Thelarche
Thelarche is the onset of secondary breast development, which often represents the beginning of pubertal development.[1] The initial growth of breasts occurs during fetal development in both males and females.[2] Thelarche is the stage at which male and female breasts become distinct due to variance in hormone levels; however, some males have a condition in which they develop breasts, a term called gynecomastia.[2][3] Thelarche, also known as breast budding, typically occurs between the ages of 8 and 13 years with significant variation between individuals.[1][4][5] The cause of this variation is a question central to countless research projects, yet it is generally accepted that race, genetics, exercise, and body mass each influence the age of thelarche.[1][4][6] Puberty is considered delayed if breast development does not start before age 13 or if a female has not had her first period (menarche) within 3 years of thelarche.[7] Ordinarily, females experience menarche about 2 years after thelarche has begun.[6] Complete breast development, from thelarche to adult breasts, takes between 2 and 4 years.[1][6] If secondary breast development occurs before the age of 7 or 8 years, the individual may be experiencing either premature thelarche or precocious puberty.
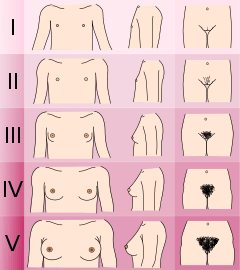
Pubertal changes, including breast development, are assessed using the Tanner Scale (Sexual Maturity Rating Scale) where stage 1 represents the lack of breast development, stage 2 is the breast budding or thelarche stage, stages 3 and 4 are continual breast growth and areolar development, and finally, stage 5 signifies completion of development.[6][8] This system does not use breast size, but instead examines the shape of breasts, nipples, and areolae to determine the progression of growth.[6]
The growth and accumulation of adipose tissue in the breasts are induced by estrogen, while the development of mammary glands and areolae are caused by progesterone; both estrogen and progesterone are produced by ovaries.[1][3][6] Due to change in hormone levels, young breasts are likely to develop asymmetrically and in many cases, adult breasts will remain unequal in size or shape.[5][6] For some girls, thelarche will occur, soon followed by the regression of breast development, and then months or years later, normal breast growth will commence again accompanied by normal pubertal changes; this is termed transient thelarche.[1]
Premature thelarche
Premature thelarche is a benign condition in which a young female has breast development before the age of 8 without any accompanied pubertal changes.[2][7][9][10] Individuals suffering from premature thelarche do not experience menstruation, pubic hair growth (pubarche), or the bone growth characteristic of puberty.[9] The breasts do not develop past stage 3 on the Tanner Scale, hence maintaining adolescent nipples.[5][9] The most common age for females to develop isolated premature thelarche is between the ages of 0 and 2 years with a prevalence rate between 2.2 and 4.7 percent of all female infants.[7][11] The breasts of these females typically exhibit alternating progression and regression patterns of growth in 6-week intervals, often completely decreasing in size within 1.5 years.[4][5][9][12] Due to the benign nature of the condition and the tendency to self-resolve, premature thelarche does not require treatment.[12]
Precocious puberty
Precocious puberty is a condition where females experience puberty before the age of seven or eight years.[4] Precocious puberty differs from premature thelarche in that the individual experiences additional indications of puberty including menarche, adrenarche, pubarche, vaginal discharge, and bone growth, while premature thelarche is identified by the sole presence of early thelarche.[13] Though premature thelarche and precocious puberty are distinct conditions, there is some overlap; an estimated 14 to 18 percent of females who exhibit premature thelarche will additionally develop precocious puberty.[1][5][4] Precocious puberty can be identified using a pelvic ultrasound to assess the size of ovaries and uterus relative to the individual's age.[4] Other methods of diagnosis consist of blood tests to determine hormone levels and simple physician assessments with follow-up appointments to track the progression of development.[4]
Thelarche variant
Thelarche variant, also named exaggerated thelarche, is an intermediate condition between premature thelarche and precocious puberty.[9] This condition resembles premature thelarche without the cyclic waxing and waning of breast growth.[9] Pubic hair growth (pubarche) and advanced bone growth are often present in thelarche variant, yet this growth does not result in complete sexual maturity as occurs with precocious puberty.[9][12]
Racial variation in thelarche
Statistics indicate that the average age of thelarche differs depending on racial population.[3][4] The average age of thelarche for African American females in the United States is between 8.9 and 9.5 years, the average for Causasians is 10-10.4 years, and the average age of thelarche for Hispanic females is approximately 9.8 years.[3][4] Due to the decreasing age of thelarche over time, there is discussion of adjusting the cutoff for early thelarche to 7 years old for white females and 6 years old for black females.[13]
See also
References
- De Silva, Nirupama K. (April 2018). "Breast development and disorders in the adolescent female". Best Practice & Research Clinical Obstetrics & Gynaecology. 48: 40–50. doi:10.1016/j.bpobgyn.2017.08.009. ISSN 1521-6934. PMID 28935365.
- Bao, Yong; Diamantopoulos, Stavros (2007-09-01). "Gynecomastia and Premature Thelarche: A Guide for Practitioners". Pediatrics in Review. 28 (9): e57–e68. doi:10.1542/pir.28-9-e57. ISSN 0191-9601. PMID 17766590.
- Colvin, Caroline Wingo; Abdullatif, Hussein (2012-09-19). "Anatomy of female puberty: The clinical relevance of developmental changes in the reproductive system". Clinical Anatomy. 26 (1): 115–129. doi:10.1002/ca.22164. ISSN 0897-3806. PMID 22996962.
- Sanfilippo, Joseph S.; Lara-Torre, Eduardo; Edmonds, D. Keith; Templeman, Claire, eds. (2008-12-24). Clinical Pediatric and Adolescent Gynecology. ISBN 9780203091784. OCLC 992561838.
- Bauer, Andrew J.; Francis, Gary L.; Poth, Merrily (May 2001). "Review of Precocious Puberty: Part III—Premature Thelarche and Premature Adrenarche. Variations of Normal?". The Endocrinologist. 11 (3): 196–203. doi:10.1097/00019616-200105000-00006. ISSN 1051-2144.
- Litt, Iris F. (1997). Taking Our Pulse: The Health of America's Women. Stanford University Press. ISBN 9780804731379.
- Sultan, Charles; Gaspari, Laura; Maimoun, Laurent; Kalfa, Nicolas; Paris, Françoise (April 2018). "Disorders of puberty". Best Practice & Research Clinical Obstetrics & Gynaecology. 48: 62–89. doi:10.1016/j.bpobgyn.2017.11.004. PMID 29422239.
- Hauspie, Roland C.; Cameron, Noël; Molinari, Luciano (2004-06-24). Methods in Human Growth Research. Cambridge University Press. ISBN 9781139451680.
- Sultan, Charles (2004-01-01). Pediatric and Adolescent Gynecology: Evidence-based Clinical Practice. Karger Medical and Scientific Publishers. ISBN 9783805576239.
- Sultan, C. (2012-07-30). Pediatric and Adolescent Gynecology. Karger Medical and Scientific Publishers. ISBN 9783805593373.
- Khokhar, Aditi; Mojica, Angela (2018-01-01). "Premature Thelarche". Pediatric Annals. 47 (1): e12–e15. doi:10.3928/19382359-20171214-01. ISSN 1938-2359. PMID 29323691.
- Balen, Adam H.; Creighton, Sarah M.; Davies, Melanie C.; MacDougall, Jane; Stanhope, Richard (2004-04-01). Paediatric and Adolescent Gynaecology: A Multidisciplinary Approach. Cambridge University Press. ISBN 9781107320185.
- Lebrethon, Marie-Christine; Bourguignon, Jean-Pierre (August 2000). "Management of central isosexual precocity: diagnosis, treatment, outcome". Current Opinion in Pediatrics. 12 (4): 394–399. doi:10.1097/00008480-200008000-00020. ISSN 1040-8703.