Currarino syndrome
The Currarino syndrome is an inherited congenital disorder where either the sacrum (the fused vertebrae forming the back of the pelvis) is not formed properly, or there is a mass in the presacral space in front of the sacrum, and there are malformations of the anus or rectum. It can also cause an anterior meningocele or a presacral teratoma.
| Currarino syndrome | |
|---|---|
| Other names | Currarino triad |
 | |
| An X-ray showing Imperforate anus | |
Presacral teratoma usually is considered to be a variant of sacrococcygeal teratoma. However, the presacral teratoma that is characteristic of the Currarino syndrome may be a distinct kind.[1]
Genetics
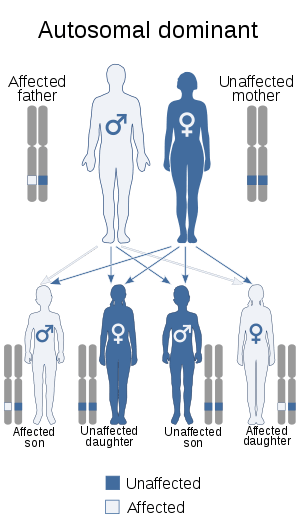
The disorder is an autosomal dominant genetic trait[2] caused by a mutation in the HLXB9 homeobox gene. In 2000 the first large series of Currarino cases was genetically screened for HLXB9 mutations, and it was shown that the gene is specifically causative for the syndrome, but not for other forms of sacral agenesis. The study was published in the American Journal of Human Genetics.[3]
Diagnosis
Treatment
Surgery of an anterior myelomeningocele is not necessarily indicated, only in the rare case in which the space-occupying aspect is expected to cause constipation or problems during pregnancy or delivery. Fistulas between the spinal canal and colon have to be operated on directly.[4]
Importance of early diagnosis and multidisciplinary assessment is recommended to establish adequate treatment if needed.[5][6][7]
By accurate evaluation, the correct surgical management, including neurosurgery, can be performed in a 1-stage approach.[8]
The management of Currarino syndrome is similar to the usual management of anorectal malformation (ARM) regarding the surgical approach and probably the prognosis that mainly depends on degree of associated sacral dysplasia.[9]
The cooperation between pediatric surgeons and neurosurgeons is crucial. The follow-up of these patients should be done in a spina bifida clinic.[10]
Neurosurgeons are involved in the surgical treatment of anterior meningoceles, which are often associated with this condition. The accepted surgical treatment is a anterior or posterior or a staged anterior-posterior resection of the presacral mass and obliteration of the anterior meningocele.[11][12]
The anterior sacral meningocele regresses over time following transdural ligation of its neck.[13]
Posterior approach
A posterior procedure via lumbar and sacral partial laminectomy-laminoplasty and transdural ligation of the neck of the meningocele for anterior sacral meningoceles, or alternatively, tumor excision for other types of presacral lesions.[14][15]
Endoscopic or endoscope-assisted surgery via a posterior sacral route can be feasible for treatment of some of the patients with anterior sacral meningocele. Anterior meningocele pouch associated with Currarino syndrome will regresses over time following transdural ligation of its neck.[16]
Anterior approach
A 40-year-old woman presenting with cauda equina syndrome and ascending meningitis. The meningocele was removed using an anterior abdominal approach. A sigmoid resection was performed with rectal on-table antegrade lavage followed by closure of the rectal fistula, closure of the rectal stump, and proximal colostomy. Closure of the sacral deficit was carried out by suturing a strip of well-vascularized omentum and fibrin glue.
Prompt surgical management using an anterior approach, resection of the sac, closure of the sacral deficit, and fecal diversion resulted in a satisfactory outcome.[17]
See also
References
- Gopal M, Turnpenny PD, Spicer R (June 2007). "Hereditary sacrococcygeal teratoma--not the same as its sporadic counterpart!". Eur J Pediatr Surg. 17 (3): 214–6. doi:10.1055/s-2007-965121. PMID 17638164.
- Ashcraft KW; Holder TM (October 1974). "Hereditary presacral teratoma". J. Pediatr. Surg. 9 (5): 691–7. doi:10.1016/0022-3468(74)90107-9. PMID 4418917.
- Belloni, E; Martucciello, G; Verderio, D; Ponti, E; Seri, M; Jasonni, V; Torre, M; Ferrari, M; Tsui, LC; Scherer, SW (January 2000). "Involvement of the HLXB9 homeobox gene in Currarino syndrome". American Journal of Human Genetics. 66 (1): 312–9. doi:10.1086/302723. PMC 1288336. PMID 10631160.
- Emans PJ, van Aalst J, van Heurn EL, Marcelis C, Kootstra G, Beets-Tan RG, Vles JS, Beuls EA (2006). "The Currarino triad: neurosurgical considerations". Neurosurgery. 58 (5): 924–9, discussion 924–9. doi:10.1227/01.NEU.0000209945.87233.6A. PMID 16639328.CS1 maint: multiple names: authors list (link)
- Berghauser Pont LM, Dirven CM, Dammers R (2012). "Currarino's triad diagnosed in an adult woman". Eur Spine J. 21 Suppl 4: S569–72. doi:10.1007/s00586-012-2311-2. PMC 3369045. PMID 22526704.CS1 maint: multiple names: authors list (link)
- Emoto S, Kaneko M, Murono K, Sasaki K, Otani K, Nishikawa T, Tanaka T, Hata K, Kawai K, Imai H, Saito N, Kobayashi H, Tanaka S, Ikemura M, Ushiku T, Nozawa H (2018). "Surgical management for a huge presacral teratoma and a meningocele in an adult with Currarino triad: a case report". Surg Case Rep. 4 (1): 9. doi:10.1186/s40792-018-0419-2. PMC 5775187. PMID 29352751.CS1 maint: multiple names: authors list (link)
- Samuel M, Hosie G, Holmes K (Dec 2000). "Currarino triad--diagnostic dilemma and a combined surgical approach". J Pediatr Surg. 35 (12): 1790–4. doi:10.1053/jpsu.2000.19258. PMID 11101738.CS1 maint: multiple names: authors list (link)
- Crétolle C, Zérah M, Jaubert F, Sarnacki S, Révillon Y, Lyonnet S, Nihoul-Fékété C (2006). "New clinical and therapeutic perspectives in Currarino syndrome (study of 29 cases)". J Pediatr Surg. 41 (1): 126–31, discussion 126–31. doi:10.1016/j.jpedsurg.2005.10.053. PMID 16410121.CS1 maint: multiple names: authors list (link)
- AbouZeid AA, Mohammad SA, Abolfotoh M, Radwan AB, Ismail MME, Hassan TA (2017). "The Currarino triad: What pediatric surgeons need to know". J Pediatr Surg. 52 (8): 1260–1268. doi:10.1016/j.jpedsurg.2016.12.010. PMID 28065719.CS1 maint: multiple names: authors list (link)
- Serratrice N, Fievet L, Albader F, Scavarda D, Dufour H, Fuentes S (2018). "Multiple neurosurgical treatments for different members of the same family with Currarino syndrome". Neurochirurgie. 64 (3): 211–215. doi:10.1016/j.neuchi.2018.01.009. PMID 29731315.CS1 maint: multiple names: authors list (link)
- Chakhalian D, Gunasekaran A, Gandhi G, Bradley L, Mizell J, Kazemi N (2017). "Multidisciplinary surgical treatment of presacral meningocele and teratoma in an adult with Currarino triad". Surg Neurol Int. 8: 77. doi:10.4103/sni.sni_439_16. PMC 5445655. PMID 28584680.CS1 maint: multiple names: authors list (link)
- Emoto S, Kaneko M, Murono K, Sasaki K, Otani K, Nishikawa T, Tanaka T, Hata K, Kawai K, Imai H, Saito N, Kobayashi H, Tanaka S, Ikemura M, Ushiku T, Nozawa H (2018). "Surgical management for a huge presacral teratoma and a meningocele in an adult with Currarino triad: a case report". Surg Case Rep. 4 (1): 9. doi:10.1186/s40792-018-0419-2. PMC 5775187. PMID 29352751.CS1 maint: multiple names: authors list (link)
- Işik N, Balak N, Kircelli A, Göynümer G, Elmaci I (2008). "The shrinking of an anterior sacral meningocele in time following transdural ligation of its neck in a case of the Currarino triad". Turk Neurosurg. 18 (3): 254–8. PMID 18814114.CS1 maint: multiple names: authors list (link)
- Isik N, Elmaci I, Gokben B, Balak N, Tosyali N (2010). "Currarino triad: surgical management and follow-up results of four [correction of three] cases". Pediatr Neurosurg. 46 (2): 110–9. doi:10.1159/000319007. PMID 20664237.CS1 maint: multiple names: authors list (link)
- Kansal R, Mahore A, Dange N, Kukreja S (2012). "Epidermoid cyst inside anterior sacral meningocele in an adult patient of Currarino syndrome manifesting with meningitis". Turk Neurosurg. 22 (5): 659–61. doi:10.5137/1019-5149.JTN.3985-10.1. PMID 23015348.CS1 maint: multiple names: authors list (link)
- Duru S, Karabagli H, Turkoglu E, Erşahin Y (2014). "Currarino syndrome: report of five consecutive patients". Childs Nerv Syst. 30 (3): 547–52. doi:10.1007/s00381-013-2274-6. PMID 24013264.CS1 maint: multiple names: authors list (link)
- Bergeron E, Roux A, Demers J, Vanier LE, Moore L (2010). "A 40-year-old woman with cauda equina syndrome caused by rectothecal fistula arising from an anterior sacral meningocele". Neurosurgery. 67 (5): E1464–7, discussion E1467–8. doi:10.1227/NEU.0b013e3181f352ba. PMID 20871432.CS1 maint: multiple names: authors list (link)