Duodenum
The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In fish, the divisions of the small intestine are not as clear, and the terms anterior intestine or proximal intestine may be used instead of duodenum.[3] In mammals the duodenum may be the principal site for iron absorption.[4]
| Duodenum | |
|---|---|
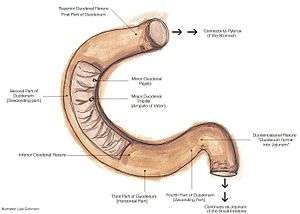
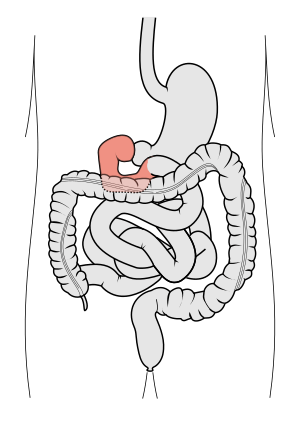 Schematic diagram of the gastrointestinal tract, highlighting the duodenum. | |
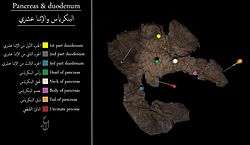 duodenum parts | |
| Details | |
| Precursor | Foregut (1st and 2nd parts), Midgut (3rd and 4th part) |
| Artery | Inferior pancreaticoduodenal artery, Superior pancreaticoduodenal artery |
| Vein | Pancreaticoduodenal veins |
| Nerve | celiac ganglia, vagus[1] |
| Identifiers | |
| Latin | Intestinum duodenum |
| MeSH | D004386 |
| TA | A05.6.02.001 |
| FMA | 7206 |
| Anatomical terminology | |
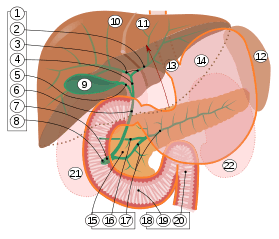
9. Gallbladder, 10–11. Right and left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. 15. Pancreas: 16. Accessory pancreatic duct, 17. Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22. Right and left kidneys.
The front border of the liver has been lifted up (brown arrow).[2]
The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.
In humans, the duodenum is a hollow jointed tube about 25–38 cm (10–15 inches) long connecting the stomach to the jejunum. It begins with the duodenal bulb and ends at the suspensory muscle of duodenum.[5] It can be divided into four parts.
Etymology
The name duodenum (/ˌduːəˈdiːnəm, duˈɒdɪ-/) is from Medieval Latin, short for intestīnum duodēnum digitōrum, which may be translated: intestine of twelve finger-widths (in length), from Latin duodēnum, genitive pl. of duodēnī, twelve each, from duodecim, twelve.[6] The Latin phrase intestīnum duodēnum digitōrum is thought to be a loan-translation from the Greek word dodekadaktylon (δωδεκαδάκτυλον), literally "twelve fingers long." The intestinal section was so called by Greek physician Herophilus (c.335–280 B.C.E.) for its length, about equal to the breadth of 12 fingers.[7]
Structure
The duodenum is a 25–38 cm (12-15 inch) C-shaped structure lying adjacent to the stomach. It is divided anatomically into four sections. The first part of the duodenum lies within the peritoneum but its other parts are retroperitoneal.[8]:273
First part
The first part, or superior part, of the duodenum is a continuation from the pylorus to transpyloric plane. It is superior to the rest of the segments, at the vertebral level of L1. The duodenal bulb about 2 cm long, is the very first part of the duodenum and is slightly dilated. The duodenal bulb is a remnant of the mesoduodenum, a mesentery which suspends the organ from the posterior abdominal wall in fetal life.[9] The first part of the duodenum is mobile, and connected to the liver by the hepatoduodenal ligament of the lesser omentum. The first part of the duodenum ends at the corner, the superior duodenal flexure.[8]:273
Relations:
Second part
The second part, or descending part, of the duodenum begins at the superior duodenal flexure. It goes inferior to the lower border of vertebral body L3, before making a sharp turn medially into the inferior duodenal flexure, the end of the descending part.[8]:274
The pancreatic duct and common bile duct enter the descending duodenum, through the major duodenal papilla. The second part of the duodenum also contains the minor duodenal papilla, the entrance for the accessory pancreatic duct. The junction between the embryological foregut and midgut lies just below the major duodenal papilla.[8]:274
Third part
The third part, or horizontal part or inferior part of the duodenum is 10~12 cm in length. It begins at the inferior duodenal flexure and passes transversely to the left, passing in front of the inferior vena cava, abdominal aorta and the vertebral column. The superior mesenteric artery and vein are anterior to the third part of duodenum.[8]:274 This part may be compressed between the aorta and SMA causing superior mesenteric artery syndrome.
Fourth part
The fourth part, or ascending part, of the duodenum passes upward, joining with the jejunum at the duodenojejunal flexure. The fourth part of the duodenum is at the vertebral level L3, and may pass directly on top, or slightly to the left, of the aorta.[8]:274
Blood supply
The duodenum receives arterial blood from two different sources. The transition between these sources is important as it demarcates the foregut from the midgut. Proximal to the 2nd part of the duodenum (approximately at the major duodenal papilla – where the bile duct enters) the arterial supply is from the gastroduodenal artery and its branch the superior pancreaticoduodenal artery. Distal to this point (the midgut) the arterial supply is from the superior mesenteric artery (SMA), and its branch the inferior pancreaticoduodenal artery supplies the 3rd and 4th sections. The superior and inferior pancreaticoduodenal arteries (from the gastroduodenal artery and SMA respectively) form an anastomotic loop between the celiac trunk and the SMA; so there is potential for collateral circulation here.
The venous drainage of the duodenum follows the arteries. Ultimately these veins drain into the portal system, either directly or indirectly through the splenic or superior mesenteric vein and then to portal vein .
Lymphatic drainage
The lymphatic vessels follow the arteries in a retrograde fashion. The anterior lymphatic vessels drain into the pancreatoduodenal lymph nodes located along the superior and inferior pancreatoduodenal arteries and then into the pyloric lymph nodes (along the gastroduodenal artery). The posterior lymphatic vessels pass posterior to the head of the pancreas and drain into the superior mesenteric lymph nodes. Efferent lymphatic vessels from the duodenal lymph nodes ultimately pass into the celiac lymph nodes.
Histology
Under microscopy, the duodenum has a villous mucosa. This is distinct from the mucosa of the pylorus, which directly joins to the duodenum. Like other structures of the gastrointestinal tract, the duodenum has a mucosa, submucosa, muscularis externa, and adventitia. Glands line the duodenum, known as Brunner's glands, which secrete mucus and bicarbonate in order to neutralise stomach acids. These are distinct glands not found in the ileum or jejunum, the other parts of the small intestine.[10] :274–275
 Dog Duodenum 100X
Dog Duodenum 100X Duodenum with amyloid deposition in lamina propria
Duodenum with amyloid deposition in lamina propria Section of duodenum of cat. X 60
Section of duodenum of cat. X 60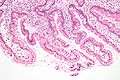
- Duodenum with brush border (microvillus)
Variation
Function
The duodenum is largely responsible for the breakdown of food in the small intestine, using enzymes. The duodenum also regulates the rate of emptying of the stomach via hormonal pathways. Secretin and cholecystokinin are released from cells in the duodenal epithelium in response to acidic and fatty stimuli present there when the pylorus opens and emits gastric chyme into the duodenum for further digestion. These cause the liver and gall bladder to release bile, and the pancreas to release bicarbonate and digestive enzymes such as trypsin, lipase and amylase into the duodenum as they are needed.
The villi of the duodenum have a leafy-looking appearance, which is a histologically identifiable structure. Brunner's glands, which secrete mucus, are found in the duodenum only. The duodenum wall consists of a very thin layer of cells that form the muscularis mucosae.
Gene and protein expression
About 20,000 protein coding genes are expressed in human cells and 70% of these genes are expressed in the normal duodenum.[11][12] Some 300 of these genes are more specifically expressed in the duodenum with very few genes expressed only in the duodenum. The corresponding specific proteins are expressed in the duodenal mucosa, and many of these are also expressed in the small intestine, such as ANPEP, a digestive enzyme, ACE, an enzyme involved in control of blood pressure, and RBP2, a protein involved in the uptake of vitamin A.[13]
Diseases
Ulceration
Ulcers of the duodenum commonly occur because of infection by the bacteria Helicobacter pylori. These bacteria, through a number of mechanisms, erode the protective mucosa of the duodenum, predisposing it to damage from gastric acids. The first part of the duodenum is the most common location of ulcers since it is where the acidic chyme meets the duodenal mucosa before mixing with the alkaline secretions of the duodenum.[14] Duodenal ulcers may cause recurrent abdominal pain and dyspepsia, and are often investigated using a urea breath test to test for the bacteria, and endoscopy to confirm ulceration and take a biopsy. If managed, these are often managed through antibiotics that aim to eradicate the bacteria, and PPIs and antacids to reduce the gastric acidity.[15]
Celiac disease
The British Society of Gastroenterology (BSG) guidelines specify that a duodenal biopsy is required for the diagnosis of adult celiac disease. The biopsy is ideally performed at a moment when the patient is on a gluten-containing diet.[16]
Cancer
Duodenal cancer is a cancer in the first section of the small intestine. Cancer of the duodenum is relatively rare compared to stomach cancer and colorectal cancer. Its histology is usually adenocarcinoma.
Inflammation
Inflammation of the duodenum is referred to as duodenitis. There are multiple known causes.[17]
Additional images
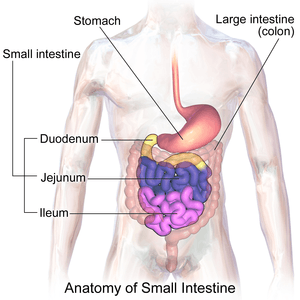 Sections of the small intestine
Sections of the small intestine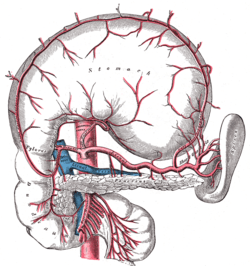 The celiac artery and its branches; the stomach has been raised and the peritoneum removed
The celiac artery and its branches; the stomach has been raised and the peritoneum removed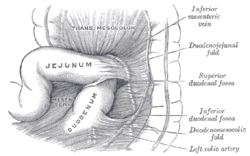 Superior and inferior duodenal fossæ
Superior and inferior duodenal fossæ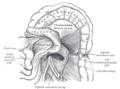 Duodenojejunal fossa
Duodenojejunal fossa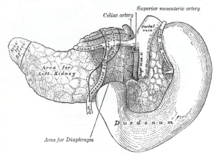 The pancreas and duodenum from behind
The pancreas and duodenum from behind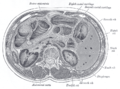 Transverse section through the middle of the first lumbar vertebra, showing the relations of the pancreas
Transverse section through the middle of the first lumbar vertebra, showing the relations of the pancreas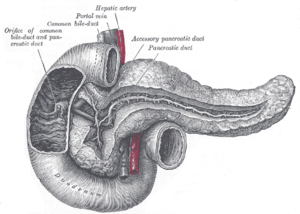 The pancreatic duct
The pancreatic duct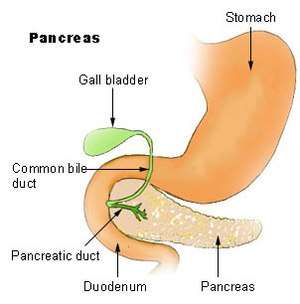 Region of pancreas
Region of pancreas- Duodenum
- Duodenum
- Duodenum
See also
| Wikimedia Commons has media related to Duodenum. |
| Look up duodenum in Wiktionary, the free dictionary. |
Notes
References
- Nosek, Thomas M. Essentials of Human Physiology. Section 6/6ch2/s6ch2_30
- Standring S, Borley NR, eds. (2008). Gray's anatomy : the anatomical basis of clinical practice. Brown JL, Moore LA (40th ed.). London: Churchill Livingstone. pp. 1163, 1177, 1185–6. ISBN 978-0-8089-2371-8.
- Guillaume, Jean; Praxis Publishing; Sadasivam Kaushik; Pierre Bergot; Robert Metailler (2001). Nutrition and Feeding of Fish and Crustaceans. Springer. p. 31. ISBN 978-1-85233-241-9. Retrieved 2009-01-09.
- Latunde-Dada GO; Van der Westhuizen J; Vulpe CD; et al. (2002). "Molecular and functional roles of duodenal cytochrome B (Dcytb) in iron metabolism". Blood Cells Mol. Dis. 29 (3): 356–60. doi:10.1006/bcmd.2002.0574. PMID 12547225.
- van Gijn J; Gijselhart JP (2011). "Treitz and his ligament". Ned. Tijdschr. Geneeskd. 155 (8): A2879. PMID 21557825.
- American Heritage Dictionary, 4th edition
- "duodenum - Origin and meaning of duodenum by Online Etymology Dictionary". www.etymonline.com.
- Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students. Philadelphia: Elsevier/Churchill Livingstone. ISBN 978-0-8089-2306-0.
- Singh, Inderbir; GP Pal (2012). "13". Human Embryology (9 ed.). Delhi: Macmillan Publishers India. p. 163. ISBN 978-93-5059-122-2.
- Deakin, Barbara Young ... [et al.]; drawings by Philip J. (2006). Wheater's functional histology : a text and colour atlas (5th ed.). [Edinburgh?]: Churchill Livingstone/Elsevier. ISBN 978-0-443-06850-8.
- "The human proteome in duodenum - The Human Protein Atlas". www.proteinatlas.org. Retrieved 2017-09-26.
- Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (2015-01-23). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900.
- Gremel, Gabriela; Wanders, Alkwin; Cedernaes, Jonathan; Fagerberg, Linn; Hallström, Björn; Edlund, Karolina; Sjöstedt, Evelina; Uhlén, Mathias; Pontén, Fredrik (2015-01-01). "The human gastrointestinal tract-specific transcriptome and proteome as defined by RNA sequencing and antibody-based profiling". Journal of Gastroenterology. 50 (1): 46–57. doi:10.1007/s00535-014-0958-7. ISSN 0944-1174. PMID 24789573.
- Smith, Margaret E. The Digestive System.
- Britton, the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston; illustrated by Robert (2010). Davidson's principles and practice of medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. pp. 871–874. ISBN 978-0-7020-3085-7.
- Ludvigsson, J. F.; Bai, J. C.; Biagi, F.; Card, T. R.; Ciacci, C.; Ciclitira, P. J.; Green, P. H. R.; Hadjivassiliou, M.; Holdoway, A.; van Heel, D. A.; Kaukinen, K.; Leffler, D. A.; Leonard, J. N.; Lundin, K. E. A.; McGough, N.; Davidson, M.; Murray, J. A.; Swift, G. L.; Walker, M. M.; Zingone, F.; Sanders, D. S. (2014). "Diagnosis and management of adult coeliac disease: Guidelines from the British Society of Gastroenterology". Gut. 63 (8): 1210–1228. doi:10.1136/gutjnl-2013-306578. ISSN 0017-5749. PMC 4112432. PMID 24917550.
- Serra S, Jani PA (2006). "An approach to duodenal biopsies". J. Clin. Pathol. 59 (11): 1133–50. doi:10.1136/jcp.2005.031260. PMC 1860495. PMID 16679353.
External links
| Look up duodenum in Wiktionary, the free dictionary. |
- Duodenum at the Human Protein Atlas
- duodenum at The Anatomy Lesson by Wesley Norman (Georgetown University)