Branchial cleft cyst
A branchial cleft cyst is a cyst as a swelling in the upper part of neck anterior to sternocleidomastoid. It can, but does not necessarily, have an opening to the skin surface, called a fistula. The cause is usually a developmental abnormality arising in the early prenatal period, typically failure of obliteration of the second branchial cleft, i.e. failure of fusion of the second and third branchial arches. Branchial cleft cysts account for almost 20% of neck masses in children.[1] Less commonly, the cysts can develop from the first, third, or fourth clefts, and their location and the location of associated fistulas differs accordingly.
| Branchial arch fistula | |
|---|---|
| Other names | Benign cervical lymphoepithelial cyst Pharyngeal arch cyst |
 | |
| Fistulogram (sinogram) of a right branchial cleft sinus. | |
| Specialty | Medical genetics |
| Symptoms | Painless, firm mass lateral to midline, usually anterior to the SCM, which does not move with swallowing |
| Causes | Family history |
| Differential diagnosis | Vascular anomaly, dermoid cyst, thymic cyst, lymphadenopathy, lymphoma, HPV-related oropharyngeal cancer |
| Treatment | Conservative, surgical excision |
Symptoms
Most branchial cleft cysts present in late childhood or early adulthood as a solitary, painless mass, which went previously unnoticed, that has now become infected (typically after an upper respiratory tract infection). Fistulas, if present, are asymptomatic until infection arises.[2]
Pathophysiology
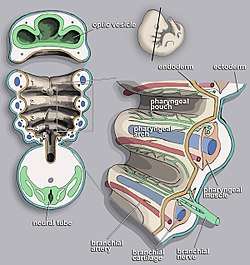
Branchial cleft cysts are remnants of embryonic development and result from a failure of obliteration of one of the branchial clefts, which are homologous to the structures in fish that develop into gills.[3][4]
Pathology
The cyst wall is composed of squamous epithelium (90%), columnar cells with or without cilia, or a mixture of both, with lymphoid infiltrate, often with prominent germinal centers and few subcapsular lymph sinuses. The cyst is typically surrounded by lymphoid tissue that has attenuated or absent overlying epithelium due to inflammatory changes.[5] The cyst may or may not contain granular and keratinaceous cellular debris. Cholesterol crystals may be found in the fluid extracted from a branchial cyst.
Diagnosis
The diagnosis of branchial cleft cysts are typically done clinically due to their relatively consistent location in the neck, typically anterior to the sternocleidomastoid muscle. For masses presenting in adulthood, the presumption should be a malignancy until proven otherwise, since carcinomas of the tonsil, tongue base and thyroid may all present as cystic masses of the neck.[6] Unlike a thyroglossal duct cyst, when swallowing, the mass should not move up or down.[7]
Types

Four branchial clefts (also called "grooves") form during the development of a human embryo. The first cleft normally develops into the external auditory canal,[8] but the remaining three arches are obliterated and have no persistent structures in normal development. Persistence or abnormal formation of these four clefts can all result in branchial cleft cysts which may or may not drain via sinus tracts.
- First branchial cleft cysts are rare (less than 1%)[9] and typically originate in the angle of the mandible and extend to the external auditory canal. They are in close proximity to the facial nerve.
- Second branchial cleft cysts account for a majority of branchial cleft cysts and can be found along the anterior border of the sternocleidomastoid muscle in the same region as the level II cervical lymph nodes. If sinus tracts are present, they typically drain into the tonsillar fossa, found between the palatoglossal arch and the palatopharyngeal arch.[9] The location and cystic nature of second branchial cleft cysts can make them difficult to clinically distinguish from HPV-related oropharyngeal squamous cell carcinoma.[6]
- Third and fourth branchial cleft cysts are rare. They are located about two-thirds of the way down the sternocleidomastoid muscle anteriorly, usually lower than second branchial cleft cysts. Sinus tracts, if present, ascend along the carotid sheath posteriorly to the internal carotid artery, under the glossopharyngeal nerve, and over the vagus nerve and hypoglossal nerve to open into the piriform sinus or thyrohyoid membrane.[9]
Treatment
Conservative (i.e. no treatment), or surgical excision. With surgical excision, recurrence is common, usually due to incomplete excision. Often, the tracts of the cyst will pass near important structures, such as the internal jugular vein, carotid artery, or facial nerve, making complete excision impractical due to the high risk of complications.[10]
See also
References
- Pincus RL (2001). "Congenital neck masses and cysts". Head & Neck Surgery - Otolaryngology (3 ed.). Lippincott Williams & Wilkins: 933.
- Colman R (2008). Toronto Notes. pp. OT33.
- Hong C. "Branchial cleft cyst". eMedicine.com. Retrieved 24 August 2008.
- Shubin N (2009). Your Inner Fish. Vintage. ISBN 978-0-307-27745-9.
- Nahata V (2016). "Branchial Cleft Cyst". Indian Journal of Dermatology. 61 (6): 701. doi:10.4103/0019-5154.193718. PMC 5122306. PMID 27904209.
- "Differential diagnosis of a neck mass". www.uptodate.com. UpToDate. Retrieved 2018-08-18.
- "Branchial Cleft Cyst". missinglink.ucsf.edu. Retrieved 2019-06-26.
- "Duke Embryology - Craniofacial Development". web.duke.edu. Retrieved 2016-09-08.
- "Differential diagnosis of a neck mass". www.uptodate.com. Retrieved 2016-09-08.
- Waldhausen JH (May 2006). "Branchial cleft and arch anomalies in children". Seminars in Pediatric Surgery. 15 (2): 64–9. doi:10.1053/j.sempedsurg.2006.02.002. PMID 16616308.
External links
| Classification | |
|---|---|
| External resources |