Clofazimine
Clofazimine, sold under the brand name Lamprene, is a medication used together with rifampicin and dapsone to treat leprosy.[1] It is specifically used for multibacillary (MB) leprosy and erythema nodosum leprosum.[2] Evidence is insufficient to support its use in other conditions.[1] It is taken by mouth.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lamprene |
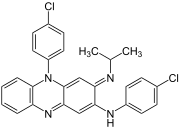
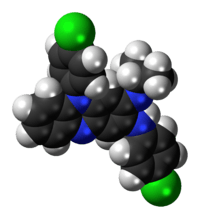
| Other names | N,5-bis(4-chlorophenyl)-3-(1-methylethylimino)-5H-phenazin-2-amine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682128 |
| ATC code | |
| Pharmacokinetic data | |
| Elimination half-life | 70 days |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| ECHA InfoCard | 100.016.347 |
| Chemical and physical data | |
| Formula | C27H22Cl2N4 |
| Molar mass | 473.396 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 210 to 212 °C (410 to 414 °F) |
SMILES
| |
InChI
| |
| | |
Common side effects include abdominal pain, diarrhea, itchiness, dry skin, and change in color of the skin.[1] May also cause swelling of the lining of the gastrointestinal tract, increased blood sugar, and sensitivity to the sun.[2] It is unclear if use during pregnancy is safe.[1] Clofazimine is a phenazine dye and believed to work by interfering with DNA.[1]
Clofazimine was discovered in the 1950s at Trinity College, Dublin,[3] and approved for medical use in the United States in 1986.[1] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[4] The wholesale cost in the developing world is about US$24 per month.[5] In the United States it is not available commercially but can be obtained from the US Department of Health and Human Services.[1]
Medical uses
The primary use of clofazimine is for the treatment of leprosy.[1] Other uses have not been proven to be safe or effective.[1]
It has been studied in combination with other antimycobacterial drugs to treat Mycobacterium avium infections in people with HIV/AIDS and Mycobacterium avium paratuberculosis. Clofazimine also has a marked anti-inflammatory effect and is given to control the leprosy reaction, erythema nodosum leprosum (ENL). (From AMA Drug Evaluations Annual, 1993, p1619). The drug is given as an alternative to people who can not tolerate the effects of dapsone for leprosy.[6]
Side effects
Clofazimine produces pink to brownish skin pigmentation in 75-100% of patients within a few weeks, as well as similar discoloration of most bodily fluids and secretions. These discolorations are reversible but may take months to years to disappear. There is evidence in medical literature that as a result of clofazimine administration, several patients have developed depression which in some cases resulted in suicide. It has been hypothesized that the depression was a result of this chronic skin discoloration.[7]
Cases of icthyosis and skin dryness are also reported in response to this drug (8%-28%), as well as rash and itchiness (1-5%).
40-50% of patients develop gastrointestinal intolerance. Rarely, patients have died from bowel obstructions and intestinal bleeding, or required abdominal surgery to correct the same problem.
Mechanism
Clofazimine works by binding to the guanine bases of bacterial DNA, thereby blocking the template function of the DNA and inhibiting bacterial proliferation.[8][9] It also increases activity of bacterial phospholipase A2, leading to release and accumulation of lysophospholipids,[8][9] which are toxic and inhibit bacterial proliferation.[10][11]
Clofazimine is also a FIASMA (functional inhibitor of acid sphingomyelinase).[12]
Metabolism
Clofazimine has a biological half life of about 70 days. Autopsies performed on those who have died while on clofazimine show crystal-like aggregates in the intestinal mucosa, liver, spleen, and lymph nodes.[13]
History
Clofazimine, initially known as B663, was first synthesised in 1954 by a team of scientists at Trinity College, Dublin: Frank Winder, J.G. Belton, Stanley McElhinney, M.L. Conalty, Seán O'Sullivan, and Dermot Twomey, led by Vincent Barry. Clofazimine was originally intended as an anti-tuberculosis drug but drug proved ineffective. In 1959, a researcher named Y. T. Chang identified its effectiveness against leprosy. After clinical trials in Nigeria and elsewhere during the 1960s, Swiss pharmaceutical company Novartis launched the product in 1969 under the brand name Lamprene.
Novartis was granted FDA approval of clofazimine in December 1986 as an orphan drug. The drug is currently no longer commercially available in the United States.[14]
Society and culture
Clofazimine is marketed under the trade name Lamprene by Novartis. One producer of the clofazimine molecule is Sangrose Laboratories, located in Mavelikara, India.
Research
The immunosuppressive effects of clofazimine were immediately noticed when applied in animal model. Macrophages were first reported to be inhibited due to the stabilization of lysosomal membrane by clofazimine.[15] Clofazimine also showed a dosage-dependent inhibition of neutrophil motility, lymphocyte transformation,[16] mitogen-induced PBMC proliferation[17] and complement-mediated solubilization of pre-formed immune complexes in vitro.[18] A mechanistic studying of clofazimine in human T cells revealed that this drug is a Kv1.3 (KCNA3) channel blocker.[19] This indicates that clofazimine will be potentially used for treatment of multiple sclerosis, rheumatoid arthritis and type 1 diabetes. Because the Kv1.3-high effector memory T cells (TEM) are actively involved in the development of these diseases,[20] and Kv1.3 activity is essential for stimulation and proliferation of TEM by regulating calcium influx in the T cells.[21] Several clinical trials were also conducted looking for its immunosuppressive activity even before it was approved for leprosy by FDA. It was first reported to be effective in treating chronic discoid lupus erythematosus with 17 out of 26 patients got remission.[22] But later another group found it was ineffective in treating diffuse, photosensitive, systemic lupus erythematosus.[23] Clofazimine also has been sporadically reported with some success in other autoimmune diseases such as psoriasis,[24] Miescher's granulomatous cheilitis.[25]
References
- "Clofazimine". The American Society of Health-System Pharmacists. Archived from the original on 20 December 2016. Retrieved 8 December 2016.
- WHO Model Formulary 2008 (PDF). World Health Organization. 2009. p. 132. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- Greenwood, David (2008). Antimicrobial Drugs: Chronicle of a Twentieth Century Medical Triumph. OUP Oxford. p. 200. ISBN 9780199534845.
By 1954 related molecules known as iminophenazines were being investigated... one of the first ones to be made, originally given the laboratory code B663 ... B663—subsequently called clofazimine
- "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- "Clofazimine". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- Clinical Microbiology Made Ridiculously Simple
- Brown, Stoudemire (1998). Psychiatric Side Effects of Prescription and Over-the-counter Medications: Recognition and Management. American Psychiatric Pub. ISBN 9780880488686. Archived from the original on 2016-03-05.
- Arbiser JL, Moschella SL (Feb 1995). "Clofazimine: a review of its medical uses and mechanisms of action". J Am Acad Dermatol. 32 (2 Pt 1): 241–7. doi:10.1016/0190-9622(95)90134-5. PMID 7829710.
- Morrison N. E.; Morley G. M. (1976). "The mode of action of clofazimine: DNA binding studies". Int. J. Lepr. 44: 133–135.
- Dennis, E. A. 1983. Phospholipases, p. 307-353. In P. D. Boyer (ed.), The enzymes, 3rd ed., vol. 16. Lipid enzymology. Academic Press, Inc., New York.
- Kagan V. E. (1989). "Tocopherol stabilizes membrane against phospholipase A, free fatty acids and lysophospholipids". Ann. N.Y. Acad. Sci. 570: 121–135. doi:10.1111/j.1749-6632.1989.tb14913.x. PMID 2698101.
- Kornhuber J, Muehlbacher M, Trapp S, Pechmann S, Friedl A, Reichel M, Mühle C, Terfloth L, Groemer T, Spitzer G, Liedl K, Gulbins E, Tripal P (2011). "Identification of novel functional inhibitors of acid sphingomyelinase". PLOS ONE. 6 (8): e23852. doi:10.1371/journal.pone.0023852. PMC 3166082. PMID 21909365.
- Baik, J.; Rosania, G. R. (2011-07-29). "Molecular Imaging of Intracellular Drug–Membrane Aggregate Formation". Molecular Pharmaceutics. 8 (5): 1742–1749. doi:10.1021/mp200101b. PMC 3185106. PMID 21800872.
- "Lamprene (clofazimine) dosing, indications, interactions, adverse effects, and more". Archived from the original on 2014-07-09. Retrieved 2014-06-13.
- Conalty ML, Barry VC, Jina A (Apr 1971). "The antileprosy agent B.663 (Clofazimine) and the reticuloendothelial system". Int J Lepr Other Mycobact Dis. 39 (2): 479–92. PMID 4948088.
- Gatner EM, Anderson R, van Remsburg CE, Imkamp FM (Jun 1982). "The in vitro and in vivo effects of clofazimine on the motility of neutrophils and transformation of lymphocytes from normal individuals". Lepr Rev. 53 (2): 85–90. PMID 7098757.
- van Rensburg CE, Gatner EM, Imkamp FM, Anderson R (May 1982). "Effects of clofazimine alone or combined with dapsone on neutrophil and lymphocyte functions in normal individuals and patients with lepromatous leprosy". Antimicrob. Agents Chemother. 21 (5): 693–7. doi:10.1128/aac.21.5.693. PMC 181995. PMID 7049077.
- Kashyap A, Sehgal VN, Sahu A, Saha K (Feb 1992). "Anti-leprosy drugs inhibit the complement-mediated solubilization of pre-formed immune complexes in vitro". Int J Immunopharmacol. 14 (2): 269–73. doi:10.1016/0192-0561(92)90039-N. PMID 1624226.
- Ren YR, Pan F, Parvez S, Fleig A, Chong CR, Xu J, Dang Y, Zhang J, Jiang H, Penner R, Liu JO (Dec 2008). "Clofazimine inhibits human Kv1.3 potassium channel by perturbing calcium oscillation in T lymphocytes". PLOS ONE. 3 (12): e4009. doi:10.1371/journal.pone.0004009. PMC 2602975. PMID 19104661.
- Beeton C, Wulff H, Standifer NE, Azam P, Mullen KM, Pennington MW, Kolski-Andreaco A, Wei E, Grino A, Counts DR, Wang PH, LeeHealey CJ, S Andrews B, Sankaranarayanan A, Homerick D, Roeck WW, Tehranzadeh J, Stanhope KL, Zimin P, Havel PJ, Griffey S, Knaus HG, Nepom GT, Gutman GA, Calabresi PA, Chandy KG (Nov 2006). "Kv1.3 channels are a therapeutic target for T cell-mediated autoimmune diseases". Proc Natl Acad Sci U S A. 103 (46): 17414–9. doi:10.1073/pnas.0605136103. PMC 1859943. PMID 17088564.
- Wulff H, Calabresi PA, Allie R, Yun S, Pennington M, Beeton C, Chandy KG (2003). "The voltage-gated Kv1.3 K(+) channel in effector memory T cells as new target for MS". J Clin Invest. 111 (11): 1703–13. doi:10.1172/JCI16921. PMC 156104. PMID 12782673.
- Mackey JP, Barnes J (Jul 1974). "Clofazimine in the treatment of discoid lupus erythematosus". Br J Dermatol. 91 (1): 93–6. doi:10.1111/j.1365-2133.1974.tb06723.x. PMID 4851057.
- Jakes JT, Dubois EL, Quismorio FP Jr (Nov 1982). "Antileprosy drugs and lupus erythematosus". Ann Intern Med. 97 (5): 788. doi:10.7326/0003-4819-97-5-788_2. PMID 7137755.
- Chuaprapaisilp T, Piamphongsant T (Sep 1978). "Treatment of pustular psoriasis with clofazimine". Br J Dermatol. 99 (3): 303–5. doi:10.1111/j.1365-2133.1978.tb02001.x. PMID 708598.
- Podmore P, Burrows D (Mar 1986). "Clofazimine--an effective treatment for Melkersson-Rosenthal syndrome or Miescher's cheilitis". Clin Exp Dermatol. 11 (2): 173–8. doi:10.1111/j.1365-2230.1986.tb00443.x. PMID 3720016.