2][3][4][5]
- major procedures: turbinate surgery (turbinectomy, turbinoplasty) for removal or reduction or modification of turbinates
- minor procedures: submucosal cautery, submucosal resection, laser therapy, and cryosurgery.
It appears to be a health care caused condition but its existence as a medical condition, cause, diagnosis and management are controversial.[1] All aspects have been subject to debate, including whether it should be considered solely rhinologic, or may have neurological or psychosomatic aspects.[1][2][6][7][8][9] As of 2015 many ear, nose, and throat doctors do not recognize the condition.[6]
Signs and symptoms
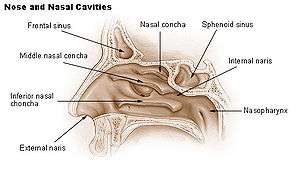
There are no objective physical examination findings that definitely diagnose ENS.[1] Generally, one or more turbinates may be reduced or absent when viewed in medical imaging or via endoscope with no sign of physical obstruction, the mucosa will be dry and pale, and there may be signs of secondary infection.[1]
Symptoms of ENS include a sensation of being unable to breathe, a feeling of nasal obstruction and dryness, and crusting, oozing, and foul smells inside the nose from infections.[1] A person with ENS may complain of pain in their nose or face, an inability to sleep and fatigue, and feeling irritated, depressed, or anxious; they may be constantly distracted by the sense that they are not getting enough air.[1]
A study, found that 77% of patients with empty nose syndrome have hyperventilation syndrome.[10]
Cause
The cause may be changes to the nasal mucous membrane and to the nerve endings in the mucosa resulting from chronic changes to the temperature and humidity of the air flowing inside the nose, caused in turn by removal or reduction of the turbinates.[1][2] Direct damage to the nerves may be a result of surgical intervention; however, as of 2015, there is no technology that allows the mapping of the sensory nerves within the nose, so it is difficult to determine whether this is causative of ENS.[1] Investigators have been unable to identify consistent diagnostic or precipitating features, psychological causes leading to a psychosomatic condition have been proposed.[1][6][7][9]

Diagnosis
No consensus criteria exist for the diagnosis of ENS; it is typically diagnosed by ruling out other conditions, with ENS remaining the likely diagnosis if the signs and symptoms are present.[1][2][6] A "cotton test" has been proposed, in which moist cotton is held where a turbinate should be, to see if it provides relief; while this has not been validated nor is it widely accepted, it may be useful to identify which people may benefit from surgery.[1][2][6]
As of 2015, protocols for using rhinomanometry to diagnose ENS and measure response to surgery were under development,[2][6] as was a standardized clinical instrument (a well defined and validated questionnaire) to obtain more useful reporting of symptoms.[6]
A validated ENS-specific, 6-item questionnaire called the Empty Nose Syndrome 6-item Questionnaire (ENS6Q) was developed as an adjunct to the standard Sino-Nasal Outcome Test 22 (SNOT-22).[11] The ENS6Q is the first validated, specific, adjunct questionnaire to the SNOT-22. It can more reliably identify patients suspected of ENS.[12] The ENS6Q is gaining usage in studies on ENS.
Classification
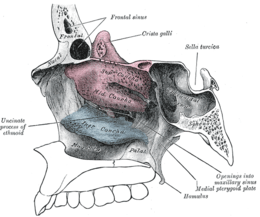
Four types have been proposed:[1]
- ENS secondary to inferior turbinate resection
- ENS secondary to middle turbinate resection
- ENS secondary to both inferior and middle turbinate
- ENS after turbinate-sparing procedures
Treatment
Initial treatment is similar to atrophic rhinitis, namely keeping the nasal mucosa moist with saline or oil-based lubricants and treating pain and infection as they arise; adding menthol to lubricants may be helpful in ENS, as may be use of a cool mist humidifer at home.[1] For people with anxiety, depression, or who are obsessed with the feeling that they can't breathe, psychiatric or psychological care may be helpful.[1][6]
In some people, surgery to restore missing or reduced turbinates may be beneficial.[1]
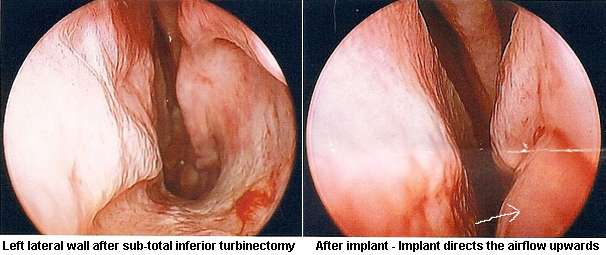
A 2015 meta-analysis identified 128 people treated with surgery from eight studies that were useful to pool, with an age range of 18 to 64, most of whom had been suffering ENS symptoms for many years. The most common surgical approach was creating a pocket under the mucosa and implanting material - the amount and location were based on the judgement of the surgeon. In about half the cases a filler such as noncellular dermis, a medical-grade porous high-density polyethylene, or silastic was used and in about 40% cartilage taken from the person or from a cow was used. In a few cases hyaluronic acid was injected and in a few others tricalcium phosphate was used. There were no complications caused by the surgery, although one person was over-corrected and developed chronic rhinosinusitis and two people were under-corrected. The hyaluronic acid was completely resorbed in the three people who received it at the one year follow up, and in six people some of the implant came out, but this did not affect the result as enough remained. About 21% of the people had no or marginal improvement but the rest reported significant relief of their symptoms. Since none of the studies used placebo or blinding there may be a strong placebo effect or bias in reporting.[6]
Outcomes
Empty nose syndrome has been observed to affect a small proportion of people who have undergone surgery to the nose or sinuses, particularly those who have undergone turbinectomy (a procedure that removes some of the bones in the nasal passage). The incidence of ENS is variable and has not yet been quantified.[1][2][6][7][13]
Untreated, the condition can cause significant and longterm physical and emotional distress in some people; some of the initial presentations on the condition described people who committed suicide.[6] It is difficult to determine what treatments are safe and effective, and to what extent, in part because the diagnosis itself is unclear.[6]
History
As early as 1914, Dr Albert Mason reported cases of "a condition resembling atrophic rhinitis" with "a dryness of the nose and throat" following turbinectomy. Mason called the turbinates "the most important organ in the nose" and claimed they were "slaughtered and removed with discriminate abandon more than any other part of the body, with the possible exception of the prepuce."[14]
The term "Empty Nose Syndrome" was first used by Eugene Kern and Monika Stenkvist of the Mayo Clinic in 1994.[1] Kerm and Eric Moore published a case study of 242 people with secondary atrophic rhinitis in 2001 and were the first to attribute the cause to prior sinonasal surgery in the scientific literature.[1][15] Whether the condition existed or not and whether surgery was a cause, was hotly debated at Nose 2000, a meeting of the International Rhinologic Society that occurs every four years, and continued to be debated thereafter at scientific meetings and in the literature;[1][16] as an example of how heated the debate became, in a 2002 textbook on nasal reconstruction techniques, two surgeons from University of Utrecht called turbinectomies a "nasal crime".[1]
Society and culture
As of 2016, according to Spencer Payne, a doctor who studies ENS, many people with ENS symptoms commonly encounter doctors who consider their symptoms to be purely psychological;[17] according to Subinoy Das, another doctor who studies ENS, recognition among rhinologists was growing.[18]
People who experience ENS have formed online communities to support one another[1] and to advocate for recognition, prevention, and treatments for ENS.[18]
References
- Kuan EC, Suh JD, Wang MB. Empty nose syndrome. Curr Allergy Asthma Rep. 2015 Jan;15(1):493. Review. PMID 25430954
- Sozansky J, Houser SM. Pathophysiology of empty nose syndrome. Laryngoscope. 2015 Jan;125(1):70-4. Review. PMID 24978195
- Houser, Steven M. (2007-09-01). "Surgical Treatment for Empty Nose Syndrome". Archives of Otolaryngology–Head & Neck Surgery. 133 (9): 858–863. doi:10.1001/archotol.133.9.858. ISSN 0886-4470.
Although total turbinate excision is most frequently the cause of ENS, lesser procedures (eg, submucosal cautery, submucosal resection, cryosurgery) to reduce the turbinates may cause problems as well if performed in an overly aggressive manner.
- "FFAAIR | Syndrome du Nez Vide (SNV)". www.ffaair.org (in French). Retrieved 2019-09-11.
suite d’interventions endonasales diverses (turbinectomie, turbinoplastie, cautérisation
- Saafan. "Empty nose syndrome: etiopathogenesis and management". www.ejo.eg.net. Retrieved 2019-09-11.
ENS is a complication of middle and/or inferior turbinate surgery, most frequently total turbinate excision, but also with minor procedures such as submucosal cautery, submucosal resection, laser therapy, and cryosurgery if performed in an aggressive manner
- Leong SC. The clinical efficacy of surgical interventions for empty nose syndrome: A systematic review. Laryngoscope. 2015 Jul;125(7):1557-62. Review. PMID 25647010
- Coste A, Dessi P, Serrano E. Empty nose syndrome. Eur Ann Otorhinolaryngol Head Neck Dis. 2012 Apr;129(2):93-7. Review. PMID 22513047
- Hildenbrand T, Weber RK, Brehmer D. Rhinitis sicca, dry nose and atrophic rhinitis: a review of the literature. Eur Arch Otorhinolaryngol. 2011 Jan;268(1):17-26. Review. PMID 20878413
- Payne SC. Empty nose syndrome: what are we really talking about? Otolaryngol Clin North Am. 2009 Apr;42(2):331-7, ix-x. Review. PMID 19328896
- Mangin, David; Bequignon, Emilie; Zerah-Lancner, Francoise; Isabey, Daniel; Louis, Bruno; Adnot, Serge; Papon, Jean-François; Coste, André; Boyer, Laurent (September 2017). "Investigating hyperventilation syndrome in patients suffering from empty nose syndrome". The Laryngoscope. 127 (9): 1983–1988. doi:10.1002/lary.26599. ISSN 1531-4995. PMID 28407251.
- Soler, ZM; Jones, R; Le, P; Rudmik, L; Mattos, JL; Nguyen, SA; Schlosser, RJ (March 2018). "Sino-Nasal outcome test-22 outcomes after sinus surgery: A systematic review and meta-analysis". The Laryngoscope. 128 (3): 581–592. doi:10.1002/lary.27008. PMC 5814358. PMID 29164622.
- Velasquez N, Thamboo A, Habib A-RR, Huang Z, Nayak JV (2017). "The Empty Nose Syndrome 6‐item Questionnaire: a validated 6‐item questionnaire as a diagnostic aid for empty nose syndrome patients". Int Forum Allergy Rhinol. 7: 64–71. doi:10.1002/alr.21842. PMID 27557473.CS1 maint: multiple names: authors list (link)
- Gehani NC and Houser S. Septoplasty, Turbinate Reduction, and Correction of Nasal Obstruction. Chapter 42. in Bailey's Head and Neck Surgery: Otolaryngology. Ed Jonas Johnson: Lippincott Williams & Wilkins, Jul 9, 2013 ISBN 9781609136024
- Mason, Albert (September 1914). "A plea for the conservation of the inferior turbinate". Atlanta Journal-record of Medicine. 61: 245–249.
- Moore EJ, Kern EB. Atrophic rhinitis: a review of 242 cases. Am J Rhinol. 2001 Nov-Dec;15(6):355-61. PMID 11777241
- Aaron Zitner for The Los Angeles Times. May 10, 2001 Sniffing at Empty Nose Idea
- Tomas Harmon for CBS19 May 4, 2016 Medical Mystery: Empty Nose Syndrome
- Joel Oliphint for BuzzFeed. April 14, 2016 Is Empty Nose Syndrome Real? And If Not, Why Are People Killing Themselves Over It