Coenzyme Q10
Coenzyme Q, also known as ubiquinone, is a coenzyme family that is ubiquitous in animals and most bacteria (hence the name ubiquinone). In humans, the most common form is Coenzyme Q10 or ubiquinone-10. CoQ10 is not approved by the U.S. Food and Drug Administration (FDA) for the treatment of any medical condition;[1] however, it is sold as a dietary supplement.
 | |
| Names | |
|---|---|
| IUPAC name
2-[(2E,6E,10E,14E,18E,22E,26E,30E,34E)-3,7,11,15,19,23,27,31,35,39-Decamethyltetraconta-2,6,10,14,18,22,26,30,34,38-decaenyl]-5,6-dimethoxy-3-methylcyclohexa-2,5-diene-1,4-dione | |
| Other names
Ubiquinone, ubidecarenone, coenzyme Q, CoQ10 /ˌkoʊˌkjuːˈtɛn/, CoQ, Q10 | |
| Identifiers | |
CAS Number |
|
3D model (JSmol) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| ECHA InfoCard | 100.005.590 |
PubChem CID |
|
| UNII | |
CompTox Dashboard (EPA) |
|
InChI
| |
SMILES
| |
| Properties | |
Chemical formula |
C59H90O4 |
| Molar mass | 863.365 g·mol−1 |
| Appearance | yellow or orange solid |
| Melting point | 48–52 °C (118–126 °F; 321–325 K) |
Solubility in water |
insoluble |
| Pharmacology | |
| C01EB09 (WHO) | |
| Related compounds | |
Related quinones |
1,4-Benzoquinone Plastoquinone Ubiquinol |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
It is a 1,4-benzoquinone, where Q refers to the quinone chemical group and 10 refers to the number of isoprenyl chemical subunits in its tail. In natural ubiquinones, the number can be anywhere from 6 to 10. This family of fat-soluble substances, which resemble vitamins, is present in all respiring eukaryotic cells, primarily in the mitochondria. It is a component of the electron transport chain and participates in aerobic cellular respiration, which generates energy in the form of ATP. Ninety-five percent of the human body's energy is generated this way.[2][3] Organs with the highest energy requirements—such as the heart, liver, and kidney—have the highest CoQ10 concentrations.[4][5][6]
There are three redox states of CoQ: fully oxidized (ubiquinone), semiquinone (ubisemiquinone), and fully reduced (ubiquinol). The capacity of this molecule to act as a two-electron carrier (moving between the quinone and quinol form) and a one-electron carrier (moving between the semiquinone and one of these other forms) is central to its role in the electron transport chain due to the iron–sulfur clusters that can only accept one electron at a time, and as a free-radical–scavenging antioxidant.
Deficiency and toxicity
There are two major factors that lead to deficiency of CoQ10 in humans: reduced biosynthesis, and increased use by the body. Biosynthesis is the major source of CoQ10. Biosynthesis requires at least 12 genes, and mutations in many of them cause CoQ deficiency. CoQ10 levels also may be affected by other genetic defects (such as mutations of mitochondrial DNA, ETFDH, APTX, FXN, and BRAF, genes that are not directly related to the CoQ10 biosynthetic process).
Some adverse effects, largely gastrointestinal, are reported with very high intakes. The observed safe level (OSL) risk assessment method indicated that the evidence of safety is strong at intakes up to 1200 mg/day, and this level is identified as the OSL.[7]
Assessment
Although CoQ10 may be measured in blood plasma, these measurements reflect dietary intake rather than tissue status. Currently, most clinical centers measure CoQ10 levels in cultured skin fibroblasts, muscle biopsies, and blood mononuclear cells.[8] Culture fibroblasts can be used also to evaluate the rate of endogenous CoQ10 biosynthesis, by measuring the uptake of 14C-labelled p-hydroxybenzoate.[9]
Statins
It has been suggested that the myotoxicity of statins is due to impairment of CoQ biosynthesis, but the evidence supporting this was deemed controversial in 2011.[8]
While statins may reduce coenzyme Q10 in the blood it is unclear if they reduce coenzyme Q10 in muscle.[10] Evidence does not support that supplementation improves side effects from statins.[10]
Dietary supplement
Regulation and composition
CoQ10 is sold in many jurisdictions as a dietary supplement, not subject to the same regulations as medicinal drugs, but not approved for the treatment of any medical condition.[1][11] The manufacture of CoQ10 is not regulated, and different batches and brands may vary significantly:[1] a 2004 laboratory analysis by ConsumerLab.com of CoQ10 supplements on sale in the US found that some did not contain the quantity identified on the product label. Amounts ranged from "no detectable CoQ10", through 75% of stated dose, up to a 75% excess.[12]
Generally, CoQ10 is well tolerated. The most common side effects are gastrointestinal symptoms (nausea, vomiting, appetite suppression, and abdominal pain), rashes, and headaches.[13]
While there is no established ideal dosage of CoQ10, a typical daily dose is 100–200 milligrams. Different formulations have varying declared amounts of CoQ10 and other ingredients.[14]
Heart disease
A 2014 Cochrane review found "no convincing evidence to support or refute" the use of CoQ10 for the treatment of heart failure.[15] Another 2014 Cochrane review found insufficient evidence to make a conclusion about its use for the prevention of heart disease.[16] A 2016 Cochrane review concluded that CoQ10 had no effect on blood pressure.[17] In a 2017 meta-analysis of people with heart failure 30–100 mg/d of CoQ10 resulted in 31% lower mortality. Exercise capacity was also increased. No significant difference was found in the endpoints of left heart ejection fraction and New York Heart Association (NYHA) classification.[18]
Migraine headaches
The Canadian Headache Society guideline for migraine prophylaxis recommends, based on low-quality evidence, that 300 mg of CoQ10 be offered as a choice for prophylaxis.[19]
Statin myopathy
CoQ10 has been routinely used to treat muscle breakdown associated as a side effect of use of statin medications. A 2015 meta-analysis of randomized controlled trials found that CoQ10 had no effect on statin myopathy.[20] A 2018 meta-analysis concluded that there was preliminary evidence for oral CoQ10 reducing statin-associated muscle symptoms, including muscle pain, muscle weakness, muscle cramps and muscle tiredness.[21]
Cancer
As of 2014 no large well-designed clinical trials of CoQ10 in cancer treatment had been conducted.[1] The US' National Cancer Institute identified issues with the few, small studies that had been carried out, stating, "the way the studies were done and the amount of information reported made it unclear if benefits were caused by the CoQ10 or by something else".[1] The American Cancer Society concluded, "CoQ10 may reduce the effectiveness of chemo and radiation therapy, so most oncologists would recommend avoiding it during cancer treatment."[22]
Dental disease
A 1995 review study found that there is no clinical benefit to the use of CoQ10 in the treatment of periodontal disease.[23] Most of the studies suggesting otherwise were outdated, focused on in vitro tests,[24][25][26] had too few test subjects and/or erroneous statistical methodology and trial setup,[27][28] or were sponsored by a manufacturer of the product.[29]
Chronic kidney disease
A review of the effects of CoQ10 supplementation in people with CKD was proposed in 2019.[30]
Interactions
Coenzyme Q10 has potential to inhibit the effects of theophylline as well as the anticoagulant warfarin; coenzyme Q10 may interfere with warfarin's actions by interacting with Cytochome p450 enzymes thereby reducing the INR, a measure of blood clotting.[31] The structure of coenzyme Q10 is very similar to that of vitamin K, which competes with and counteracts warfarin's anticoagulation effects. Coenzyme Q10 should be avoided in patients currently taking warfarin due to the increased risk of clotting.[13]
Chemical properties
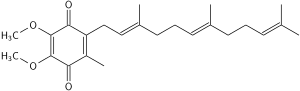
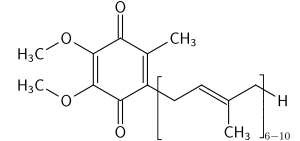
The oxidized structure of CoQ10 is shown on the top-right. The various kinds of Coenzyme Q may be distinguished by the number of isoprenoid subunits in their side-chains. The most common Coenzyme Q in human mitochondria is CoQ10. Q refers to the quinone head and 10 refers to the number of isoprene repeats in the tail. The molecule below has three isoprenoid units and would be called Q3.
Biosynthesis
Biosynthesis occurs in most human tissue. There are three major steps:
- Creation of the benzoquinone structure (using phenylalanine or tyrosine, via 4-hydroxybenzoate)
- Creation of the isoprene side chain (using acetyl-CoA)
- The joining or condensation of the above two structures
The initial two reactions occur in mitochondria, the endoplasmic reticulum, and peroxisomes, indicating multiple sites of synthesis in animal cells.[32]
An important enzyme in this pathway is HMG-CoA reductase, usually a target for intervention in cardiovascular complications. The "statin" family of cholesterol-reducing medications inhibits HMG-CoA reductase. One possible side effect of statins is decreased production of CoQ10, which may be connected to the development of myopathy and rhabdomyolysis. However, the role statin plays in CoQ deficiency is controversial. Although these drug reduce blood levels of CoQ, studies on the effects of muscle levels of CoQ are yet to come. CoQ supplementation also does not reduce side effects of statin medications.[8][10]
Genes involved include PDSS1, PDSS2, COQ2, and ADCK3 (COQ8, CABC1).[33]
Organisms other than human use somewhat different source chemicals to produce the benzoquinone structure and the isoprene structure. For example, the bacteria E. coli produces the former from chorismate and the latter from a non-mevalonate source. The common yeast S. cerevisiae, however, derives the former from either chorismate or tyrosine and the latter from mevalonate. Most organisms share the common 4-hydroxybenzoate intermediate, yet again uses different steps to arrive at the "Q" structure.[34]
Absorption and metabolism
Absorption
CoQ10 is a crystalline powder insoluble in water. Absorption follows the same process as that of lipids; the uptake mechanism appears to be similar to that of vitamin E, another lipid-soluble nutrient. This process in the human body involves secretion into the small intestine of pancreatic enzymes and bile, which facilitates emulsification and micelle formation required for absorption of lipophilic substances.[35] Food intake (and the presence of lipids) stimulates bodily biliary excretion of bile acids and greatly enhances absorption of CoQ10. Exogenous CoQ10 is absorbed from the small intestine and is best absorbed if taken with a meal. Serum concentration of CoQ10 in fed condition is higher than in fasting conditions.[36][37]
Metabolism
Data on the metabolism of CoQ10 in animals and humans are limited.[38] A study with 14C-labeled CoQ10 in rats showed most of the radioactivity in the liver two hours after oral administration when the peak plasma radioactivity was observed, but CoQ9 (with only 9 isoprenyl units) is the predominant form of coenzyme Q in rats.[39] It appears that CoQ10 is metabolised in all tissues, while a major route for its elimination is biliary and fecal excretion. After the withdrawal of CoQ10 supplementation, the levels return to normal within a few days, irrespective of the type of formulation used.[40]
Pharmacokinetics
Some reports have been published on the pharmacokinetics of CoQ10. The plasma peak can be observed 2–6 hours after oral administration, depending mainly on the design of the study. In some studies, a second plasma peak also was observed at approximately 24 hours after administration, probably due to both enterohepatic recycling and redistribution from the liver to circulation.[35] Tomono et al. used deuterium-labeled crystalline CoQ10 to investigate pharmacokinetics in humans and determined an elimination half-time of 33 hours.[41]
Improving the bioavailability of CoQ10
The importance of how drugs are formulated for bioavailability is well known. In order to find a principle to boost the bioavailability of CoQ10 after oral administration, several new approaches have been taken; different formulations and forms have been developed and tested on animals and humans.[38]
Reduction of particle size
Nanoparticles have been explored as a delivery system for various drugs, such as improving the oral bioavailability of drugs with poor absorption characteristics.[42] However, this has not proved successful with CoQ10, although reports have differed widely.[43][44] The use of aqueous suspension of finely powdered CoQ10 in pure water also reveals only a minor effect.[40]
Soft-gel capsules with CoQ10 in oil suspension
A successful approach was to use the emulsion system to facilitate absorption from the gastrointestinal tract and to improve bioavailability. Emulsions of soybean oil (lipid microspheres) could be stabilised very effectively by lecithin and were used in the preparation of soft gelatin capsules. In one of the first such attempts, Ozawa et al. performed a pharmacokinetic study on beagles in which the emulsion of CoQ10 in soybean oil was investigated; about twice the plasma CoQ10 level than that of the control tablet preparation was determined during administration of a lipid microsphere.[40] Although an almost negligible improvement of bioavailability was observed by Kommuru et al. with oil-based softgel capsules in a later study on dogs,[45] the significantly increased bioavailability of CoQ10 was confirmed for several oil-based formulations in most other studies.[46]
Novel forms of CoQ10 with increased water-solubility
Facilitating drug absorption by increasing its solubility in water is a common pharmaceutical strategy and also has been shown to be successful for CoQ10. Various approaches have been developed to achieve this goal, with many of them producing significantly better results over oil-based softgel capsules in spite of the many attempts to optimize their composition.[38] Examples of such approaches are use of the aqueous dispersion of solid CoQ10 with the polymer tyloxapol,[47] formulations based on various solubilising agents, such as hydrogenated lecithin,[48] and complexation with cyclodextrins; among the latter, the complex with β-cyclodextrin has been found to have highly increased bioavailability.[49][50] and also is used in pharmaceutical and food industries for CoQ10-fortification.[38]
History
In 1950, G. N. Festenstein was the first to isolate a small amount of CoQ10 from the lining of a horse's gut at Liverpool, England. In subsequent studies the compound was briefly called substance SA, it was deemed to be quinone and it was noted that it could found from many tissues of a number of animals.[51]
In 1957, Frederick L. Crane and colleagues at the University of Wisconsin–Madison Enzyme Institute isolated the same compound from mitochondrial membranes of beef heart and noted that it transported electrons within mitochondria. They called it Q-275 for short as it was a quinone.[52][51] Soon they noted that Q-275 and substance SA studied in England may be the same compound. This was confirmed later that year and Q-275/substance SA was renamed ubiquinone as it was an ubiquitous quinone that could be found from all animal tissues.[51][53]
In 1958, its full chemical structure was reported by D. E. Wolf and colleagues working under Karl Folkers at Merck in Rahway.[54][51][53] Later that year D. E. Green and colleagues belonging to the Wisconsin research group suggested that ubiquinone should be called either mitoquinone or coenzyme Q due to its participation to the mitochondrial electron transport chain.[51][53]
In 1966, A. Mellors and A. L. Tappel at the University of California were to first to show that reduced CoQ6 was an effective antioxidant in cells.[55][53]
In 1960s Peter D. Mitchell enlarged upon the understanding of mitochondrial function via his theory of electrochemical gradient, which involves CoQ10, and in late 1970s studies of Lars Ernster enlargened upon the importance of CoQ10 as an antioxidant. The 1980s witnessed a steep rise in the number of clinical trials involving CoQ10.[53]
Dietary concentrations
Detailed reviews on occurrence of CoQ10 and dietary intake were published in 2010.[56] Besides the endogenous synthesis within organisms, CoQ10 also is supplied to the organism by various foods. Despite the scientific community's great interest in this compound, however, a very limited number of studies have been performed to determine the contents of CoQ10 in dietary components. The first reports on this aspect were published in 1959, but the sensitivity and selectivity of the analytical methods at that time did not allow reliable analyses, especially for products with low concentrations.[56] Since then, developments in analytical chemistry have enabled a more reliable determination of CoQ10 concentrations in various foods:
CoQ10 levels in selected foods[56] Food CoQ10 concentration (mg/kg) Beef heart 113 liver 39–50 muscle 26–40 Pork heart 12–128 liver 23–54 muscle 14–45 Chicken breast 8–17 thigh 24–25 wing 11 Fish sardine 5–64 mackerel: – red flesh 43–67 – white flesh 11–16 salmon 4–8 tuna 5 Oils soybean 54–280 olive 4–160 grapeseed 64–73 sunflower 4–15 canola 64–73 Nuts peanut 27 walnut 19 sesame seed 18–23 pistachio 20 hazelnut 17 almond 5–14 Vegetables parsley 8–26 broccoli 6–9 cauliflower 2–7 spinach up to 10 Chinese cabbage 2–5 Fruit avocado 10 blackcurrant 3 grape 6–7 strawberry 1 orange 1–2 grapefruit 1 apple 1 banana 1
Meat and fish are the richest sources of dietary CoQ10; levels over 50 mg/kg may be found in beef, pork, and chicken heart and liver. Dairy products are much poorer sources of CoQ10 than animal tissues. Vegetable oils also are quite rich in CoQ10. Within vegetables, parsley and perilla are the richest CoQ10 sources, but significant differences in their CoQ10 levels may be found in the literature. Broccoli, grapes, and cauliflower are modest sources of CoQ10. Most fruit and berries represent a poor to very poor source of CoQ10, with the exception of avocados, which have a relatively high CoQ10 content.[56]
Intake
In the developed world, the estimated daily intake of CoQ10 has been determined at 3–6 mg per day, derived primarily from meat.[56]
Effect of heat and processing
Cooking by frying reduces CoQ10 content by 14–32%.[57]
See also
- Idebenone – synthetic analog with reduced oxidant generating properties
References
- White, J. (14 May 2014). "PDQ® Coenzyme Q10". National Cancer Institute, National Institutes of Health, U.S. Dept. of Health and Human Services. Retrieved 29 June 2014.
- Ernster L, Dallner G (May 1995). "Biochemical, physiological and medical aspects of ubiquinone function". Biochimica et Biophysica Acta. 1271 (1): 195–204. doi:10.1016/0925-4439(95)00028-3. PMID 7599208.
- Dutton, P. L.; Ohnishi, T.; Darrouzet, E.; Leonard, M. A.; Sharp, R. E.; Cibney, B. R.; Daldal, F.; Moser, C. C. (2000). "4 Coenzyme Q oxidation reduction reactions in mitochondrial electron transport". In Kagan, V. E.; Quinn, P. J. (eds.). Coenzyme Q: Molecular mechanisms in health and disease. Boca Raton: CRC Press. pp. 65–82.
- Okamoto T, Matsuya T, Fukunaga Y, Kishi T, Yamagami T (1989). "Human serum ubiquinol-10 levels and relationship to serum lipids". International Journal for Vitamin and Nutrition Research. Internationale Zeitschrift Fur Vitamin- und Ernahrungsforschung. Journal International de Vitaminologie et de Nutrition. 59 (3): 288–92. PMID 2599795.
- Aberg F, Appelkvist EL, Dallner G, Ernster L (June 1992). "Distribution and redox state of ubiquinones in rat and human tissues". Archives of Biochemistry and Biophysics. 295 (2): 230–4. doi:10.1016/0003-9861(92)90511-T. PMID 1586151.
- Shindo Y, Witt E, Han D, Epstein W, Packer L (January 1994). "Enzymic and non-enzymic antioxidants in epidermis and dermis of human skin". The Journal of Investigative Dermatology. 102 (1): 122–4. doi:10.1111/1523-1747.ep12371744. PMID 8288904.
- Hathcock JN, Shao A (August 2006). "Risk assessment for coenzyme Q10 (Ubiquinone)". Regulatory Toxicology and Pharmacology. 45 (3): 282–8. doi:10.1016/j.yrtph.2006.05.006. PMID 16814438.
- Trevisson E, DiMauro S, Navas P, Salviati L (October 2011). "Coenzyme Q deficiency in muscle". Current Opinion in Neurology. 24 (5): 449–56. doi:10.1097/WCO.0b013e32834ab528. hdl:10261/129020. PMID 21844807.
- Montero R, Sánchez-Alcázar JA, Briones P, Hernández AR, Cordero MD, Trevisson E, et al. (June 2008). "Analysis of coenzyme Q10 in muscle and fibroblasts for the diagnosis of CoQ10 deficiency syndromes". Clinical Biochemistry. 41 (9): 697–700. doi:10.1016/j.clinbiochem.2008.03.007. PMID 18387363.
- Tan JT, Barry AR (June 2017). "Coenzyme Q10 supplementation in the management of statin-associated myalgia". American Journal of Health-System Pharmacy. 74 (11): 786–793. doi:10.2146/ajhp160714. PMID 28546301.
- "Mitochondrial disorders in children: Co-enzyme Q10". UK: National Institute for Health and Care Excellence. 28 March 2017.
- "ConsumerLab.com finds discrepancies in strength of CoQ10 supplements". Townsend Letter for Doctors and Patients. August–September 2004. p. 19.
- Wyman M, Leonard M, Morledge T (July 2010). "Coenzyme Q10: a therapy for hypertension and statin-induced myalgia?". Cleveland Clinic Journal of Medicine. 77 (7): 435–42. doi:10.3949/ccjm.77a.09078. PMID 20601617.
- "Benefits of Coenzyme Q10". Benefits of CoQ10. 28 September 2017. Retrieved 28 September 2017.
- Madmani ME, Yusuf Solaiman A, Tamr Agha K, Madmani Y, Shahrour Y, Essali A, Kadro W (June 2014). "Coenzyme Q10 for heart failure". Heart Group. The Cochrane Database of Systematic Reviews (6): CD008684. doi:10.1002/14651858.CD008684.pub2. PMID 24049047.
- Flowers N, Hartley L, Todkill D, Stranges S, Rees K (4 December 2014). "Co-enzyme Q10 supplementation for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 12 (12): CD010405. doi:10.1002/14651858.CD010405.pub2. PMID 25474484.
- Ho MJ, Li EC, Wright JM (March 2016). "Blood pressure lowering efficacy of coenzyme Q10 for primary hypertension". The Cochrane Database of Systematic Reviews. 3 (3): CD007435. doi:10.1002/14651858.CD007435.pub3. PMC 6486033. PMID 26935713.
- Lei L, Liu Y (July 2017). "Efficacy of coenzyme Q10 in patients with cardiac failure: a meta-analysis of clinical trials". BMC Cardiovascular Disorders. 17 (1): 196. doi:10.1186/s12872-017-0628-9. PMC 5525208. PMID 28738783.
- Pringsheim T, Davenport W, Mackie G, Worthington I, Aubé M, Christie SN, et al. (March 2012). "Canadian Headache Society guideline for migraine prophylaxis". The Canadian Journal of Neurological Sciences. 39 (2 Suppl 2): S1–59. PMID 22683887.
- Banach M, Serban C, Sahebkar A, Ursoniu S, Rysz J, Muntner P, et al. (January 2015). "Effects of coenzyme Q10 on statin-induced myopathy: a meta-analysis of randomized controlled trials". Mayo Clinic Proceedings (Systematic Review and Meta-Analysis). Lipid and Blood Pressure Meta-analysis Collaboration Group. 90 (1): 24–34. doi:10.1016/j.mayocp.2014.08.021. PMID 25440725.
- Qu H, Guo M, Chai H, Wang WT, Gao ZY, Shi DZ (October 2018). "Effects of Coenzyme Q10 on Statin-Induced Myopathy: An Updated Meta-Analysis of Randomized Controlled Trials". Journal of the American Heart Association. 7 (19): e009835. doi:10.1161/JAHA.118.009835. PMC 6404871. PMID 30371340.
- "Coenzyme Q10". American Cancer Society.
- Watts TL (March 1995). "Coenzyme Q10 and periodontal treatment: is there any beneficial effect?". British Dental Journal. 178 (6): 209–13. doi:10.1038/sj.bdj.4808715. PMID 7718355.
- Folkers K, Hanioka T, Xia LJ, McRee JT, Langsjoen P (April 1991). "Coenzyme Q10 increases T4/T8 ratios of lymphocytes in ordinary subjects and relevance to patients having the AIDS related complex". Biochemical and Biophysical Research Communications. 176 (2): 786–91. doi:10.1016/S0006-291X(05)80254-2. PMID 1673841.
- Littarru GP, Nakamura R, Ho L, Folkers K, Kuzell WC (October 1971). "Deficiency of coenzyme Q 10 in gingival tissue from patients with periodontal disease". Proceedings of the National Academy of Sciences of the United States of America. 68 (10): 2332–5. Bibcode:1971PNAS...68.2332L. doi:10.1073/pnas.68.10.2332. PMC 389415. PMID 5289867.
- Nakamura R, Littarru GP, Folkers K, Wilkinson EG (April 1974). "Study of CoQ10-enzymes in gingiva from patients with periodontal disease and evidence for a deficiency of coenzyme Q10". Proceedings of the National Academy of Sciences of the United States of America. 71 (4): 1456–60. Bibcode:1974PNAS...71.1456N. doi:10.1073/pnas.71.4.1456. PMC 388248. PMID 4151519.
- McRee, J. T.; Hanioka, T.; Shizukuishi, S.; Folkers, K. (1993). "Therapy with coenzyme Q10 for patients with periodontal disease". Journal of Dental Health. 43 (5): 659–666. doi:10.5834/jdh.43.659.
- Hanioka T, Tanaka M, Ojima M, Shizukuishi S, Folkers K (1994). "Effect of topical application of coenzyme Q10 on adult periodontitis". Molecular Aspects of Medicine. 15 Suppl (Suppl): s241–8. doi:10.1016/0098-2997(94)90034-5. PMID 7752836.
- Wilkinson EG, Arnold RM, Folkers K (August 1976). "Bioenergetics in clinical medicine. VI. adjunctive treatment of periodontal disease with coenzyme Q10". Research Communications in Chemical Pathology and Pharmacology. 14 (4): 715–9. PMID 785563.
- Xu, Yongxing; Liu, Juan; Han, Enhong; Wang, Yan; Gao, Jianjun (2019). "Efficacy of coenzyme Q10 in patients with chronic kidney disease: protocol for a systematic review". BMJ Open. 9 (5): e029053. doi:10.1136/bmjopen-2019-029053. ISSN 2044-6055. PMC 6530451. PMID 31092669.
- Sharma, A; Fonarow, GC; Butler, J; Ezekowitz, JA; Felker, GM (April 2016). "Coenzyme Q10 and Heart Failure: A State-of-the-Art Review". Circulation: Heart Failure. 9 (4): e002639. doi:10.1161/CIRCHEARTFAILURE.115.002639. PMID 27012265.
- Bentinger M, Tekle M, Dallner G (May 2010). "Coenzyme Q--biosynthesis and functions". Biochemical and Biophysical Research Communications. 396 (1): 74–9. doi:10.1016/j.bbrc.2010.02.147. PMID 20494114.
- Espinós, Carmen; Felipo, Vicente; Palau, Francesc (2009). Inherited Neuromuscular Diseases: Translation from Pathomechanisms to Therapies. Springer. pp. 122ff. ISBN 978-90-481-2812-9. Retrieved 4 January 2011.
- Meganathan R (September 2001). "Ubiquinone biosynthesis in microorganisms". FEMS Microbiology Letters. 203 (2): 131–9. doi:10.1111/j.1574-6968.2001.tb10831.x. PMID 11583838.
- Bhagavan HN, Chopra RK (May 2006). "Coenzyme Q10: absorption, tissue uptake, metabolism and pharmacokinetics". Free Radical Research. 40 (5): 445–53. doi:10.1080/10715760600617843. PMID 16551570.
- Bogentoft 1991
- Ochiai A, Itagaki S, Kurokawa T, Kobayashi M, Hirano T, Iseki K (August 2007). "Improvement in intestinal coenzyme q10 absorption by food intake". Yakugaku Zasshi. 127 (8): 1251–4. doi:10.1248/yakushi.127.1251. PMID 17666877.
- Žmitek; et al. (2008). "Improving the bioavailability of CoQ10". Agro Food Industry Hi Tech. 19 (4): 9. Archived from the original on 5 October 2011. Retrieved 21 October 2008.
- Kishi, H.; Kanamori, N.; Nisii, S.; Hiraoka, E.; Okamoto, T.; Kishi, T. (1964). "Metabolism and Exogenous Coenzyme Q10 in vivo and Bioavailability of Coenzyme Q10 Preparations in Japan". Biomedical and Clinical Aspects of Coenzyme Q. Amsterdam: Elsevier. pp. 131–142.
- Ozawa Y, Mizushima Y, Koyama I, Akimoto M, Yamagata Y, Hayashi H, Murayama H (April 1986). "Intestinal absorption enhancement of coenzyme Q10 with a lipid microsphere". Arzneimittel-Forschung. 36 (4): 689–90. PMID 3718593.
- Tomono Y, Hasegawa J, Seki T, Motegi K, Morishita N (October 1986). "Pharmacokinetic study of deuterium-labelled coenzyme Q10 in man". International Journal of Clinical Pharmacology, Therapy, and Toxicology. 24 (10): 536–41. PMID 3781673.
- Mathiowitz E, Jacob JS, Jong YS, Carino GP, Chickering DE, Chaturvedi P, et al. (March 1997). "Biologically erodable microspheres as potential oral drug delivery systems". Nature. 386 (6623): 410–4. Bibcode:1997Natur.386..410M. doi:10.1038/386410a0. PMID 9121559.
- Hsu CH, Cui Z, Mumper RJ, Jay M (2003). "Preparation and characterization of novel coenzyme Q10 nanoparticles engineered from microemulsion precursors". AAPS PharmSciTech. 4 (3): E32. doi:10.1208/pt040332. PMC 2750625. PMID 14621964.
- Joshi SS, Sawant SV, Shedge A, Halpner AD (January 2003). "Comparative bioavailability of two novel coenzyme Q10 preparations in humans". International Journal of Clinical Pharmacology and Therapeutics. 41 (1): 42–8. doi:10.5414/CPP41042. PMID 12564745.
- Kommuru TR, Ashraf M, Khan MA, Reddy IK (July 1999). "Stability and bioequivalence studies of two marketed formulations of coenzyme Q10 in beagle dogs". Chemical & Pharmaceutical Bulletin. 47 (7): 1024–8. doi:10.1248/cpb.47.1024. PMID 10434405.
- Bhagavan HN, Chopra RK (June 2007). "Plasma coenzyme Q10 response to oral ingestion of coenzyme Q10 formulations". Mitochondrion. 7 Suppl (Suppl): S78–88. doi:10.1016/j.mito.2007.03.003. PMID 17482886.
- US 6197349, Westesen, K. & B. Siekmann, "Particles with modified physicochemical properties, their preparation and uses", published 2001
- US 4483873, Ohashi, H.; T. Takami & N. Koyama et al., "Aqueous solution containing ubidecarenone", published 1984
- Zmitek J, Smidovnik A, Fir M, Prosek M, Zmitek K, Walczak J, Pravst I (2008). "Relative bioavailability of two forms of a novel water-soluble coenzyme Q10". Annals of Nutrition & Metabolism. 52 (4): 281–7. doi:10.1159/000129661. PMID 18645245.
- Kagan, Daniel; Madhavi, Doddabele (2010). "A Study on the Bioavailability of a Novel Sustained-Release Coenzyme Q10-β-Cyclodextrin Complex". Integrative Medicine. 9 (1).
- Morton RA (December 1958). "Ubiquinone". Nature. 182 (4652): 1764–7. Bibcode:1958Natur.182.1764M. doi:10.1038/1821764a0. PMID 13622652.
- Crane FL, Hatefi Y, Lester RL, Widmer C (July 1957). "Isolation of a quinone from beef heart mitochondria". Biochimica et Biophysica Acta. 25 (1): 220–1. doi:10.1016/0006-3002(57)90457-2. PMID 13445756.
- Boreková M, et al. (2008). "Nourishing and health benefits of coenzyme Q10". Czech Journal of Food Sciences. 26 (4): 229–241. doi:10.17221/1122-cjfs.
- Wolf DE, et al. (1958). "Coenzyme Q. I. structure studies on the coenzyme Q group". Journal of the American Chemical Society. 80 (17): 4752. doi:10.1021/ja01550a096. ISSN 0002-7863.
- Mellors A, Tappel AL (July 1966). "Quinones and quinols as inhibitors of lipid peroxidation". Lipids. 1 (4): 282–4. doi:10.1007/BF02531617. PMID 17805631.
- Pravst I, Zmitek K, Zmitek J (April 2010). "Coenzyme Q10 contents in foods and fortification strategies". Critical Reviews in Food Science and Nutrition. 50 (4): 269–80. doi:10.1080/10408390902773037. PMID 20301015.
- Weber C, Bysted A, Hłlmer G (1997). "The coenzyme Q10 content of the average Danish diet". International Journal for Vitamin and Nutrition Research. Internationale Zeitschrift Fur Vitamin- und Ernahrungsforschung. Journal International de Vitaminologie et de Nutrition. 67 (2): 123–9. PMID 9129255.
External links
- "List of USP Verified CoQ10 Ingredients". U.S. Pharmacopeial Convention. Archived from the original on 9 February 2009.
- "Coenzyme Q10". National Cancer Institute. 23 September 2005.
- Bonakdar, Robert Alan; Guarneri, Erminia (15 September 2005). "Coenzyme Q10". American Family Physician. 72 (6): 1065–1070.