Pneumonia
Pneumonia is an inflammatory condition of the lung affecting primarily the small air sacs known as alveoli.[4][13] Typically symptoms include some combination of productive or dry cough, chest pain, fever, and trouble breathing.[2] Severity is variable.[2]
| Pneumonia | |
|---|---|
| Other names | Pneumonitis, bronchopneumonia[1] |
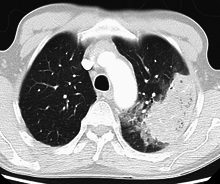
 | |
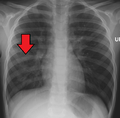
| Chest X-ray of a pneumonia caused by influenza and Haemophilus influenzae, with patchy consolidations, mainly in the right upper lobe (arrow). | |
| Pronunciation |
|
| Specialty | Pulmonology, Infectious disease |
| Symptoms | Cough, difficulty breathing, rapid breathing, fever[2] |
| Duration | Few weeks[3] |
| Causes | Bacteria, virus, aspiration[4][5] |
| Risk factors | Cystic fibrosis, COPD, asthma, diabetes, heart failure, history of smoking[6] |
| Diagnostic method | Based on symptoms, chest X-ray[7] |
| Differential diagnosis | COPD, asthma, pulmonary edema, pulmonary embolism[8] |
| Prevention | Vaccines, handwashing, not smoking[9] |
| Medication | Antibiotics, antivirals, oxygen therapy[10][11] |
| Frequency | 450 million (7%) per year[11][12] |
| Deaths | Four million per year[11][12] |
Pneumonia is usually caused by infection with viruses or bacteria and less commonly by other microorganisms, certain medications and conditions such as autoimmune diseases.[4][5] Risk factors include cystic fibrosis, chronic obstructive pulmonary disease (COPD), asthma, diabetes, heart failure, a history of smoking, a poor ability to cough such as following a stroke, and a weak immune system.[6] Diagnosis is often based on the symptoms and physical examination.[7] Chest X-ray, blood tests, and culture of the sputum may help confirm the diagnosis.[7] The disease may be classified by where it was acquired with community, hospital, or health care associated pneumonia.[14]
Vaccines to prevent certain types of pneumonia are available.[9] Other methods of prevention include handwashing and not smoking.[9] Treatment depends on the underlying cause.[15] Pneumonia believed to be due to bacteria is treated with antibiotics.[10] If the pneumonia is severe, the affected person is generally hospitalized.[15] Oxygen therapy may be used if oxygen levels are low.[10]
Pneumonia affects approximately 450 million people globally (7% of the population) and results in about four million deaths per year.[11][12] Pneumonia was regarded by William Osler in the 19th century as "the captain of the men of death".[16] With the introduction of antibiotics and vaccines in the 20th century, survival improved.[11] Nevertheless, in developing countries, and among the very old, the very young, and the chronically ill, pneumonia remains a leading cause of death.[11][17] Pneumonia often shortens suffering among those already close to death and has thus been called "the old man's friend".[18]
Signs and symptoms
| Symptoms frequency[19] | |
|---|---|
| Symptom | Frequency |
| Cough | 79–91% |
| Fatigue | 90% |
| Fever | 71–75% |
| Shortness of breath | 67–75% |
| Sputum | 60–65% |
| Chest pain | 39–49% |
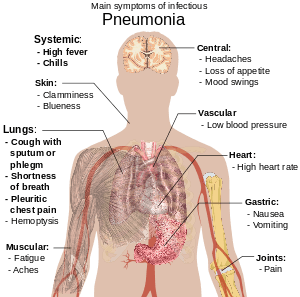
People with infectious pneumonia often have a productive cough, fever accompanied by shaking chills, shortness of breath, sharp or stabbing chest pain during deep breaths, and an increased rate of breathing.[8] In elderly people, confusion may be the most prominent sign.[8]
The typical signs and symptoms in children under five are fever, cough, and fast or difficult breathing.[20] Fever is not very specific, as it occurs in many other common illnesses and may be absent in those with severe disease, malnutrition or in the elderly. In addition, a cough is frequently absent in children less than 2 months old.[20] More severe signs and symptoms in children may include blue-tinged skin, unwillingness to drink, convulsions, ongoing vomiting, extremes of temperature, or a decreased level of consciousness.[20][21]
Bacterial and viral cases of pneumonia usually result in similar symptoms.[22] Some causes are associated with classic, but non-specific, clinical characteristics. Pneumonia caused by Legionella may occur with abdominal pain, diarrhea, or confusion.[23] Pneumonia caused by Streptococcus pneumoniae is associated with rusty colored sputum.[24] Pneumonia caused by Klebsiella may have bloody sputum often described as "currant jelly".[19] Bloody sputum (known as hemoptysis) may also occur with tuberculosis, Gram-negative pneumonia, lung abscesses and more commonly acute bronchitis.[21] Pneumonia caused by Mycoplasma pneumoniae may occur in association with swelling of the lymph nodes in the neck, joint pain, or a middle ear infection.[21] Viral pneumonia presents more commonly with wheezing than bacterial pneumonia.[22] Pneumonia was historically divided into "typical" and "atypical" based on the belief that the presentation predicted the underlying cause.[25] However, evidence has not supported this distinction, therefore it is no longer emphasized.[25]
Cause
Pneumonia is due to infections caused primarily by bacteria or viruses and less commonly by fungi and parasites. Although there are over 100 strains of infectious agents identified, only a few are responsible for the majority of the cases. Mixed infections with both viruses and bacteria may occur in roughly 45% of infections in children and 15% of infections in adults.[11] A causative agent may not be isolated in approximately half of cases despite careful testing.[18]
The term pneumonia is sometimes more broadly applied to any condition resulting in inflammation of the lungs (caused for example by autoimmune diseases, chemical burns or drug reactions); however, this inflammation is more accurately referred to as pneumonitis.[26][27]
Factors that predispose to pneumonia include smoking, immunodeficiency, alcoholism, chronic obstructive pulmonary disease, asthma, chronic kidney disease, liver disease, and old age.[21][28] Additional risk in children include not being breastfeed, exposure to cigarettes or air pollution, malnutrition, and poverty.[29] The use of acid-suppressing medications – such as proton-pump inhibitors or H2 blockers – is associated with an increased risk of pneumonia.[30] Approximately 10% of people who require mechanical ventilation develop ventilator associated pneumonia,[31] and people with gastric feeding tube have an increased risk of developing of aspiration pneumonia.[32] For people with specific variants of FER gene, the risk of death is reduced in sepsis caused by pneumonia. However, for those with TLR6 variants, the risk of getting Legionnaires' disease is increased.[33]
Bacteria
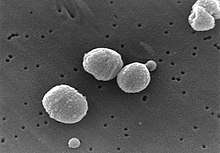
Bacteria are the most-common cause of community-acquired pneumonia (CAP), with Streptococcus pneumoniae isolated in nearly 50% of cases.[34][35] Other commonly-isolated bacteria include Haemophilus influenzae in 20%, Chlamydophila pneumoniae in 13%, and Mycoplasma pneumoniae in 3% of cases;[34] Staphylococcus aureus; Moraxella catarrhalis; Legionella pneumophila; and Gram-negative bacilli.[18] A number of drug-resistant versions of the above infections are becoming more common, including drug-resistant Streptococcus pneumoniae (DRSP) and methicillin-resistant Staphylococcus aureus (MRSA).[21]
The spreading of organisms is facilitated when risk factors are present.[18] Alcoholism is associated with Streptococcus pneumoniae, anaerobic organisms, and Mycobacterium tuberculosis; smoking facilitates the effects of Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Legionella pneumophila. Exposure to birds is associated with Chlamydia psittaci; farm animals with Coxiella burnetti; aspiration of stomach contents with anaerobic organisms; and cystic fibrosis with Pseudomonas aeruginosa and Staphylococcus aureus.[18] Streptococcus pneumoniae is more common in the winter,[18] and it should be suspected in persons aspirating a large amount of anaerobic organisms.[21]
Viruses
In adults, viruses account for approximately a third[11] and in children for about 15% of pneumonia cases.[36] Commonly-implicated agents include rhinoviruses, coronaviruses, influenza virus, respiratory syncytial virus (RSV), adenovirus, and parainfluenza.[11][37] Herpes simplex virus rarely causes pneumonia, except in groups such as: newborns, persons with cancer, transplant recipients, and people with significant burns.[38] People following organ transplantation or those otherwise-immunocompromised present high rates of cytomegalovirus pneumonia.[36][38] Those with viral infections may be secondarily infected with the bacteria Streptococcus pneumoniae, Staphylococcus aureus, or Haemophilus influenzae, particularly when other health problems are present.[21][36] Different viruses predominate at different periods of the year; during flu season, for example, influenza may account for over half of all viral cases.[36] Outbreaks of other viruses also occasionally occur, including hantaviruses and coronavirus.[36]
Fungi
Fungal pneumonia is uncommon, but occurs more commonly in individuals with weakened immune systems due to AIDS, immunosuppressive drugs, or other medical problems.[18][39] It is most often caused by Histoplasma capsulatum, blastomyces, Cryptococcus neoformans, Pneumocystis jiroveci (pneumocystis pneumonia, or PCP), and Coccidioides immitis. Histoplasmosis is most common in the Mississippi River basin, and coccidioidomycosis is most common in the Southwestern United States.[18] The number of cases has been increasing in the later half of the 20th century due to increasing travel and rates of immunosuppression in the population.[39] For people infected with HIV/AIDS, PCP is a common opportunistic infection.[40]
Parasites
A variety of parasites can affect the lungs, including Toxoplasma gondii, Strongyloides stercoralis, Ascaris lumbricoides, and Plasmodium malariae.[41] These organisms typically enter the body through direct contact with the skin, ingestion, or via an insect vector.[41] Except for Paragonimus westermani, most parasites do not affect specifically the lungs but involve the lungs secondarily to other sites.[41] Some parasites, in particular those belonging to the Ascaris and Strongyloides genera, stimulate a strong eosinophilic reaction, which may result in eosinophilic pneumonia.[41] In other infections, such as malaria, lung involvement is due primarily to cytokine-induced systemic inflammation.[41] In the developed world these infections are most common in people returning from travel or in immigrants.[41] Around the world, these infections are most common in the immunodeficient.[42]
Noninfectious
Idiopathic interstitial pneumonia or noninfectious pneumonia[43] is a class of diffuse lung diseases. They include diffuse alveolar damage, organizing pneumonia, nonspecific interstitial pneumonia, lymphocytic interstitial pneumonia, desquamative interstitial pneumonia, respiratory bronchiolitis interstitial lung disease, and usual interstitial pneumonia.[44] Lipoid pneumonia is another rare cause due to lipids entering the lung.[45] These lipids can either be inhaled or from lipids within the body.[45]
Mechanisms
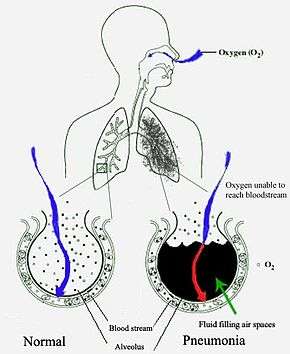
Pneumonia frequently starts as an upper respiratory tract infection that moves into the lower respiratory tract.[46] It is a type of pneumonitis (lung inflammation).[47] The normal flora of the upper airway gives protection by competing with pathogens for nutrients. In the lower airways, reflexes of the glottis, actions of complement proteins and immunoglobulins are important for protection. Microaspiration of contaminated secretions can infect the lower airways and cause pneumonia. The virulence of the organism, amount of the organisms to start an infection and body immune response against the infection all determines the progress of pneumonia.[33]
Bacterial
Most bacteria enter the lungs via small aspirations of organisms residing in the throat or nose.[21] Half of normal people have these small aspirations during sleep.[25] While the throat always contains bacteria, potentially infectious ones reside there only at certain times and under certain conditions.[25] A minority of types of bacteria such as Mycobacterium tuberculosis and Legionella pneumophila reach the lungs via contaminated airborne droplets.[21] Bacteria can spread also via the blood.[22] Once in the lungs, bacteria may invade the spaces between cells and between alveoli, where the macrophages and neutrophils (defensive white blood cells) attempt to inactivate the bacteria.[48] The neutrophils also release cytokines, causing a general activation of the immune system.[49] This leads to the fever, chills, and fatigue common in bacterial pneumonia.[49] The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli, resulting in the consolidation seen on chest X-ray.[50]
Viral
Viruses may reach the lung by a number of different routes. Respiratory syncytial virus is typically contracted when people touch contaminated objects and then they touch their eyes or nose.[36] Other viral infections occur when contaminated airborne droplets are inhaled through the mouth or nose.[21] Once in the upper airway, the viruses may make their way in the lungs, where they invade the cells lining the airways, alveoli, or lung parenchyma.[36] Some viruses such as measles and herpes simplex may reach the lungs via the blood.[51] The invasion of the lungs may lead to varying degrees of cell death.[36] When the immune system responds to the infection, even more lung damage may occur.[36] Primarily white blood cells, mainly mononuclear cells, generate the inflammation.[51] As well as damaging the lungs, many viruses simultaneously affect other organs and thus disrupt other body functions. Viruses also make the body more susceptible to bacterial infections; in this way, bacterial pneumonia can occur at the same time as viral pneumonia.[37]
Diagnosis
Pneumonia is typically diagnosed based on a combination of physical signs and a chest X-ray.[52] In adults with normal vital signs and a normal lung examination the diagnosis is unlikely.[53] However, the underlying cause can be difficult to confirm, as there is no definitive test able to distinguish between bacterial and non-bacterial origin.[11][52] The overall impression of a physician appears to be at least as good as decision rules for making or excluding the diagnosis.[54]
The World Health Organization has defined pneumonia in children clinically based on either a cough or difficulty breathing and a rapid respiratory rate, chest indrawing, or a decreased level of consciousness.[55] A rapid respiratory rate is defined as greater than 60 breaths per minute in children under 2 months old, greater than 50 breaths per minute in children 2 months to 1 year old, or greater than 40 breaths per minute in children 1 to 5 years old.[55] In children, low oxygen levels and lower chest indrawing are more sensitive than hearing chest crackles with a stethoscope or increased respiratory rate.[56] Grunting and nasal flaring may be other useful signs in children less than five years old.[57] Lack of wheezing is an indicator of Mycoplasma pneumoniae in children with pneumonia, but as an indicator it is not accurate enough to decide whether or not macrolide treatment should be used.[58] The presence of chest pain in children with pneumonia doubles the probability of Mycoplasma pneumoniae.[58]
In general, in adults, investigations are not needed in mild cases.[59] There is a very low risk of pneumonia if all vital signs and auscultation are normal.[60] In persons requiring hospitalization, pulse oximetry, chest radiography and blood tests – including a complete blood count, serum electrolytes, C-reactive protein level, and possibly liver function tests – are recommended.[59] Procalcitonin may help determine the cause and support who should receive antibiotics.[61] Antibiotics is encouraged if procalcitonin level reaches 0.25 μg/L, strongly encouraged if it reaches 0.5 μg/L, and strongly discouraged if the level is below 0.10 μg/L.[33] For those with CRP less than 20 mg/L without convincing evidence of pneumonia, antibiotics are not recommended.[33]
The diagnosis of influenza-like illness can be made based on the signs and symptoms; however, confirmation of an influenza infection requires testing.[62] Thus, treatment is frequently based on the presence of influenza in the community or a rapid influenza test.[62]
Physical exam
Physical examination may sometimes reveal low blood pressure, high heart rate, or low oxygen saturation.[21] The respiratory rate may be faster than normal, and this may occur a day or two before other signs.[21][25] Examination of the chest may be normal, but it may show decreased chest expansion on the affected side. Harsh breath sounds from the larger airways that are transmitted through the inflamed lung are termed bronchial breathing and are heard on auscultation with a stethoscope.[21] Crackles (rales) may be heard over the affected area during inspiration.[21] Percussion may be dulled over the affected lung, and increased, rather than decreased, vocal resonance distinguishes pneumonia from a pleural effusion.[8]
Imaging


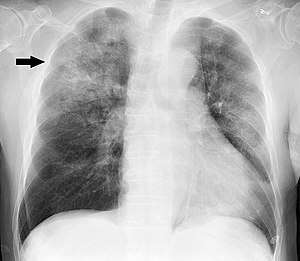
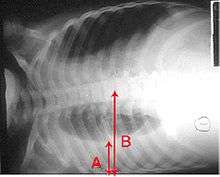
A chest radiograph is frequently used in diagnosis.[20] In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain.[20][59] If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended.[59] Findings do not always match the severity of disease and do not reliably separate between bacterial infection and viral infection.[20]
X-ray presentations of pneumonia may be classified as lobar pneumonia, bronchopneumonia (also known as lobular pneumonia), and interstitial pneumonia.[63] Bacterial, community-acquired pneumonia classically show lung consolidation of one lung segmental lobe, which is known as lobar pneumonia.[34] However, findings may vary, and other patterns are common in other types of pneumonia.[34] Aspiration pneumonia may present with bilateral opacities primarily in the bases of the lungs and on the right side.[34] Radiographs of viral pneumonia may appear normal, appear hyper-inflated, have bilateral patchy areas, or present similar to bacterial pneumonia with lobar consolidation.[34] Radiologic findings may not be present in the early stages of the disease, especially in the presence of dehydration, or may be difficult to be interpreted in the obese or those with a history of lung disease.[21] Complications such as pleural effusion may also be found on chest radiographs. Laterolateral chest radiograph can increase the diagnostic accuracy of lung consolidation and pleural effusion.[33] A CT scan can give additional information in indeterminate cases.[34] CT scan can also provide more details in those with an unclear chest radiograph (for example occult pneumonia in chronic obstructive pulmonary disease) and is able to exclude pulmonary embolism and fungal pneumonia and detecting lung abscess in those who are not responding to treatments.[33] However, CT scan is more expensive, has a higher dose of radiation, and cannot be done at bedside.[33]
Lung ultrasound may also be useful in helping to make the diagnosis.[64] Ultrasound is radiation free and can be done at bedside. However, ultrasound requires specific skills to operate the machine and interpret the findings.[33] It may be more accurate than chest X-ray.[65]
Microbiology
In people managed in the community, determining the causative agent is not cost-effective and typically does not alter management.[20] For people who do not respond to treatment, sputum culture should be considered, and culture for Mycobacterium tuberculosis should be carried out in persons with a chronic productive cough.[59] Microbiological evaluation is also indicated in severe pneumonia, alcoholism, asplenia, immunosuppression, HIV infection, and those being empirically treated for MRSA of pseudomonas.[33][67] Although positive blood culture and pleural fluid culture definitively establish the diagnosis of the type of micro-organism involved, a positive sputum culture has to be interpreted with care for the possibility of colonisation of respiratory tract.[33] Testing for other specific organisms may be recommended during outbreaks, for public health reasons.[59] In those hospitalized for severe disease, both sputum and blood cultures are recommended,[59] as well as testing the urine for antigens to Legionella and Streptococcus.[68] Viral infections, can be confirmed via detection of either the virus or its antigens with culture or polymerase chain reaction (PCR), among other techniques.[11] Mycoplasma, Legionella, Streptococcus, and Chlamydia can also be detected using PCR techniques on bronchoalveolar lavage and nasopharyngeal swab.[33] The causative agent is determined in only 15% of cases with routine microbiological tests.[8]
Classification
Pneumonitis refers to lung inflammation; pneumonia refers to pneumonitis, usually due to infection but sometimes non-infectious, that has the additional feature of pulmonary consolidation.[69] Pneumonia is most commonly classified by where or how it was acquired: community-acquired, aspiration, healthcare-associated, hospital-acquired, and ventilator-associated pneumonia.[34] It may also be classified by the area of lung affected: lobar pneumonia, bronchial pneumonia and acute interstitial pneumonia;[34] or by the causative organism.[70] Pneumonia in children may additionally be classified based on signs and symptoms as non-severe, severe, or very severe.[71]
The setting in which pneumonia develops is important to treatment,[72][73] as it correlates to which pathogens are likely suspects,[72] which mechanisms are likely, which antibiotics are likely to work or fail,[72] and which complications can be expected based on the person's health status.
Community
Community-acquired pneumonia (CAP) is acquired in the community,[72][73] outside of health care facilities. Compared with health care–associated pneumonia, it is less likely to involve multidrug-resistant bacteria. Although the latter are no longer rare in CAP,[72] they are still less likely.
Healthcare
Health care–associated pneumonia (HCAP) is an infection associated with recent exposure to the health care system,[72] including hospital, outpatient clinic, nursing home, dialysis center, chemotherapy treatment, or home care.[73] HCAP is sometimes called MCAP (medical care–associated pneumonia).
Hospital
Hospital-acquired pneumonia is acquired in a hospital, specifically, pneumonia that occurs 48 hours or more after admission, which was not incubating at the time of admission.[73][72] It is likely to involve hospital-acquired infections, with higher risk of multidrug-resistant pathogens. Also, because hospital people are often ill (which is why they are present in the hospital), accompanying disorders are an issue.
Ventilator
Ventilator-associated pneumonia occurs in people breathing with the help of mechanical ventilation.[72][31] Ventilator-associated pneumonia is specifically defined as pneumonia that arises more than 48 to 72 hours after endotracheal intubation.[73]
Differential diagnosis
Several diseases can present with similar signs and symptoms to pneumonia, such as: chronic obstructive pulmonary disease, asthma, pulmonary edema, bronchiectasis, lung cancer, and pulmonary emboli.[8] Unlike pneumonia, asthma and COPD typically present with wheezing, pulmonary edema presents with an abnormal electrocardiogram, cancer and bronchiectasis present with a cough of longer duration, and pulmonary emboli presents with acute onset sharp chest pain and shortness of breath.[8] Mild pneumonia should be differentiated from upper respiratory tract infection (URTI). Severe pneumonia should be differentiated from acute heart failure. Pulmonary infiltrates that resolved after giving mechanical ventilation should point to heart failure and atelectasis rather than pneumonia. For recurrent pneumonia, underlying lung cancer, metastasis, tuberculosis, foreign body, immunosuppression, and hypersensitivity should be sought after.[33]
Prevention
Prevention includes vaccination, environmental measures and appropriate treatment of other health problems.[20] It is believed that, if appropriate preventive measures were instituted globally, mortality among children could be reduced by 400,000; and, if proper treatment were universally available, childhood deaths could be decreased by another 600,000.[22]
Vaccination
Vaccination prevents against certain bacterial and viral pneumonias both in children and adults. Influenza vaccines are modestly effective at preventing symptoms of influenza,[11][74] The Center for Disease Control and Prevention (CDC) recommends yearly influenza vaccination for every person 6 months and older.[75] Immunizing health care workers decreases the risk of viral pneumonia among their people.[68]
Vaccinations against Haemophilus influenzae and Streptococcus pneumoniae have good evidence to support their use.[46] There is strong evidence for vaccinating children under the age of 2 against Streptococcus pneumoniae (pneumococcal conjugate vaccine).[76][77][78] Vaccinating children against Streptococcus pneumoniae has led to a decreased rate of these infections in adults, because many adults acquire infections from children. A Streptococcus pneumoniae vaccine is available for adults, and has been found to decrease the risk of invasive pneumococcal disease by 74%, but there is insufficient evidence to suggest using the pneumococcal vaccine to prevent pneumonia or death in the general adult population.[79] The CDC recommends that young children and adults over the age of 65 receive the pneumococcal vaccine, as well as older children or younger adults who have an increased risk of getting pneumococcal disease.[78] The pneumococcal vaccine has been shown to reduce the risk of community acquired pneumonia in people with chronic obstructive pulmonary disease, but does not reduce mortality or the risk of hospitalization for people with this condition.[80] People with COPD are suggested to have a pneumococcal vaccination.[80] Other vaccines for which there is support for a protective effect against pneumonia include pertussis, varicella, and measles.[81]
Medications
When influenza outbreaks occur, medications such as amantadine or rimantadine may help prevent the condition; however are associated with side effects.[82] Zanamivir or oseltamivir decrease the chance that people who are exposed to the virus will develop symptoms; however, it is recommended that potential side effects are taken into account.[83]
Other
Smoking cessation[59] and reducing indoor air pollution, such as that from cooking indoors with wood or dung, are both recommended.[20][22] Smoking appears to be the single biggest risk factor for pneumococcal pneumonia in otherwise-healthy adults.[68] Hand hygiene and coughing into one's sleeve may also be effective preventative measures.[81] Wearing surgical masks by the sick may also prevent illness.[68]
Appropriately treating underlying illnesses (such as HIV/AIDS, diabetes mellitus, and malnutrition) can decrease the risk of pneumonia.[22][81][84] In children less than 6 months of age, exclusive breast feeding reduces both the risk and severity of disease.[22] In those with HIV/AIDS and a CD4 count of less than 200 cells/uL the antibiotic trimethoprim/sulfamethoxazole decreases the risk of Pneumocystis pneumonia[85] and is also useful for prevention in those that are immunocomprised but do not have HIV.[86]
Testing pregnant women for Group B Streptococcus and Chlamydia trachomatis, and administering antibiotic treatment, if needed, reduces rates of pneumonia in infants;[87][88] preventive measures for HIV transmission from mother to child may also be efficient.[89] Suctioning the mouth and throat of infants with meconium-stained amniotic fluid has not been found to reduce the rate of aspiration pneumonia and may cause potential harm,[90] thus this practice is not recommended in the majority of situations.[90] In the frail elderly good oral health care may lower the risk of aspiration pneumonia.[91] Zinc supplementation in children 2 months to five years old appears to reduce rates of pneumonia.[92]
For people with low levels of vitamin C in their diet or blood, taking vitamin C supplements may be suggested to decrease the risk of pneumonia, although there is no strong evidence of benefit.[93] There is insufficient evidence to recommend that the general population take vitamin C to prevent pneumonia.[93]
For adults and children in the hospital who require a respirator, there is no strong evidence indicating a difference between heat and moisture exchangers and heated humidifiers for preventing pneumonia.[94] There is no good evidence that one approach to mouth care is better than others in preventing nursing home acquired pneumonia.[95]
Management
| CURB-65 | |
|---|---|
| Symptom | Points |
| Confusion | 1 |
| Urea>7 mmol/l | 1 |
| Respiratory rate>30 | 1 |
| SBP<90mmHg, DBP<60mmHg | 1 |
| Age>=65 | 1 |
Antibiotics by mouth, rest, simple analgesics, and fluids usually suffice for complete resolution.[59] However, those with other medical conditions, the elderly, or those with significant trouble breathing may require more advanced care. If the symptoms worsen, the pneumonia does not improve with home treatment, or complications occur, hospitalization may be required.[59] Worldwide, approximately 7–13% of cases in children result in hospitalization,[20] whereas in the developed world between 22 and 42% of adults with community-acquired pneumonia are admitted.[59] The CURB-65 score is useful for determining the need for admission in adults.[59] If the score is 0 or 1, people can typically be managed at home; if it is 2, a short hospital stay or close follow-up is needed; if it is 3–5, hospitalization is recommended.[59] In children those with respiratory distress or oxygen saturations of less than 90% should be hospitalized.[96] The utility of chest physiotherapy in pneumonia has not yet been determined.[97][98] Over-the-counter cough medicine has not been found to be effective,[99] nor has the use of zinc in children.[100] There is insufficient evidence for mucolytics.[99] There is no strong evidence to recommend that children who have non-measles related pneumonia take vitamin A supplements.[101] Vitamin D, as of 2018 is of unclear benefit in children.[102]
Pneumonia can cause severe illness in a number of ways, and pneumonia with evidence of organ dysfunction may require intensive care unit admission for observation and specific treatment.[103] The main impact is on the respiratory and the circulatory system. Respiratory failure not responding to normal oxygen therapy may require heated humidified high-flow therapy delivered through nasal cannulae,[103] non-invasive ventilation,[104] or in severe cases invasive ventilation through an endotracheal tube.[103] With regards to circulatory problems as part of sepsis, evidence of poor blood flow or low blood pressure is initially treated with 30 ml/kg of crystalloid infused intravenously.[33] In situations where fluids alone are ineffective, vasopressor medication may be required.[103]
Bacterial
Antibiotics improve outcomes in those with bacterial pneumonia.[12] First dose of antibiotics should be given as soon as possible.[33] Increased use of antibiotics, however, may lead to the development of antimicrobial resistant strains of bacteria.[105] Antibiotic choice depends initially on the characteristics of the person affected, such as age, underlying health, and the location the infection was acquired. Antibiotic use is also associated with side effects such as nausea, diarrhea, dizziness, taste distortion, or headaches.[105] In the UK, treatment before culture results with amoxicillin is recommended as the first line for community-acquired pneumonia, with doxycycline or clarithromycin as alternatives.[59] In North America, amoxicillin, doxycycline, and in some areas a macrolides (such as azithromycin or erythromycin) is first-line outpatient treatment in adults.[35][106][67] In children with mild or moderate symptoms, amoxicillin taken by mouth is the first line.[96][107][108] The use of fluoroquinolones in uncomplicated cases is discouraged due to concerns about side-effects and generating resistance in light of there being no greater benefit.[35][109]
For those who require hospitalization and caught their pneumonia in the community the use of a β-lactam such as cephazolin plus macrolide such as azithromycin is recommended.[110][67] A fluoroquinolone may replace azithromycin but is less preferred.[67] Antibiotics by mouth and by injection appear to be similarly effective in children with severe pneumonia.[111]
The duration of treatment has traditionally been seven to ten days, but increasing evidence suggests that shorter courses (3–5 days) may be effective for certain types of pneumonia and may reduce the risk of antibiotic resistance.[112][113][114][115] For pneumonia that is associated with a ventilator caused by non-fermenting Gram-negative bacilli (NF-GNB), a shorter course of antibiotics increases the risk of that pneumonia will return.[114] Recommendations for hospital-acquired pneumonia include third- and fourth-generation cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, and vancomycin.[73] These antibiotics are often given intravenously and used in combination.[73] In those treated in hospital, more than 90% improve with the initial antibiotics.[25] For people with ventilator-acquired pneumonia, the choice of antibiotic therapy will depend on the person's risk of being infected with a strain of bacteria that is multi-drug resistant.[31] Once clinically stable, intravenous antibiotics should be switched to oral antibiotics.[33] For those with Methicillin resistant Staphylococcus aureus (MRSA) or Legionella infections, prolonged antibiotics may be beneficial.[33]
The addition of corticosteroids to standard antibiotic treatment appears to improve outcomes, reducing death and morbidity for adults with severe community acquired pneumonia, and reducing death for adults and children with non-severe community acquired pneumonia.[116][117] Side effects associated with the use of corticosteroids include high blood sugar.[116] A 2017 review therefore recommended them in adults with severe community acquired pneumonia.[116] A 2019 guideline however recommended against there general use, unless refractory shock was present.[67] There is some evidence that adding corticosteroids to the standard PCP pneumonia treatment may be beneficial for people who are infected with HIV.[40]
The use of granulocyte colony stimulating factor (G-CSF) along with antibiotics does not appear to reduce mortality and routine use for treating pneumonia is not supported by evidence.[118]
Viral
Neuraminidase inhibitors may be used to treat viral pneumonia caused by influenza viruses (influenza A and influenza B).[11] No specific antiviral medications are recommended for other types of community acquired viral pneumonias including SARS coronavirus, adenovirus, hantavirus, and parainfluenza virus.[11] Influenza A may be treated with rimantadine or amantadine, while influenza A or B may be treated with oseltamivir, zanamivir or peramivir.[11] These are of most benefit if they are started within 48 hours of the onset of symptoms.[11] Many strains of H5N1 influenza A, also known as avian influenza or "bird flu", have shown resistance to rimantadine and amantadine.[11] The use of antibiotics in viral pneumonia is recommended by some experts, as it is impossible to rule out a complicating bacterial infection.[11] The British Thoracic Society recommends that antibiotics be withheld in those with mild disease.[11] The use of corticosteroids is controversial.[11]
Aspiration
In general, aspiration pneumonitis is treated conservatively with antibiotics indicated only for aspiration pneumonia.[119] The choice of antibiotic will depend on several factors, including the suspected causative organism and whether pneumonia was acquired in the community or developed in a hospital setting. Common options include clindamycin, a combination of a beta-lactam antibiotic and metronidazole, or an aminoglycoside.[120] Corticosteroids are sometimes used in aspiration pneumonia, but there is limited evidence to support their effectiveness.[119]
Prognosis
With treatment, most types of bacterial pneumonia will stabilize in 3–6 days.[3] It often takes a few weeks before most symptoms resolve.[3] X-ray finding typically clear within four weeks and mortality is low (less than 1%).[21][122] In the elderly or people with other lung problems, recovery may take more than 12 weeks. In persons requiring hospitalization, mortality may be as high as 10%, and in those requiring intensive care it may reach 30–50%.[21] Pneumonia is the most common hospital-acquired infection that causes death.[25] Before the advent of antibiotics, mortality was typically 30% in those that were hospitalized.[18] However, for those whose lung condition deteriorates within 72 hours, the problem is usually due to sepsis.[33] If pneumonia deteriorates after 72 hours, it could be due to nosocomial infection or excerbation of other underlying co-morbidities.[33] About 10% of those discharged from hospital are readmitted due to underlying co-morbidities such as heart, lung, or neurology disorders, or due to new onset of pneumonia.[33]
Complications may occur in particular in the elderly and those with underlying health problems.[122] This may include, among others: empyema, lung abscess, bronchiolitis obliterans, acute respiratory distress syndrome, sepsis, and worsening of underlying health problems.[122]
Clinical prediction rules
Clinical prediction rules have been developed to more objectively predict outcomes of pneumonia.[25] These rules are often used in deciding whether or not to hospitalize the person.[25]
- Pneumonia severity index (or PSI Score)[25]
- CURB-65 score, which takes into account the severity of symptoms, any underlying diseases, and age[123]
Pleural effusion, empyema, and abscess
In pneumonia, a collection of fluid may form in the space that surrounds the lung.[124] Occasionally, microorganisms will infect this fluid, causing an empyema.[124] To distinguish an empyema from the more common simple parapneumonic effusion, the fluid may be collected with a needle (thoracentesis), and examined.[124] If this shows evidence of empyema, complete drainage of the fluid is necessary, often requiring a drainage catheter.[124] In severe cases of empyema, surgery may be needed.[124] If the infected fluid is not drained, the infection may persist, because antibiotics do not penetrate well into the pleural cavity. If the fluid is sterile, it must be drained only if it is causing symptoms or remains unresolved.[124]
In rare circumstances, bacteria in the lung will form a pocket of infected fluid called a lung abscess.[124] Lung abscesses can usually be seen with a chest X-ray but frequently require a chest CT scan to confirm the diagnosis.[124] Abscesses typically occur in aspiration pneumonia, and often contain several types of bacteria. Long-term antibiotics are usually adequate to treat a lung abscess, but sometimes the abscess must be drained by a surgeon or radiologist.[124]
Respiratory and circulatory failure
Pneumonia can cause respiratory failure by triggering acute respiratory distress syndrome (ARDS), which results from a combination of infection and inflammatory response. The lungs quickly fill with fluid and become stiff. This stiffness, combined with severe difficulties extracting oxygen due to the alveolar fluid, may require long periods of mechanical ventilation for survival.[36] Other causes of circulatory failure are hypoxemia, inflammation, and increased coagulability.[33]
Sepsis is a potential complication of pneumonia but occurs usually in people with poor immunity or hyposplenism. The organisms most commonly involved are Streptococcus pneumoniae, Haemophilus influenzae, and Klebsiella pneumoniae. Other causes of the symptoms should be considered such as a myocardial infarction or a pulmonary embolism.[125]
Epidemiology
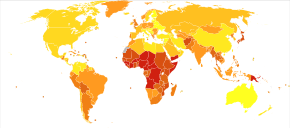
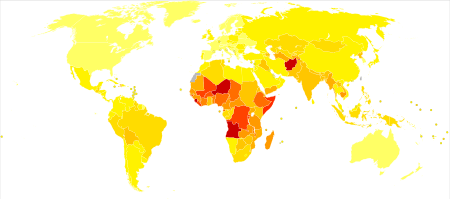
Pneumonia is a common illness affecting approximately 450 million people a year and occurring in all parts of the world.[11] It is a major cause of death among all age groups resulting in 4 million deaths (7% of the world's total death) yearly.[11][12] Rates are greatest in children less than five, and adults older than 75 years.[11] It occurs about five times more frequently in the developing world than in the developed world.[11] Viral pneumonia accounts for about 200 million cases.[11] In the United States, as of 2009, pneumonia is the 8th leading cause of death.[21]
Children
In 2008, pneumonia occurred in approximately 156 million children (151 million in the developing world and 5 million in the developed world).[11] In 2010, it resulted in 1.3 million deaths, or 18% of all deaths in those under five years, of which 95% occurred in the developing world.[11][20][127] Countries with the greatest burden of disease include India (43 million), China (21 million) and Pakistan (10 million).[128] It is the leading cause of death among children in low income countries.[11][12] Many of these deaths occur in the newborn period. The World Health Organization estimates that one in three newborn infant deaths is due to pneumonia.[129] Approximately half of these deaths can be prevented, as they are caused by the bacteria for which an effective vaccine is available.[130] In 2011, pneumonia was the most common reason for admission to the hospital after an emergency department visit in the U.S. for infants and children.[131]
History
Pneumonia has been a common disease throughout human history.[132] The word is from Greek πνεύμων (pneúmōn) meaning "lung".[133] The symptoms were described by Hippocrates (c. 460–370 BC):[132] "Peripneumonia, and pleuritic affections, are to be thus observed: If the fever be acute, and if there be pains on either side, or in both, and if expiration be if cough be present, and the sputa expectorated be of a blond or livid color, or likewise thin, frothy, and florid, or having any other character different from the common... When pneumonia is at its height, the case is beyond remedy if he is not purged, and it is bad if he has dyspnoea, and urine that is thin and acrid, and if sweats come out about the neck and head, for such sweats are bad, as proceeding from the suffocation, rales, and the violence of the disease which is obtaining the upper hand."[134] However, Hippocrates referred to pneumonia as a disease "named by the ancients". He also reported the results of surgical drainage of empyemas. Maimonides (1135–1204 AD) observed: "The basic symptoms that occur in pneumonia and that are never lacking are as follows: acute fever, sticking pleuritic pain in the side, short rapid breaths, serrated pulse and cough."[135] This clinical description is quite similar to those found in modern textbooks, and it reflected the extent of medical knowledge through the Middle Ages into the 19th century.
Edwin Klebs was the first to observe bacteria in the airways of persons having died of pneumonia in 1875.[136] Initial work identifying the two common bacterial causes, Streptococcus pneumoniae and Klebsiella pneumoniae, was performed by Carl Friedländer[137] and Albert Fraenkel[138] in 1882 and 1884, respectively. Friedländer's initial work introduced the Gram stain, a fundamental laboratory test still used today to identify and categorize bacteria. Christian Gram's paper describing the procedure in 1884 helped to differentiate the two bacteria, and showed that pneumonia could be caused by more than one microorganism.[139]
Sir William Osler, known as "the father of modern medicine", appreciated the death and disability caused by pneumonia, describing it as the "captain of the men of death" in 1918, as it had overtaken tuberculosis as one of the leading causes of death in this time. This phrase was originally coined by John Bunyan in reference to "consumption" (tuberculosis).[140][141] Osler also described pneumonia as "the old man's friend" as death was often quick and painless when there were much slower and more painful ways to die.[18]
Several developments in the 1900s improved the outcome for those with pneumonia. With the advent of penicillin and other antibiotics, modern surgical techniques, and intensive care in the 20th century, mortality from pneumonia, which had approached 30%, dropped precipitously in the developed world. Vaccination of infants against Haemophilus influenzae type B began in 1988 and led to a dramatic decline in cases shortly thereafter.[142] Vaccination against Streptococcus pneumoniae in adults began in 1977, and in children in 2000, resulting in a similar decline.[143]
Society and culture
Awareness
Due to the relatively low awareness of the disease, 12 November was declared as the annual World Pneumonia Day, a day for concerned citizens and policy makers to take action against the disease, in 2009.[144][145]
Costs
The global economic cost of community-acquired pneumonia has been estimated at $17 billion annually.[21] Other estimates are considerably higher. In 2012 the estimated aggregate costs of treating pneumonia in the United States were $20 billion;[146] the median cost of a single pneumonia-related hospitalization is over $15,000.[147] According to data released by the Centers for Medicare and Medicaid Services, average 2012 hospital charges for inpatient treatment of uncomplicated pneumonia in the U.S. were $24,549 and ranged as high as $124,000. The average cost of an emergency room consult for pneumonia was $943 and the average cost for medication was $66.[148] Aggregate annual costs of treating pneumonia in Europe have been estimated at €10 billion.[149]
References
- "Other Names for Pneumonia". NHLBI. 1 March 2011. Archived from the original on 6 February 2016. Retrieved 2 March 2016.
- Ashby B, Turkington C (2007). The encyclopedia of infectious diseases (3rd ed.). New York: Facts on File. p. 242. ISBN 978-0-8160-6397-0. Retrieved 21 April 2011.
- Behera, D. (2010). Textbook of pulmonary medicine (2nd ed.). New Delhi: Jaypee Brothers Medical Pub. pp. 296–97. ISBN 978-81-8448-749-7.
- McLuckie, A., ed. (2009). Respiratory disease and its management. New York: Springer. p. 51. ISBN 978-1-84882-094-4.
- Jeffrey C. Pommerville (2010). Alcamo's Fundamentals of Microbiology (9th ed.). Sudbury MA: Jones & Bartlett. p. 323. ISBN 978-0-7637-6258-2.
- "Who Is at Risk for Pneumonia?". NHLBI. 1 March 2011. Archived from the original on 7 March 2016. Retrieved 3 March 2016.
- "How Is Pneumonia Diagnosed?". NHLBI. 1 March 2011. Archived from the original on 7 March 2016. Retrieved 3 March 2016.
- Hoare Z, Lim WS (May 2006). "Pneumonia: update on diagnosis and management" (PDF). BMJ. 332 (7549): 1077–79. doi:10.1136/bmj.332.7549.1077. PMC 1458569. PMID 16675815.
- "How Can Pneumonia Be Prevented?". NHLBI. 1 March 2011. Archived from the original on 7 March 2016. Retrieved 3 March 2016.
- "How Is Pneumonia Treated?". NHLBI. 1 March 2011. Archived from the original on 6 March 2016. Retrieved 3 March 2016.
- Ruuskanen O, Lahti E, Jennings LC, Murdoch DR (April 2011). "Viral pneumonia". Lancet. 377 (9773): 1264–75. doi:10.1016/S0140-6736(10)61459-6. PMID 21435708.
- Lodha R, Kabra SK, Pandey RM (June 2013). "Antibiotics for community-acquired pneumonia in children". The Cochrane Database of Systematic Reviews. 6 (6): CD004874. doi:10.1002/14651858.CD004874.pub4. PMID 23733365.
- Leach, Richard E. (2009). Acute and Critical Care Medicine at a Glance (2nd ed.). Wiley-Blackwell. ISBN 978-1-4051-6139-8.
- "Types of Pneumonia". NHLBI. 1 March 2011. Archived from the original on 5 February 2016. Retrieved 2 March 2016.
- "What Is Pneumonia?". NHLBI. 1 March 2011. Archived from the original on 29 February 2016. Retrieved 2 March 2016.
- Osler, William (1901). Principles and Practice of Medicine, 4th Edition. New York: D. Appleton and Company. p. 108. Archived from the original on 8 July 2007.
- George, Ronald B. (2005). Chest medicine : essentials of pulmonary and critical care medicine (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 353. ISBN 978-0-7817-5273-2.
- Eddy, Orin (December 2005). "Community-Acquired Pneumonia: From Common Pathogens To Emerging Resistance". Emergency Medicine Practice. 7 (12).
- Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. p. 480. ISBN 978-0-07-148480-0.
- Singh V, Aneja S (March 2011). "Pneumonia – management in the developing world". Paediatric Respiratory Reviews. 12 (1): 52–59. doi:10.1016/j.prrv.2010.09.011. PMID 21172676.
- Nair GB, Niederman MS (November 2011). "Community-acquired pneumonia: an unfinished battle". The Medical Clinics of North America. 95 (6): 1143–61. doi:10.1016/j.mcna.2011.08.007. PMID 22032432.
- "Pneumonia (Fact sheet N°331)". World Health Organization. August 2012. Archived from the original on 30 August 2012.
- Darby J, Buising K (October 2008). "Could it be Legionella?". Australian Family Physician. 37 (10): 812–15. PMID 19002299.
- Ortqvist A, Hedlund J, Kalin M (December 2005). "Streptococcus pneumoniae: epidemiology, risk factors, and clinical features". Seminars in Respiratory and Critical Care Medicine. 26 (6): 563–74. doi:10.1055/s-2005-925523. PMID 16388428.
- Murray and Nadel (2010). Chapter 32.
- Lowe JF, Stevens A (2000). Pathology (2nd ed.). St. Louis: Mosby. p. 197. ISBN 978-0-7234-3200-5.
- Bowden, Raleigh A.; Ljungman, Per; Snydman, David R., eds. (2010). Transplant infections. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 978-1-58255-820-2.
- Marrie, Thomas J., ed. (2002). Community-acquired pneumonia. New York: Kluwer Academic Publishers. p. 20. ISBN 978-0-306-46834-6.
- Nguyen, TK; Tran, TH; Roberts, CL; Fox, GJ; Graham, SM; Marais, BJ (January 2017). "Risk factors for child pneumonia – focus on the Western Pacific Region". Paediatric Respiratory Reviews. 21: 95–101. doi:10.1016/j.prrv.2016.07.002. PMID 27515732.
- Eom CS, Jeon CY, Lim JW, Cho EG, Park SM, Lee KS (February 2011). "Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis". Canadian Medical Association Journal. 183 (3): 310–19. doi:10.1503/cmaj.092129. PMC 3042441. PMID 21173070.
- Arthur LE, Kizor RS, Selim AG, van Driel ML, Seoane L (October 2016). "Antibiotics for ventilator-associated pneumonia". The Cochrane Database of Systematic Reviews. 10: CD004267. doi:10.1002/14651858.CD004267.pub4. PMC 6461148. PMID 27763732.
- Alkhawaja S, Martin C, Butler RJ, Gwadry-Sridhar F (August 2015). "Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults". The Cochrane Database of Systematic Reviews (8): CD008875. doi:10.1002/14651858.CD008875.pub2. PMC 6516803. PMID 26241698.
- Elena, Prina; Otavio, T Ranzani; Anthoni, Torres (12 August 2015). "Community-acquired pneumonia". The Lancet. 386 (9998): 1097–1108. doi:10.1016/S0140-6736(15)60733-4. PMID 26277247.
- Sharma S, Maycher B, Eschun G (May 2007). "Radiological imaging in pneumonia: recent innovations". Current Opinion in Pulmonary Medicine. 13 (3): 159–69. doi:10.1097/MCP.0b013e3280f3bff4. PMID 17414122.
- Anevlavis S, Bouros D (February 2010). "Community acquired bacterial pneumonia". Expert Opinion on Pharmacotherapy. 11 (3): 361–74. doi:10.1517/14656560903508770. PMID 20085502.
- Murray and Nadel (2010). Chapter 31.
- Figueiredo LT (September 2009). "Viral pneumonia: epidemiological, clinical, pathophysiological and therapeutic aspects". Jornal Brasileiro de Pneumologia. 35 (9): 899–906. doi:10.1590/S1806-37132009000900012. PMID 19820817.
- Behera, D. (2010). Textbook of pulmonary medicine (2nd ed.). New Delhi: Jaypee Brothers Medical Pub. pp. 391–94. ISBN 978-81-8448-749-7.
- Maskell N, Millar A (2009). Oxford desk reference. Oxford: Oxford University Press. p. 196. ISBN 978-0-19-923912-2.
- Ewald H, Raatz H, Boscacci R, Furrer H, Bucher HC, Briel M (April 2015). "Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV infection". The Cochrane Database of Systematic Reviews (4): CD006150. doi:10.1002/14651858.CD006150.pub2. PMC 6472444. PMID 25835432.
- Murray and Nadel (2010). Chapter 37.
- Vijayan VK (May 2009). "Parasitic lung infections". Current Opinion in Pulmonary Medicine. 15 (3): 274–82. doi:10.1097/MCP.0b013e328326f3f8. PMID 19276810.
- Root, Richard K., ed. (1999). Clinical infectious diseases : a practical approach. New York [u.a.]: Oxford Univ. Press. p. 833. ISBN 978-0-19-508103-9.
- Volume editors, Ulrich Costabel (2007). Diffuse parenchymal lung disease : 47 tables ([Online-Ausg.] ed.). Basel: Karger. p. 4. ISBN 978-3-8055-8153-0.
- Hadda, V; Khilnani, GC (December 2010). "Lipoid pneumonia: an overview". Expert Review of Respiratory Medicine. 4 (6): 799–807. doi:10.1586/ers.10.74. PMID 21128754.
- Ranganathan SC, Sonnappa S (February 2009). "Pneumonia and other respiratory infections". Pediatric Clinics of North America. 56 (1): 135–56, xi. doi:10.1016/j.pcl.2008.10.005. PMID 19135585.
- Anderson, Douglas M. (2000). Dorland's illustrated medical dictionary (29 ed.). Philadelphia [u.a.]: Saunders. p. 1414. ISBN 978-0-7216-8261-7.
- Hammer, Gary D.; McPhee, Stephen J., eds. (2010). Pathophysiology of disease : an introduction to clinical medicine (6th ed.). New York: McGraw-Hill Medical. p. Chapter 4. ISBN 978-0-07-162167-0.
- Fein, Alan (2006). Diagnosis and management of pneumonia and other respiratory infections (2nd ed.). Caddo, OK: Professional Communications. pp. 28–29. ISBN 978-1-884735-63-9.
- Kumar, Vinay (2010). Robbins and Cotran pathologic basis of disease (8th ed.). Philadelphia: Saunders/Elsevier. p. Chapter 15. ISBN 978-1-4160-3121-5.
- Fleisher, Gary R.; Ludwig, Stephen, eds. (2010). Textbook of pediatric emergency medicine (6th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health. p. 914. ISBN 978-1-60547-159-4.
- Lynch T, Bialy L, Kellner JD, Osmond MH, Klassen TP, Durec T, Leicht R, Johnson DW (August 2010). Huicho L (ed.). "A systematic review on the diagnosis of pediatric bacterial pneumonia: when gold is bronze". PLOS ONE. 5 (8): e11989. Bibcode:2010PLoSO...511989L. doi:10.1371/journal.pone.0011989. PMC 2917358. PMID 20700510.
- Marchello, CS; Ebell, MH; Dale, AP; Harvill, ET; Shen, Y; Whalen, CC (2019). "Signs and Symptoms That Rule out Community-Acquired Pneumonia in Outpatient Adults: A Systematic Review and Meta-Analysis". Journal of the American Board of Family Medicine : JABFM. 32 (2): 234–247. doi:10.3122/jabfm.2019.02.180219. PMID 30850460.
- Dale, AP; Marchello, C; Ebell, MH (July 2019). "Clinical gestalt to diagnose pneumonia, sinusitis, and pharyngitis: a meta-analysis". The British Journal of General Practice. 69 (684): e444–e453. doi:10.3399/bjgp19X704297. PMC 6582453. PMID 31208974.
- Ezzati M, Lopez AD, Rodgers A, Murray CJ (2004). Comparative quantification of health risks. Genève: Organisation mondiale de la santé. p. 70. ISBN 978-92-4-158031-1.
- Shah SN, Bachur RG, Simel DL, Neuman MI (August 2017). "Does This Child Have Pneumonia?: The Rational Clinical Examination Systematic Review". JAMA. 318 (5): 462–71. doi:10.1001/jama.2017.9039. PMID 28763554.
- Rambaud-Althaus C, Althaus F, Genton B, D'Acremont V (April 2015). "Clinical features for diagnosis of pneumonia in children younger than 5 years: a systematic review and meta-analysis". The Lancet. Infectious Diseases. 15 (4): 439–50. doi:10.1016/s1473-3099(15)70017-4. PMID 25769269.
- Wang, Kay; Gill, Peter; Perera, Rafael; Thomson, Anne; Mant, David; Harnden, Anthony (17 October 2012). "Clinical symptoms and signs for the diagnosis of Mycoplasma pneumoniae in children and adolescents with community-acquired pneumonia". The Cochrane Database of Systematic Reviews. 10: CD009175. doi:10.1002/14651858.CD009175.pub2. ISSN 1469-493X. PMID 23076954.
- Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, Wani M, Woodhead MA (October 2009). "BTS guidelines for the management of community acquired pneumonia in adults: update 2009". Thorax. 64 Suppl 3 (Suppl 3): iii–155. doi:10.1136/thx.2009.121434. PMID 19783532.
- Saldías F, Méndez JI, Ramírez D, Díaz O (April 2007). "[Predictive value of history and physical examination for the diagnosis of community-acquired pneumonia in adults: a literature review]". Revista Médica de Chile. 135 (4): 517–28. PMID 17554463.
- Schuetz P, Wirz Y, Sager R, Christ-Crain M, Stolz D, Tamm M, et al. (January 2018). "Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis". The Lancet. Infectious Diseases. 18 (1): 95–107. doi:10.1016/S1473-3099(17)30592-3. PMID 29037960.
- Call SA, Vollenweider MA, Hornung CA, Simel DL, McKinney WP (February 2005). "Does this patient have influenza?". JAMA. 293 (8): 987–97. doi:10.1001/jama.293.8.987. PMID 15728170.
- Helms, Clyde A.; Brant, William E., eds. (20 March 2012). Fundamentals of diagnostic radiology (4th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. p. 435. ISBN 978-1-60831-911-4.
- Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J (February 2017). "Accuracy of Lung Ultrasonography in the Diagnosis of Pneumonia in Adults: Systematic Review and Meta-Analysis". Chest. 151 (2): 374–82. doi:10.1016/j.chest.2016.10.039. PMID 27818332.
- Ye, X; Xiao, H; Chen, B; Zhang, S (2015). "Accuracy of Lung Ultrasonography versus Chest Radiography for the Diagnosis of Adult Community-Acquired Pneumonia: Review of the Literature and Meta-Analysis". PLOS ONE. 10 (6): e0130066. Bibcode:2015PLoSO..1030066Y. doi:10.1371/journal.pone.0130066. PMC 4479467. PMID 26107512.
- "UOTW No. 34 – Ultrasound of the Week". Ultrasound of the Week. 20 January 2015. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- Metlay, JP; Waterer, GW; Long, AC; Anzueto, A; Brozek, J; Crothers, K; Cooley, LA; Dean, NC; Fine, MJ; Flanders, SA; Griffin, MR; Metersky, ML; Musher, DM; Restrepo, MI; Whitney, CG (1 October 2019). "Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America". American Journal of Respiratory and Critical Care Medicine. 200 (7): e45–e67. doi:10.1164/rccm.201908-1581ST. PMID 31573350.
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG (March 2007). "Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults". Clinical Infectious Diseases. 44 Suppl 2 (Suppl 2): S27–72. doi:10.1086/511159. PMID 17278083.
- Stedman's medical dictionary (28th ed.). Philadelphia: Lippincott Williams & Wilkins. 2006. ISBN 978-0-7817-6450-6.
- Dunn L (29 June – 5 July 2005). "Pneumonia: classification, diagnosis and nursing management". Nursing Standard. 19 (42): 50–54. doi:10.7748/ns2005.06.19.42.50.c3901. PMID 16013205.
- organization, World health (2005). Pocket book of hospital care for children : guidelines for the management of common illnesses with limited resources. Geneva: World Health Organization. p. 72. ISBN 978-92-4-154670-6.
- Anand N, Kollef MH (February 2009). "The alphabet soup of pneumonia: CAP, HAP, HCAP, NHAP, and VAP". Seminars in Respiratory and Critical Care Medicine. 30 (1): 3–9. doi:10.1055/s-0028-1119803. PMID 19199181.
- American Thoracic Society; Infectious Diseases Society of America (2005). "Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia". Am J Respir Crit Care Med. 171 (4): 388–416. doi:10.1164/rccm.200405-644ST. PMID 15699079.
- Demicheli, Vittorio; Jefferson, Tom; Ferroni, Eliana; Rivetti, Alessandro; Di Pietrantonj, Carlo (2018). "Vaccines for preventing influenza in healthy adults". The Cochrane Database of Systematic Reviews. 2: CD001269. doi:10.1002/14651858.CD001269.pub6. ISSN 1469-493X. PMC 6491184. PMID 29388196.
- "Seasonal Influenza (Flu)". Center for Disease Control and Prevention. Archived from the original on 29 June 2011. Retrieved 29 June 2011.
- Lucero MG, Dulalia VE, Nillos LT, Williams G, Parreño RA, Nohynek H, Riley ID, Makela H (October 2009). "Pneumococcal conjugate vaccines for preventing vaccine-type invasive pneumococcal disease and X-ray defined pneumonia in children less than two years of age". The Cochrane Database of Systematic Reviews (4): CD004977. doi:10.1002/14651858.CD004977.pub2. PMC 6464899. PMID 19821336.
- "WHO | Pneumococcal conjugate vaccines". www.who.int. Retrieved 16 January 2018.
- "Pneumococcal Disease | Vaccines – PCV13 and PPSV23 | CDC". www.cdc.gov. 18 September 2017. Retrieved 16 January 2018.
- Moberley S, Holden J, Tatham DP, Andrews RM (January 2013). "Vaccines for preventing pneumococcal infection in adults". The Cochrane Database of Systematic Reviews. 1 (1): CD000422. doi:10.1002/14651858.CD000422.pub3. PMID 23440780.
- Walters JA, Tang JN, Poole P, Wood-Baker R (January 2017). "Pneumococcal vaccines for preventing pneumonia in chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews. 1: CD001390. doi:10.1002/14651858.CD001390.pub4. PMC 6422320. PMID 28116747.
- "Pneumonia Can Be Prevented – Vaccines Can Help". Centers for Disease Control and Prevention. Archived from the original on 23 October 2012. Retrieved 22 October 2012.
- Jefferson T, Demicheli V, Di Pietrantonj C, Rivetti D (April 2006). "Amantadine and rimantadine for influenza A in adults". The Cochrane Database of Systematic Reviews (2): CD001169. doi:10.1002/14651858.CD001169.pub3. PMID 16625539.
- Jefferson T, Jones MA, Doshi P, Del Mar CB, Hama R, Thompson MJ, Spencer EA, Onakpoya I, Mahtani KR, Nunan D, Howick J, Heneghan CJ (April 2014). "Neuraminidase inhibitors for preventing and treating influenza in healthy adults and children". The Cochrane Database of Systematic Reviews. 4 (4): CD008965. doi:10.1002/14651858.CD008965.pub4. PMC 6464969. PMID 24718923.
- Gray DM, Zar HJ (May 2010). "Community-acquired pneumonia in HIV-infected children: a global perspective". Current Opinion in Pulmonary Medicine. 16 (3): 208–16. doi:10.1097/MCP.0b013e3283387984. PMID 20375782.
- Huang L, Cattamanchi A, Davis JL, den Boon S, Kovacs J, Meshnick S, Miller RF, Walzer PD, Worodria W, Masur H (June 2011). "HIV-associated Pneumocystis pneumonia". Proceedings of the American Thoracic Society. 8 (3): 294–300. doi:10.1513/pats.201009-062WR. PMC 3132788. PMID 21653531.
- Stern A, Green H, Paul M, Vidal L, Leibovici L (October 2014). "Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients". The Cochrane Database of Systematic Reviews. 10 (10): CD005590. doi:10.1002/14651858.CD005590.pub3. PMC 6457644. PMID 25269391.
- Taminato M, Fram D, Torloni MR, Belasco AG, Saconato H, Barbosa DA (November–December 2011). "Screening for group B Streptococcus in pregnant women: a systematic review and meta-analysis". Revista Latino-Americana de Enfermagem. 19 (6): 1470–78. doi:10.1590/s0104-11692011000600026. PMID 22249684.
- Darville T (October 2005). "Chlamydia trachomatis infections in neonates and young children". Seminars in Pediatric Infectious Diseases. 16 (4): 235–44. doi:10.1053/j.spid.2005.06.004. PMID 16210104.
- Global Action Plan for Prevention and Control of Pneumonia (GAPP) (PDF). World Health Organization. 2009. Archived (PDF) from the original on 17 October 2013.
- Roggensack A, Jefferies AL, Farine D (April 2009). "Management of meconium at birth". Journal of Obstetrics and Gynaecology Canada. 31 (4): 353–54. doi:10.1016/s1701-2163(16)34153-6. PMID 19497156.
- van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C (March 2013). "Oral health care and aspiration pneumonia in frail older people: a systematic literature review". Gerodontology. 30 (1): 3–9. doi:10.1111/j.1741-2358.2012.00637.x. PMID 22390255.
- Lassi ZS, Moin A, Bhutta ZA (December 2016). "Zinc supplementation for the prevention of pneumonia in children aged 2 months to 59 months". The Cochrane Database of Systematic Reviews. 12: CD005978. doi:10.1002/14651858.CD005978.pub3. PMC 6463931. PMID 27915460.
- Hemilä H, Louhiala P (August 2013). "Vitamin C for preventing and treating pneumonia". The Cochrane Database of Systematic Reviews (8): CD005532. doi:10.1002/14651858.CD005532.pub3. PMID 23925826.
- Gillies, Donna; Todd, David A.; Foster, Jann P.; Batuwitage, Bisanth T. (2017). "Heat and moisture exchangers versus heated humidifiers for mechanically ventilated adults and children". The Cochrane Database of Systematic Reviews. 9: CD004711. doi:10.1002/14651858.CD004711.pub3. ISSN 1469-493X. PMC 6483749. PMID 28905374.
- Liu, Chang; Cao, Yubin; Lin, Jie; Ng, Linda; Needleman, Ian; Walsh, Tanya; Li, Chunjie (2018). "Oral care measures for preventing nursing home‐acquired pneumonia" (PDF). Cochrane Database of Systematic Reviews. 9 (9): CD012416. doi:10.1002/14651858.CD012416.pub2. ISSN 1465-1858. PMC 6513285. PMID 30264525.
- Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, Kaplan SL, Mace SE, McCracken GH, Moore MR, St Peter SD, Stockwell JA, Swanson JT (October 2011). "The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America". Clinical Infectious Diseases. 53 (7): e25–76. doi:10.1093/cid/cir531. PMID 21880587.
- Chaves, Gabriela Ss; Freitas, Diana A.; Santino, Thayla A.; Nogueira, Patricia Angelica Ms; Fregonezi, Guilherme Af; Mendonça, Karla Mpp (2019). "Chest physiotherapy for pneumonia in children". The Cochrane Database of Systematic Reviews. 1: CD010277. doi:10.1002/14651858.CD010277.pub3. ISSN 1469-493X. PMC 6353233. PMID 30601584.
- Yang M, Yan Y, Yin X, Wang BY, Wu T, Liu GJ, Dong BR (February 2013). "Chest physiotherapy for pneumonia in adults". The Cochrane Database of Systematic Reviews. 2 (2): CD006338. doi:10.1002/14651858.CD006338.pub3. PMID 23450568.
- Chang CC, Cheng AC, Chang AB (March 2014). "Over-the-counter (OTC) medications to reduce cough as an adjunct to antibiotics for acute pneumonia in children and adults". The Cochrane Database of Systematic Reviews. 3 (3): CD006088. doi:10.1002/14651858.CD006088.pub4. PMID 24615334.
- Haider, Batool A.; Lassi, Zohra S.; Ahmed, Amina; Bhutta, Zulfiqar A. (5 October 2011). "Zinc supplementation as an adjunct to antibiotics in the treatment of pneumonia in children 2 to 59 months of age". The Cochrane Database of Systematic Reviews (10): CD007368. doi:10.1002/14651858.CD007368.pub2. ISSN 1469-493X. PMID 21975768.
- Ni J, Wei J, Wu T (July 2005). "Vitamin A for non-measles pneumonia in children". The Cochrane Database of Systematic Reviews (3): CD003700. doi:10.1002/14651858.CD003700.pub2. PMID 16034908.
- Das, Rashmi R.; Singh, Meenu; Naik, Sushree S. (19 July 2018). "Vitamin D as an adjunct to antibiotics for the treatment of acute childhood pneumonia". The Cochrane Database of Systematic Reviews. 7: CD011597. doi:10.1002/14651858.CD011597.pub2. ISSN 1469-493X. PMC 6513535. PMID 30024634.
- Phua, Jason; Dean, Nathan C.; Guo, Qi; Kuan, Win Sen; Lim, Hui Fang; Lim, Tow Keang (28 August 2016). "Severe community-acquired pneumonia: timely management measures in the first 24 hours". Critical Care. 20 (1): 237. doi:10.1186/s13054-016-1414-2. PMC 5002335. PMID 27567896.
- Zhang Y, Fang C, Dong BR, Wu T, Deng JL (March 2012). Dong BR (ed.). "Oxygen therapy for pneumonia in adults". The Cochrane Database of Systematic Reviews. 3 (3): CD006607. doi:10.1002/14651858.CD006607.pub4. PMID 22419316.
- Pakhale S, Mulpuru S, Verheij TJ, Kochen MM, Rohde GG, Bjerre LM (October 2014). "Antibiotics for community-acquired pneumonia in adult outpatients". The Cochrane Database of Systematic Reviews (10): CD002109. doi:10.1002/14651858.CD002109.pub4. PMID 25300166.
- Lutfiyya MN, Henley E, Chang LF, Reyburn SW (February 2006). "Diagnosis and treatment of community-acquired pneumonia" (PDF). American Family Physician. 73 (3): 442–50. PMID 16477891. Archived (PDF) from the original on 9 April 2012.
- "Pneumonia Fact Sheet". World Health Organization. September 2016. Retrieved 14 January 2018.
- Lodha R, Kabra SK, Pandey RM (June 2013). "Antibiotics for community-acquired pneumonia in children". The Cochrane Database of Systematic Reviews (6): CD004874. doi:10.1002/14651858.CD004874.pub4. PMID 23733365.
- Eliakim-Raz N, Robenshtok E, Shefet D, Gafter-Gvili A, Vidal L, Paul M, Leibovici L (September 2012). Eliakim-Raz N (ed.). "Empiric antibiotic coverage of atypical pathogens for community-acquired pneumonia in hospitalized adults". The Cochrane Database of Systematic Reviews. 9 (9): CD004418. doi:10.1002/14651858.CD004418.pub4. PMID 22972070.
- Lee JS, Giesler DL, Gellad WF, Fine MJ (February 2016). "Antibiotic Therapy for Adults Hospitalized With Community-Acquired Pneumonia: A Systematic Review". JAMA. 315 (6): 593–602. doi:10.1001/jama.2016.0115. PMID 26864413.
- Rojas MX, Granados C (April 2006). "Oral antibiotics versus parenteral antibiotics for severe pneumonia in children". Cochrane Database Syst Rev (2): CD004979. doi:10.1002/14651858.CD004979.pub2. PMID 16625618.
- Tansarli, GS; Mylonakis, E (September 2018). "Systematic Review and Meta-analysis of the Efficacy of Short-Course Antibiotic Treatments for Community-Acquired Pneumonia in Adults". Antimicrobial Agents and Chemotherapy. 62 (9). doi:10.1128/AAC.00635-18. PMC 6125522. PMID 29987137.
- Scalera NM, File TM (April 2007). "How long should we treat community-acquired pneumonia?". Current Opinion in Infectious Diseases. 20 (2): 177–81. doi:10.1097/QCO.0b013e3280555072. PMID 17496577.
- Pugh R, Grant C, Cooke RP, Dempsey G (August 2015). "Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults". The Cochrane Database of Systematic Reviews (8): CD007577. doi:10.1002/14651858.CD007577.pub3. PMID 26301604.
- Haider BA, Saeed MA, Bhutta ZA (April 2008). "Short-course versus long-course antibiotic therapy for non-severe community-acquired pneumonia in children aged 2 months to 59 months". The Cochrane Database of Systematic Reviews (2): CD005976. doi:10.1002/14651858.CD005976.pub2. PMID 18425930.
- Stern A, Skalsky K, Avni T, Carrara E, Leibovici L, Paul M (December 2017). "Corticosteroids for pneumonia". The Cochrane Database of Systematic Reviews. 12: CD007720. doi:10.1002/14651858.CD007720.pub3. PMC 6486210. PMID 29236286.
- Wu, WF; Fang, Q; He, GJ (February 2018). "Efficacy of corticosteroid treatment for severe community-acquired pneumonia: A meta-analysis". The American Journal of Emergency Medicine. 36 (2): 179–84. doi:10.1016/j.ajem.2017.07.050. PMID 28756034.
- Cheng AC, Stephens DP, Currie BJ (April 2007). "Granulocyte-colony stimulating factor (G-CSF) as an adjunct to antibiotics in the treatment of pneumonia in adults". The Cochrane Database of Systematic Reviews (2): CD004400. doi:10.1002/14651858.CD004400.pub3. PMID 17443546.
- Marik PE (May 2011). "Pulmonary aspiration syndromes". Current Opinion in Pulmonary Medicine. 17 (3): 148–54. doi:10.1097/MCP.0b013e32834397d6. PMID 21311332.
- O'Connor S (2003). "Aspiration pneumonia and pneumonitis". Australian Prescriber. 26 (1): 14–17. doi:10.18773/austprescr.2003.009.
- Ramsdell, Joe; Narsavage, Georgia L.; Fink, James B. (May 2005). "Management of Community-Acquired Pneumonia in the Home". Chest. 127 (5): 1752–1763. doi:10.1378/chest.127.5.1752. PMID 15888856.
- Cunha (2010). pp. 6–18.
- Rello J (2008). "Demographics, guidelines, and clinical experience in severe community-acquired pneumonia". Critical Care. 12 Suppl 6 (Suppl 6): S2. doi:10.1186/cc7025. PMC 2607112. PMID 19105795.
- Yu H (March 2011). "Management of pleural effusion, empyema, and lung abscess". Seminars in Interventional Radiology. 28 (1): 75–86. doi:10.1055/s-0031-1273942. PMC 3140254. PMID 22379278.
- Cunha (2010). pp. 250–51.
- "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002. Archived from the original on 16 January 2013.
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE (June 2012). "Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000". Lancet. 379 (9832): 2151–61. doi:10.1016/S0140-6736(12)60560-1. PMID 22579125.
- Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H (May 2008). "Epidemiology and etiology of childhood pneumonia". Bulletin of the World Health Organization. 86 (5): 408–16. doi:10.2471/BLT.07.048769. PMC 2647437. PMID 18545744.
- Garenne M, Ronsmans C, Campbell H (1992). "The magnitude of mortality from acute respiratory infections in children under 5 years in developing countries". World Health Statistics Quarterly. Rapport Trimestriel de Statistiques Sanitaires Mondiales. 45 (2–3): 180–91. PMID 1462653.
- WHO (June 1999). "Pneumococcal vaccines. WHO position paper". Releve Epidemiologique Hebdomadaire. 74 (23): 177–83. PMID 10437429.
- Weiss AJ, Wier LM, Stocks C, Blanchard J (June 2014). "Overview of Emergency Department Visits in the United States, 2011". HCUP Statistical Brief No. 174. Rockville, MD: Agency for Healthcare Research and Quality. Archived from the original on 3 August 2014.
- Feigin, Ralph (2004). Textbook of Pediatric Infectious Diseases (5th ed.). Philadelphia: W. B. Saunders. p. 299. ISBN 978-0-7216-9329-3.
- Stevenson, Angus (2010). Oxford Dictionary of English. OUP Oxford. p. 1369. ISBN 978-0-19-957112-3.
- Hippocrates On Acute Diseases wikisource link
- Maimonides, Fusul Musa ("Pirkei Moshe").
- Klebs E (10 December 1875). "Beiträge zur Kenntniss der pathogenen Schistomyceten. VII Die Monadinen" [Signs for Recognition of the Pathogen Schistomyceten]. Arch. Exp. Pathol. Pharmakol. 4 (5/6): 40–88.
- Friedländer C (4 February 1882). "Über die Schizomyceten bei der acuten fibrösen Pneumonie". Archiv für Pathologische Anatomie und Physiologie und für Klinische Medizin. 87 (2): 319–24. doi:10.1007/BF01880516.
- Fraenkel A (21 April 1884). "Über die genuine Pneumonie, Verhandlungen des Congress für innere Medicin". Dritter Congress. 3: 17–31.
- Gram C (15 March 1884). "Über die isolierte Färbung der Schizomyceten in Schnitt- und Trocken-präparaten". Fortschr. Med. 2 (6): 185–89.
- J.F. Tomashefski, Jr., ed. (2008). Dail and Hammar's pulmonary pathology (3rd ed.). New York: Springer. p. 228. ISBN 978-0-387-98395-0.
- Osler W, McCrae T (1920). The principles and practice of medicine: designed for the use of practitioners and students of medicine (9th ed.). D. Appleton. p. 78.
One of the most widespread and fatal of all acute diseases, pneumonia has become the "Captain of the Men of Death", to use the phrase applied by John Bunyan to consumption.
- Adams WG, Deaver KA, et al. (January 1993). "Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era". JAMA. 269 (2): 221–26. doi:10.1001/jama.1993.03500020055031. PMID 8417239.
- Whitney CG, Farley MM, et al. (May 2003). "Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine". The New England Journal of Medicine. 348 (18): 1737–46. doi:10.1056/NEJMoa022823. PMID 12724479.
- "World Pneumonia Day Official Website". Fiinex. Archived from the original on 2 September 2011. Retrieved 13 August 2011.
- Hajjeh R, Whitney CG (November 2012). "Call to action on world pneumonia day". Emerging Infectious Diseases. 18 (11): 1898–99. doi:10.3201/eid1811.121217. PMC 3559175. PMID 23092708.
- "Household Component Summary Data Tables". Archived from the original on 20 February 2017.
- "Household Component Summary Data Tables". Archived from the original on 20 February 2017.
- "One hospital charges $8,000 – another, $38,000". The Washington Post.
- Welte T, Torres A, Nathwani D (January 2012). "Clinical and economic burden of community-acquired pneumonia among adults in Europe". Thorax. 67 (1): 71–79. doi:10.1136/thx.2009.129502. PMID 20729232.
Bibliography
- John F. Murray (2010). Murray and Nadel's textbook of respiratory medicine (5th ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4710-0.
- Burke A. Cunha, ed. (2010). Pneumonia essentials (3rd ed.). Sudbury, MA: Physicians' Press. ISBN 978-0-7637-7220-8.
External links
| Wikiquote has quotations related to: Pneumonia |
| Classification | |
|---|---|
| External resources |
|