Colposcopy
Colposcopy (Ancient Greek: κόλπος, romanized: kolpos, lit. 'hollow, womb, vagina' + skopos "look at") is a medical diagnostic procedure to examine an illuminated, magnified view of the cervix as well as the vagina and vulva.[1] Many pre-malignant lesions and malignant lesions in these areas have discernible characteristics that can be detected through the examination. It is done using a colposcope, which provides a magnified view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue and take directed biopsies for further pathological examination. The main goal of colposcopy is to prevent cervical cancer by detecting and treating precancerous lesions early. The procedure was developed by the German physician Hans Hinselmann, with help from Eduard Wirths.[2][3] The development of colposcopy involved experimentation on Jewish inmates from Auschwitz.[4]
- Not to be confused with colonoscopy.
| Colposcopy | |
|---|---|
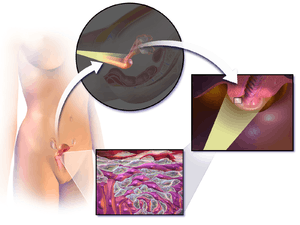
.svg.png) In this diagram, the canal of the cervix (or endocervix) is circled at the base of the womb. The vaginal portion of the cervix projects free into the vagina. The transformation zone, at the opening of the cervix into the vagina, is the area where most abnormal cell changes occur | |
| Specialty | gynecology |
| ICD-9-CM | 67 |
| MeSH | D003127 |
| OPS-301 code | 1-671 |
A specialized colposcope equipped with a camera is used in examining and collecting evidence for victims of rape and sexual assault.
Indications
Most women undergo a colposcopic examination to further investigate a cytological abnormality on their Pap smears. Other indications for a patient to have a colposcopy include:
- assessment of diethylstilbestrol (DES) exposure in utero,
- immunosuppression such as HIV infection, or an organ transplant patient
- an abnormal appearance of the cervix as noted by a primary care provider
- as a part of a sexual assault forensic examination[5] done by a Sexual Assault Nurse Examiner
Many physicians base their current evaluation and treatment decisions on the report "Evidence-Based Consensus Recommendations for Colposcopy Practice for Cervical Cancer Prevention in the United States", developed by the American Society for Colposcopy and Cervical Pathology, most recently in 2017.[6]
Colposcopy is not generally performed for persons treated for cervical cancer if their pap tests show low-grade squamous intraepithelial lesion or less.[7] Unless the person has a visible lesion, colposcopy for this population does not detect a recurrence of cancer.[7]
Procedure

During the initial evaluation, a medical history is obtained, including gravidity (number of prior pregnancies), parity (number of prior deliveries), last menstrual period, contraception use, prior abnormal pap smear results, allergies, significant past medical history, other medications, prior cervical procedures, and smoking history. In some cases, a pregnancy test may be performed before the procedure. The procedure is fully described to the patient, questions are asked and answered, and the patient then signs a consent form.
A colposcope is used to identify visible clues suggestive of abnormal tissue. It functions as a lighted binocular or monocular microscope to magnify the view of the cervix, vagina, and vulvar surface. Low magnification (2× to 6×) may be used to obtain a general impression of the surface architecture. 8x to 25x magnification are utilized to evaluate the vagina and cervix. High magnification together with green filter is often used to identify certain vascular patterns that may indicate the presence of more advanced pre-cancerous or cancerous lesions. Acetic acid solution and iodine solution (Lugol's or Schiller's) are applied to the surface to improve visualization of abnormal areas.
Colposcopy is performed with the woman lying back, legs in stirrups, and buttocks at the lower edge of the table (a position known as the dorsal lithotomy position). A speculum is placed in the vagina after the vulva is examined for any suspicious lesions.
1% or 3% dilute acetic acid is applied to the cervix using cotton swabs. Areas of acetowhiteness correlate with higher nuclear density. The squamocolumar junction, or "transformation zone", is a critical area on the cervix where many precancerous and cancerous lesions most often arise. The ability to see the transformation zone and the entire extent of any lesion visualized determines whether an adequate colposcopic examination is attainable.
Areas of the cervix that turn white after the application of acetic acid or have an abnormal vascular pattern are often considered for biopsy. If no lesions are visible, an iodine solution may be applied to the cervix to help highlight areas of abnormality.
After a complete examination, the colposcopist determines the areas with the highest degree of visible abnormality and may obtain biopsies from these areas using a long biopsy instrument, such as a punch forceps, SpiraBrush CX or SoftBiopsy. Most doctors and patients consider anesthesia unnecessary; however, some colposcopists now recommend and use a topical anesthetic such as lidocaine or a cervical block to decrease patient discomfort, particularly if many biopsy samples are taken.
Following any biopsies, an endocervical curettage (ECC) is often done. The ECC utilizes a long straight curette, a Soft-ECC curette employing fabric to simultaneously collect tissue or a cytobrush (like a small pipe-cleaner) to scrape the inside of the cervical canal. The ECC should never be done on a patient who is pregnant. Monsel's solution is applied with large cotton swabs to the surface of the cervix to control bleeding. This solution looks like mustard and turns black when exposed to blood. After the procedure this material will be expelled naturally: Patients can expect to have a thin coffee-ground like discharge for up to several days after the procedure. Alternatively, some physicians achieve hemostasis with silver nitrate.
Interpretation
One model for scoring colposcopy findings is the Swede Score, which assigns a score between 0 and 2 for 5 different parameters, as given in table below:
| Score | |||
|---|---|---|---|
| 0 | 1 | 2 | |
| Uptake of acetic acid |
0 or transparent | Shady, milky | Distinct, stearin-like |
| Margins and surface | 0 or diffuse | Sharp, but irregular, jagged, "geographical" satellites | Sharp and even, difference in surface level such as "cutting" |
| Vessels | Fine, regular | Absent | Coarse or atypical |
| Lesion size | < 5mm | 5-15mm or spanning 2 quadrants | >15mm or spanning 3-4 quadrants or endocervically undefined |
| Iodine staining | Brown | Faintly or patchy yellow | Distinct yellow |
The total Swede Score ranges between 0 and 10. A score of ≥5 is reported to identify all high-grade lesions (HGL) and ≥8 to have a specificity of 90% for HGL.[8] A score <5 is suggested to not require biopsy because of low risk of cancer, a score 5-7 to require biopsy, and a score ≥8 again not to require biopsy because it is likely more efficient to intervene by e.g. excision directly.[8]
Complications
Significant complications from a colposcopy are not common, but may include bleeding, infection at the biopsy site or endometrium, and failure to identify the lesion. Monsel's solution and silver nitrate interfere with interpretation of biopsy specimens, so these substances should not be applied until all biopsies have been taken. Some patients experience a degree of discomfort during the curettage, and many experience discomfort during the biopsy.
Colposcopy with biopsy does not cause infertility or subfertility.[9]
Follow up
Adequate follow-up is critical to the success of this procedure. Human Papillomavirus (HPV) is a common infection and the underlying cause for most cervical dysplasia. Patients should be counseled on the benefits of safe sex for reducing their risks of contracting and spreading HPV.[10] One study suggests that prostaglandin in semen may fuel the growth of cervical and uterine tumours and that those who are affected may benefit from the use of condoms.[11][12]
Smoking predisposes one to developing cervical abnormalities. A smoking cessation program should be part of the treatment plan for patients who smoke.
Treatments for significant lesions include ablative treatments (cryotherapy, thermocoagulation, and laser ablation) and excisional methods (loop electrosurgical excision procedure or LEEP, or Cervical conization).
References
- Chase DM, Kalouyan M, DiSaia PJ (May 2009). "Colposcopy to evaluate abnormal cervical cytology in 2008". Am. J. Obstet. Gynecol. 200 (5): 472–80. doi:10.1016/j.ajog.2008.12.025. PMID 19375565.
- "The Deadly Origins Of A Life-saving Procedure – Forward.com". Retrieved 2010-01-22.
- Baggish, Michael S. (11 April 2018). Colposcopy of the Cervix, Vagina, and Vulva: A Comprehensive Textbook. Mosby. ISBN 9780323018593. Retrieved 11 April 2018 – via Google Books.
- Halioua, Bruno (2010). "The Participation of Hans Hinselman in Medical Experiments at Auschwitz". Journal of Lower Genital Tract Disease. 14 (1): 1–4. doi:10.1097/LGT.0b013e3181af30ef. PMID 20040829.
- "Archived copy". Archived from the original on 2009-12-22. Retrieved 2010-02-25.CS1 maint: archived copy as title (link)
- Wentzensen, Nicolas; Massad, L. Stewart; Mayeaux, Edward J.; Khan, Michelle J.; Waxman, Alan G.; Einstein, Mark H.; Conageski, Christine; Schiffman, Mark H.; Gold, Michael A.; Apgar, Barbara S.; Chelmow, David; Choma, Kim K.; Darragh, Teresa M.; Gage, Julia C.; Garcia, Francisco A.R.; Guido, Richard S.; Jeronimo, Jose A.; Liu, Angela; Mathews, Cara A.; Mitchell, Martha M.; Moscicki, Anna-Barbara; Novetsky, Akiva P.; Papasozomenos, Theognosia; Perkins, Rebecca B.; Silver, Michelle I.; Smith, Katie M.; Stier, Elizabeth A.; Tedeschi, Candice A.; Werner, Claudia L.; Huh, Warner K. (2017). "Evidence-Based Consensus Recommendations for Colposcopy Practice for Cervical Cancer Prevention in the United States". Journal of Lower Genital Tract Disease. 21 (4): 216–222. doi:10.1097/LGT.0000000000000322. ISSN 1526-0976. PMID 28953109.
- Society of Gynecologic Oncology (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, Society of Gynecologic Oncology, retrieved 19 February 2013, which cites
- Rimel, B. J.; Ferda, A.; Erwin, J.; Dewdney, S. B.; Seamon, L.; Gao, F.; Desimone, C.; Cotney, K. K.; Huh, W.; Massad, L. S. (2011). "Cervicovaginal Cytology in the Detection of Recurrence After Cervical Cancer Treatment". Obstetrics & Gynecology. 118 (3): 548–53. doi:10.1097/AOG.0b013e3182271fdd. PMID 21860282.
- Tergas, A. I.; Havrilesky, L. J.; Fader, A. N.; Guntupalli, S. R.; Huh, W. K.; Massad, L. S.; Rimel, B. J. (2013). "Cost analysis of colposcopy for abnormal cytology in post-treatment surveillance for cervical cancer". Gynecologic Oncology. 130 (3): 421–5. doi:10.1016/j.ygyno.2013.05.037. PMID 23747836.
- Page 91 in: Principles and Practice of Colposcopy. JP Medical Ltd. 2011. ISBN 9789350250945.
- Spracklen, C. N.; Harland, K. K.; Stegmann, B. J.; Saftlas, A. F. (2013). "Cervical surgery for cervical intraepithelial neoplasia and prolonged time to conception of a live birth: A case-control study". BJOG: An International Journal of Obstetrics & Gynaecology. 120 (8): 960–965. doi:10.1111/1471-0528.12209. PMC 3691952. PMID 23489374.
- New England Journal of Medicine Condom Use and the Risk of Genital Human Papillomavirus Infection in Young Women
- "Semen 'may fuel cervical cancer'". BBC. 2006-08-31. Retrieved 2007-12-02.
- "Semen can worsen cervical cancer". Medical Research Council (UK). Archived from the original on 2011-06-15. Retrieved 2007-12-02.
External links
- Colposcopy and Treatment of Cervical Intraepithelial Neoplasia: A Beginner's Manual (IARC Screening Group)
- Atlas of colposcopy – principles and practice (IARC Screening Group)
- American Society for Colposcopy and Cervical Pathology
- Women & Babies Colposcopy and gynaecology procedures undertaken by the Women & Babies Consultants.