Brain positron emission tomography
Brain positron emission tomography is a form of positron emission tomography (PET) that is used to measure brain metabolism and the distribution of exogenous radiolabeled chemical agents throughout the brain. PET measures emissions from radioactively labeled metabolically active chemicals that have been injected into the bloodstream. The emission data from brain PET are computer-processed to produce multi-dimensional images of the distribution of the chemicals throughout the brain.[1]
| Brain positron emission tomography | |
|---|---|
| Medical diagnostics | |
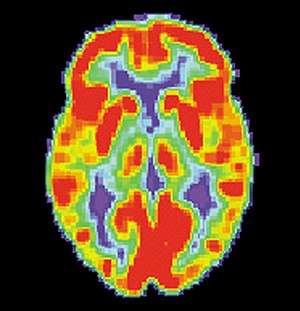 PET scan of a normal brain | |
| ICD-10-PCS | C030 |
Process
The positron emitting radioisotopes used are usually produced by a cyclotron, and chemicals are labeled with these radioactive atoms. The labeled compound, called a radiotracer, is injected into the bloodstream and eventually makes its way to the brain through blood circulation. Detectors in the PET scanner detect the radioactivity as the compound charges in various regions of the brain. A computer uses the data gathered by the detectors to create multi-dimensional (normally 3-dimensional volumetric or 4-dimensional time-varying) images that show the distribution of the radiotracer in the brain. Especially useful are a wide array of ligands used to map different aspects of neurotransmitter activity, with by far the most commonly used PET tracer being a labeled form of glucose, such as fludeoxyglucose (18F).
Advantages and disadvantages
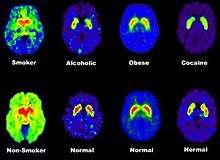
The greatest benefit of PET scanning is that different compounds can show flow and oxygen, and glucose metabolism in the tissues of the working brain. These measurements reflect the amount of brain activity in the various regions of the brain and allow to learn more about how the brain works. PET scans were superior to all other metabolic imaging methods in terms of resolution and speed of completion (as little as 30 seconds), when they first became available. The improved resolution permitted better study to be made as to the area of the brain activated by a particular task. The biggest drawback of PET scanning is that because the radioactivity decays rapidly, it is limited to monitoring short tasks.[2]
Uses
Before the use of functional magnetic resonance imaging (fMRI) became widespread, PET scanning was the preferred method of functional (as opposed to structural) brain imaging, and it still continues to make large contributions to neuroscience. PET scanning is also useful in PET-guided stereotactic surgery and radiosurgery for treatment of intracranial tumors, arteriovenous malformations and other surgically treatable conditions.[4]
PET scanning is also used for diagnosis of brain disease, most notably because brain tumors, strokes, and neuron-damaging diseases which cause dementia (such as Alzheimer's disease) all cause great changes in brain metabolism, which in turn causes easily detectable changes in PET scans. PET is probably most useful in early cases of certain dementias (with classic examples being Alzheimer's disease and Pick's disease) where the early damage is too diffuse and makes too little difference in brain volume and gross structure to change CT and standard MRI images enough to be able to reliably differentiate it from the "normal" range of cortical atrophy which occurs with aging (in many but not all) persons, and which does not cause clinical dementia.
PET is also actively used for multiple sclerosis and other acquired demyelinating syndromes, but mainly for research into pathogenesis instead of diagnosis. They use specific radioligands for microglial activity. Currently is widely used the 18-kDa translocator protein (TSPO).[5] Also combined PET-CT are sometimes performed.[6]
References
- Lars-Goran Nilsson and Hans J. Markowitsch (1999). Cognitive Neuroscience of Memory. Seattle: Hogrefe & Huber Publishers., page 57
- Lars-Goran Nilsson and Hans J. Markowitsch (1999). Cognitive Neuroscience of Memory. Seattle: Hogrefe & Huber Publishers., pg. 60
- Volkow N, Fowler J, Wang G (May 2003). "The addicted human brain: insights from imaging studies". J Clin Invest. 111 (10): 1444–1451. doi:10.1172/JCI200318533. PMC 155054. PMID 12750391.
- Levivier M, Massager N, Wikler D, Lorenzoni J, Ruiz S, Devriendt D, David P, Desmedt F, Simon S, Van Houtte P, Brotchi J, Goldman S (July 2004). "Use of stereotactic PET images in dosimetry planning of radiosurgery for brain tumors: clinical experience and proposed classification". Journal of Nuclear Medicine. 45 (7): 1146–1154. PMID 15235060.
- Airas L, Nylund M, Rissanen E (March 2018). "Evaluation of Microglial Activation in Multiple Sclerosis Patients Using Positron Emission Tomography". Front. Neurol. 9: 181. doi:10.3389/fneur.2018.00181. PMC 5879102. PMID 29632509.
- Malo-Pion C, Lambert R, Décarie JC, Turpin S, Imaging of Acquired Demyelinating Syndrome With 18F-FDG PET/CT. Clinical Nuclear Medicine [05 Dec 2017, 43(2):103-105], DOI: 10.1097/RLU.0000000000001916, PMID 29215409,