Cyanosis
Cyanosis is the bluish or purplish discolouration of the skin or mucous membranes due to the tissues near the skin surface having low oxygen saturation.[1] Based on Lundsgaard and Van Slyke's work,[2] it is classically described as occurring if 5.0 g/dL of deoxyhemoglobin or greater is present.[3] This was based on an estimate of capillary saturation based on a mean of arterial versus peripheral venous blood gas measurements.[4] Since estimation of hypoxia is usually now based either on arterial blood gas measurement or pulse oximetry, this is probably an overestimate, with evidence that levels of 2.0 g/dL of deoxyhemoglobin may reliably produce cyanosis.[5] Since, however, the presence of cyanosis is dependent upon there being an absolute quantity of deoxyhemoglobin, the bluish color is more readily apparent in those with high hemoglobin counts than it is with those with anemia. Also, the bluer the color, the more difficult it is to detect on deeply pigmented skin. When signs of cyanosis first appear, such as on the lips or fingers, intervention should be made within 3–5 minutes because a severe hypoxia or severe circulatory failure may have induced the cyanosis.
| Cyanosis | |
|---|---|
| Cyanosis of the hand of a patient with low oxygen saturations | |
| Specialty | Pulmonology, cardiology |
| Types | Central, peripheral |
The name cyanosis literally means the blue disease or the blue condition. It is derived from the color cyan, which comes from cyanós (κυανός), the Greek word for blue.[6]
Definition

Cyanosis is defined as a bluish discoloration, especially of the skin and mucous membranes, due to excessive concentration of deoxyhemoglobin in the blood caused by deoxygenation.
Cyanosis is divided into two main types: central (around the core, lips, and tongue) and peripheral (only the extremities or fingers).
Forms and causes
Central cyanosis
Central cyanosis is often due to a circulatory or ventilatory problem that leads to poor blood oxygenation in the lungs. It develops when arterial oxygen saturation drops below 85% or 75%.
Acute cyanosis can be as a result of asphyxiation or choking, and is one of the definite signs that respiration is being blocked.
Central cyanosis may be due to the following causes:
1. Central nervous system (impairing normal ventilation):
- Intracranial hemorrhage
- Drug overdose (e.g. heroin)
- Tonic–clonic seizure (e.g. grand mal seizure)
- Pneumonia
- Bronchiolitis
- Bronchospasm (e.g. asthma)
- Pulmonary hypertension
- Pulmonary embolism
- Hypoventilation
- Chronic obstructive pulmonary disease, or COPD (emphysema)
- Congenital heart disease (e.g. Tetralogy of Fallot, right to left shunts in heart or great vessels)
- Heart failure
- Valvular heart disease
- Myocardial infarction
4. Blood:
- Methemoglobinemia * Note this causes "spurious" cyanosis, in that, since methemoglobin appears blue,[7] the patient can appear cyanosed even in the presence of a normal arterial oxygen level.
- Polycythaemia
- Congenital cyanosis (HbM Boston) arises from a mutation in the α-codon which results in a change of primary sequence, H → Y. Tyrosine stabilises the Fe(III) form (oxyhaemoglobin) creating a permanent T-state of Hb.
5. Others:
- High altitude, cyanosis may develop in ascents to altitudes >2400 m.
- Hypothermia
- Obstructive sleep apnea
Peripheral cyanosis
Peripheral cyanosis is the blue tint in fingers or extremities, due to an inadequate or obstructed circulation. The blood reaching the extremities is not oxygen-rich and when viewed through the skin a combination of factors can lead to the appearance of a blue color. All factors contributing to central cyanosis can also cause peripheral symptoms to appear but peripheral cyanosis can be observed in the absence of heart or lung failures. Small blood vessels may be restricted and can be treated by increasing the normal oxygenation level of the blood.
Peripheral cyanosis may be due to the following causes:
- All common causes of central cyanosis
- Reduced cardiac output (e.g. heart failure or hypovolaemia)
- Cold exposure
- Chronic obstructive pulmonary disease (COPD)
- Arterial obstruction (e.g. peripheral vascular disease, Raynaud phenomenon)
- Venous obstruction (e.g. deep vein thrombosis)
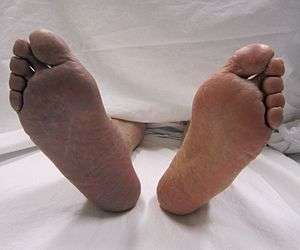
Differential cyanosis
Differential cyanosis is the bluish coloration of the lower but not the upper extremity and the head. This is seen in patients with a patent ductus arteriosus. Patients with a large ductus develop progressive pulmonary vascular disease, and pressure overload of the right ventricle occurs. As soon as pulmonary pressure exceeds aortic pressure, shunt reversal (right-to-left shunt) occurs. The upper extremity remains pink because the brachiocephalic trunk, left common carotid trunk and the left subclavian trunk is given off proximal to the PDA.
Approach to diagnosis
- Inquire about duration (cyanosis since birth suggests congenital heart disease) and exposures (drugs or chemicals that result in abnormal hemoglobins).
- Differentiate central from peripheral cyanosis.
- Check for nail clubbing: Combination of clubbing and cyanosis suggests congenital heart disease and occasionally pulmonary disease.
- If cyanosis is localized to an extremity, evaluate for peripheral vascular obstruction.
- Evaluate abnormal hemoglobins by hemoglobin electrophoresis, spectroscopy and measurement of methemoglobin level.[8]
See also
- Acrocyanosis
- Blue baby syndrome
- Raynaud's phenomenon
- Blue Fugates
References
- Adeyinka, Adebayo; Kondamudi, Noah P. (2019-03-24). "Cyanosis". NCBI Bookshelf. PMID 29489181. Retrieved 2019-05-12.
- Lundsgaard C, Van Slyke DD. Cyanosis. Medicine. 2(1):1-76.
- Mini Oxford Handbook of Clinical Medicine (7th ed.). p. 56.
- Cyanosis. Lundsgaard C, Van SD, Abbott ME. Cyanosis. Can Med Assoc J 1923 Aug;13(8):601-4.
- Goss GA, Hayes JA, Burdon JG. Deoxyhaemoglobin concentrations in the detection of central cyanosis. Thorax 1988 Mar;43(3):212–13.
- Mosby's Medical, Nursing & Allied Health Dictionary. Mosby-Year Book (4th ed.). 1994. p. 425.
- Methemoglobin
- Anthony S. Fauci; et al. (2009). Harrison's manual of medicine (17th ed.). New York: McGraw-Hill Medical. ISBN 9780071477437.
External links
| Classification | |
|---|---|
| External resources |