Neutron capture therapy of cancer
Neutron capture therapy (NCT) is a noninvasive therapeutic modality for treating locally invasive malignant tumors such as primary brain tumors, recurrent head and neck cancer, and cutaneous and extracutaneous melanomas. It is a two-step procedure: first, the patient is injected with a tumor-localizing drug containing the non-radioactive isotope boron-10 (10B), which has a high propensity to capture thermal neutrons[1]. The cross section of the 10B (3,837 barns) is many times greater than that of the other elements present in tissues such as hydrogen, oxygen, and nitrogen. In the second step, the patient is radiated with epithermal neutrons, the source of which is either a nuclear reactor or, more recently, an accelerator. After losing energy as they penetrate tissue, the neutrons are captured by the 10B, which subsequently emits high-energy alpha particles that can selectively kill those tumor cells that have taken up sufficient quantities of 10B. All of the clinical experience to date with NCT is with the non-radioactive isotope boron-10, and this is known as boron neutron capture therapy (BNCT).[2] At this time, the use of other non-radioactive isotopes, such as gadolinium, has been limited to experimental studies, and to date, it has not been used clinically. BNCT has been evaluated clinically as an alternative to conventional radiation therapy for the treatment of high-grade gliomas, meningiomas, and recurrent, locally advanced cancers of the head and neck region and superficial cutaneous and extracutaneous melanomas.[2][3]
| Neutron capture therapy of cancer | |
|---|---|
| Specialty | oncology |
| Science with neutrons |
|---|
 |
| Foundations |
|
| Neutron scattering |
|
| Other applications |
|
| Infrastructure |
|
| Neutron facilities |
Boron neutron capture therapy
History
After the initial discovery of the neutron in 1932 by Sir James Chadwick, H. J. Taylor in 1935 showed that boron-10 nuclei had a propensity to capture thermal neutrons. This results in nuclear fission of the boron-11 nuclei into stripped down helium-4 nuclei (alpha particles) and lithium-7 ions. In 1936, G.L. Locher, a scientist at the Franklin Institute in Philadelphia, Pennsylvania, recognized the therapeutic potential of this discovery and suggested that neutron capture could be used to treat cancer. W. H. Sweet, from Massachusetts General Hospital, first suggested the technique for treating malignant brain tumors and a trial of BNCT against the most malignant of all brain tumors, glioblastoma multiforme, using borax as the boron delivery agent in 1951.[4] A clinical trial was initiated in a collaboration with Brookhaven National Laboratory[5] in Long Island, New York, U.S.A. and the Massachusetts General Hospital in Boston in 1954.[4]
A number of research groups throughout the world have continued the early groundbreaking work of William Sweet and Ralph Fairchild, and in particular, the pioneering clinical studies of Hiroshi Hatanaka (畠中洋) in Japan. This was followed by clinical trials in a number of other countries including Japan, the United States, Sweden, Finland, Czech Republic, Argentina, and the European Union (centered in the Netherlands). Currently, the program in Japan has transitioned from a reactor neutron source to accelerators, and now a Phase I/II trial is underway to evaluate the safety and therapeutic efficacy of the accelerator neutron sources.
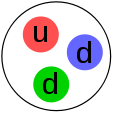
Basic principles
Neutron capture therapy is a binary system that consists of two separate components to achieve its therapeutic effect. Each component in itself is non-tumoricidal, but when combined together they are highly lethal to cancer cells.
_illustration.jpg)
BNCT is based on the nuclear capture and fission reactions that occur when non-radioactive boron-10, which makes up approximately 20% of natural elemental boron, is irradiated with neutrons of the appropriate energy to yield excited boron-11 (11B*). This undergoes instantaneous nuclear fission to produce high-energy alpha particles (4He nuclei) and high-energy lithium-7 (7Li) nuclei. The nuclear reaction is:
- 10B + nth → [11B] *→ α + 7Li + 2.31 MeV
Both the alpha particles and the lithium nuclei produce closely spaced ionizations in the immediate vicinity of the reaction, with a range of 5–9 µm, which is approximately the diameter of the target cell. The lethality of the capture reaction is limited to boron containing cells. BNCT, therefore, can be regarded as both a biologically and a physically targeted type of radiation therapy. The success of BNCT is dependent upon the selective delivery of sufficient amounts of 10B to the tumor with only small amounts localized in the surrounding normal tissues.[6] Thus, normal tissues, if they have not taken up sufficient amounts of boron-10, can be spared from the nuclear capture and fission reactions. Normal tissue tolerance is determined by the nuclear capture reactions that occur with normal tissue hydrogen and nitrogen.
A wide variety of boron delivery agents have been synthesized,[7] but only two of these currently are being used in clinical trials. The first, which has been used primarily in Japan, is a polyhedral borane anion, sodium borocaptate or BSH (Na2B12H11SH), and the second is a dihydroxyboryl derivative of phenylalanine, referred to as boronophenylalanine or BPA. The latter has been used in clinical trials in the United States, Finland, Japan, and, more recently, Argentina and Taiwan. Following administration of either BPA or BSH by intravenous infusion, the tumor site is irradiated with neutrons, the source of which until recently has been specially designed nuclear reactors, but now specially designed accelerators are being used. Until 1994, low-energy (< 0.5 eV) thermal neutron beams were used in Japan[8] and the United States,[4][5] but since they have a limited depth of penetration in tissues, higher energy (>.5eV<10 keV) epithermal neutron beams, which have a greater depth of penetration, have been used in clinical trials in the United States,[9][10] Europe,[11][12] Japan,[13][14] Argentina, Taiwan, and China. In theory BNCT is a highly selective type of radiation therapy that can target tumor cells without causing radiation damage to the adjacent normal cells and tissues. Doses up to 60–70 grays (Gy) can be delivered to the tumor cells in one or two applications compared to 6–7 weeks for conventional fractionated external beam photon irradiation. However, the effectiveness of BNCT is dependent upon a relatively homogeneous cellular distribution of 10B within the tumor, and this is still one of the main unsolved problems that have limited its success.[2]
Radiobiological considerations
The radiation doses delivered to tumor and normal tissues during BNCT are due to energy deposition from three types of directly ionizing radiation that differ in their linear energy transfer (LET), which is the rate of energy loss along the path of an ionizing particle:
1. low-LET gamma rays, resulting primarily from the capture of thermal neutrons by normal tissue hydrogen atoms [1H(n,γ)2H];
2. high-LET protons, produced by the scattering of fast neutrons and from the capture of thermal neutrons by nitrogen atoms [14N(n,p)14C]; and
3. high-LET, heavier charged alpha particles (stripped down helium [4He] nuclei) and lithium-7 ions, released as products of the thermal neutron capture and fission reactions with 10B [10B(n,α)7Li].
Since both tumor and surrounding normal tissues are present in the radiation field, even with an ideal epithermal neutron beam, there will be an unavoidable, nonspecific background dose, consisting of both high- and low-LET radiation. However, a higher concentration of 10B in the tumor will result in it receiving a higher total dose than that of adjacent normal tissues, which is the basis for the therapeutic gain in BNCT.[15] The total radiation dose in Gy delivered to any tissue can be expressed in photon-equivalent units as the sum of each of the high-LET dose components multiplied by weighting factors (Gyw), which depend on the increased radiobiological effectiveness of each of these components.
Clinical dosimetry
Biological weighting factors have been used in all of the recent clinical trials in patients with high-grade gliomas, using boronophenylalanine (BPA) in combination with an epithermal neutron beam. The 10B(n,α)7Li component of the radiation dose to the scalp has been based on the measured boron concentration in the blood at the time of BNCT, assuming a blood: scalp boron concentration ratio of 1.5:1 and a compound biological effectiveness (CBE) factor for BPA in skin of 2.5. A relative biological effectiveness (RBE) or CBE factor of 3.2 has been used in all tissues for the high-LET components of the beam, such as alpha particles. The RBE factor is used to compare the biologic effectiveness of different types of ionizing radiation. The high-LET components include protons resulting from the capture reaction with normal tissue nitrogen, and recoil protons resulting from the collision of fast neutrons with hydrogen.[15] It must be emphasized that the tissue distribution of the boron delivery agent in humans should be similar to that in the experimental animal model in order to use the experimentally derived values for estimation of the radiation doses for clinical radiations.[15][16] For more detailed information relating to computational dosimetry and treatment planning, interested readers are referred to a comprehensive review on this subject.[17]
Boron delivery agents
The development of boron delivery agents for BNCT began in the early 1960s and is an ongoing and difficult task. A number of boron-10 containing delivery agents have been prepared for potential use in BNCT.[7][18][19] The most important requirements for a successful boron delivery agent are:
- low systemic toxicity and normal tissue uptake with high tumor uptake and concomitantly high tumor: to brain (T:Br) and tumor: to blood (T:Bl) concentration ratios (> 3–4:1);
- tumor concentrations in the range of ~20 µg 10B/g tumor;
- rapid clearance from blood and normal tissues and persistence in tumor during BNCT.
However, as of 2019 no single boron delivery agent fulfills all of these criteria. With the development of new chemical synthetic techniques and increased knowledge of the biological and biochemical requirements needed for an effective agent and their modes of delivery, a wide variety of new boron agents has emerged (see examples in Table 1), but only two of these, boronophenylalanine (BPA) and sodium borocaptate (BSH) have been used clinically.[2]
| Boric acid | Boronated unnatural amino acids |
| Boron nitride nanotubes | Boronated VEGF |
| Boron-containing immunoliposomes and liposomes | Carboranyl nucleosides |
| Boron-containing Lipiodol | Carboranyl porphyrazines |
| Boron-containing nanoparticles | Carboranyl thymidine analogues |
| Boronated co-polymers | Decaborone (GB10) |
| Boronated cyclic peptides | Dodecaborate cluster lipids and cholesterol derivatives |
| Boronated DNAc intercalators | Dodecahydro-closo-dodecaborate clusters |
| Boronated EGF and anti-EGFR MoAbs | Linear and cyclic peptides |
| Boronated polyamines | Polyanionic polymers |
| Boronated porphyrins | Transferrin-polyethylene glycol liposomes |
| Boronated sugars |
aThe delivery agents are not listed in any order that indicates their potential usefulness for BNCT. None of these agents have been evaluated clinically.
bSee Barth, R.F., Mi, P., and Yang, W., Boron delivery agents for neutron capture therapy of cancer, Cancer Communications, 38:35 (doi: 10.1186/s40880-018-0299-7), 2018 for an updated review.
cThe abbreviations used in this table are defined as follows: BNCT, boron neutron capture therapy; DNA, deoxyribonucleic acid; EGF, epidermal growth factor; EGFR, epidermal growth factor receptor; MoAbs, monoclonal antibodies; VEGF, vascular endothelial growth factor.
The major challenge in the development of boron delivery agents has been the requirement for selective tumor targeting in order to achieve boron concentrations (20-50 µg/g tumor) sufficient to produce therapeutic doses of radiation at the site of the tumor with minimal radiation delivered to normal tissues. The selective destruction of brain tumor (glioma) cells in the presence of normal cells represents an even greater challenge compared to malignancies at other sites in the body, since malignant gliomas are highly infiltrative of normal brain, histologically diverse and heterogeneous in their genomic profile. In principle, NCT is a radiation therapy that could selectively deliver lethal doses of radiation to tumor cells while sparing adjacent normal cells.[4]
Gadolinium neutron capture therapy (Gd NCT)
There also has been interest in the possible use of gadolinium-157 (157Gd) as a capture agent for NCT for the following reasons:[20] First, and foremost, has been its very high neutron capture cross section of 254,000 barns. Second, gadolinium compounds, such as Gd-DTPA (gadopentetate dimeglumine Magnevist®), have been used routinely as contrast agents for magnetic resonance imaging (MRI) of brain tumors and have shown high uptake by brain tumor cells in tissue culture (in vitro).[21] Third, gamma rays and internal conversion and Auger electrons are products of the 157Gd (n,γ)158Gd capture reaction (157Gd + nth (0.025eV) → [158Gd] → 158Gd + γ + 7.94 MeV). Although the gamma rays have longer pathlengths, orders of magnitude greater depths of penetration compared with alpha particles, the other radiation products (internal conversion and Auger electrons) have pathlengths of approximately one cell diameter and can directly damage DNA. Therefore, it would be highly advantageous for the production of DNA damage if the 157Gd were localized within the cell nucleus. However, the possibility of incorporating gadolinium into biologically active molecules is very limited and only a small number of potential delivery agents for Gd NCT have been evaluated.[22][23] Relatively few studies with Gd have been carried out in experimental animals compared to the large number with boron containing compounds (Table 1), which have been synthesized and evaluated in experimental animals (in vivo). Although in vitro activity has been demonstrated using the Gd-containing MRI contrast agent Magnevist® as the Gd delivery agent,[24] there are very few studies demonstrating the efficacy of Gd NCT in experimental animal tumor models,[23][25] and, as evidenced by a lack of citations in the literature, Gd NCT has not, as of 2019, been used clinically in humans.
Neutron sources
Nuclear reactors
Until recently neutron sources for NCT have been limited to nuclear reactors and in the present section we only will summarize information that is described in more detail in a 2009 review.[26] Reactor-derived neutrons are classified according to their energies as thermal (En <0.5 eV), epithermal (0.5 eV <En <10 keV), or fast (En >10 keV). Thermal neutrons are the most important for BNCT since they usually initiate the 10B(n,α)7Li capture reaction. However, because they have a limited depth of penetration, epithermal neutrons, which lose energy and fall into the thermal range as they penetrate tissues, are not used for clinical therapy other than for skin tumors such as melanoma.
A number of nuclear reactors with very good neutron beam quality have been developed and used clinically. These include:
- Kyoto University Research Reactor Institute (KURRI) in Kumatori, Japan;
- the Massachusetts Institute of Technology Research Reactor (MITR);
- the FiR1 (Triga Mk II) research reactor at VTT Technical Research Centre, Espoo, Finland;
- the RA-6 CNEA reactor in Bariloche, Argentina;
- the High Flux Reactor (HFR) at Petten in the Netherlands; and
- Tsing Hua Open-pool Reactor (THOR) at the National Tsing Hua University, Hsinchu, Taiwan.
- JRR-4 at Japan Atomic Energy Agency, Tokai, JAPAN
However, as of April 2019, only the RA-6 reactor in Argentina and the THOR reactor in Taiwan currently are being used for clinical studies.
Although not currently being used for BNCT, the neutron irradiation facility at the MITR represented the state of the art in epithermal beams for NCT with the capability of completing a radiation field in 10–15 minutes with close to the theoretically maximum ratio of tumor to normal tissue dose. Unfortunately, however, no clinical studies currently are being carried out at the HFR and the MITR. The operation of the BNCT facility at the Finnish FiR1 research reactor (Triga Mk II), treating patients since 1999, was terminated in 2012 due to a variety of reasons, one of which was financial.[27] It is anticipated that future clinical studies in Finland will utilize an accelerator neutron source designed and fabricated in the United States by Neutron Therapeutics, Danvers, Massachusetts. Finally, a low-power "in-hospital" compact nuclear reactor has been designed and built in Beijing, China, and at this time has only been used to treat a small number of patients with cutaneous melanomas.[28][29]
Accelerators
Accelerators also can be used to produce epithermal neutrons and accelerator-based neutron sources (ABNS) are being developed in a number of countries. Interested readers are referred to two recently published reviews relating to accelerator neutron sources[30][31] and abstracts of the 17th and 18th International Congresses[32][33] on Neutron Capture Therapy for more information on this subject. For ABNS, one of the more promising nuclear reactions involves bombarding a 7Li target with high-energy protons. An experimental BNCT facility, using a thick lithium solid target, was developed in the early 1990s at the University of Birmingham in the UK, but to date no clinical or experimental animal studies have been carried out at this facility, which makes use of a high-current Dynamitron accelerator originally supplied by Radiation Dynamics.
Recently, a cyclotron-based neutron source (C-BENS) has been developed by Sumitomo Heavy Industries (SHI) in Japan.[34] It has been installed at the Particle Radiation Oncology Research Center of Kyoto University in Kumatori, Japan. It now is being used in a Phase I clinical trial to evaluate its safety for treating patients with high-grade gliomas. A second one has been constructed by High Energy Accelerator Organization (KEK) with Mitsubishi Heavy Industrial, and Toshiba, for use at University of Tsukuba in Japan. A third one is being built by CICS with Hitachi for use in Tokyo. A fourth accelerator, manufactured by SHI, is located at the Southern Tohoku BNCT Research Center in Fukushima prefecture in Japan and is being used in a Phase II clinical trial for BNCT of recurrent brain tumors and head and neck cancer. Finally, a fifth one, which as of Spring 2019 has been installed at Helsinki University Hospital in Finland.[35] This accelerator was designed and fabricated by Neutron Therapeutics in Danvers, Massachusetts and it is anticipated that clinical use will begin in the latter half of 2019. It will be important to determine how these ABNS compare to BNCT that has been carried out in the past using nuclear reactors as the neutron source.[35]
Clinical studies of BNCT for brain tumors
Early studies in the US and Japan
It was not until the 1950s that the first clinical trials were initiated by Farr at the Brookhaven National Laboratory (BNL) in New York[5] and by Sweet and Brownell at the Massachusetts General Hospital (MGH) using the Massachusetts Institute of Technology (MIT) nuclear reactor (MITR)[36] and several different low molecular weight boron compounds as the boron delivery agent. However, the results of these studies were disappointing, and no further clinical trials were carried out in the United States until the 1990s.
Following a two-year Fulbright fellowship in Sweet's laboratory at the MGH, clinical studies were initiated by Hiroshi Hatanaka in Japan in 1967. He used a low-energy thermal neutron beam, which had low tissue penetrating properties, and sodium borocaptate (BSH) as the boron delivery agent, which had been evaluated as a boron delivery agent by Albert Soloway at the MGH.[37] In Hatanaka's procedure,[38] as much as possible of the tumor was surgically resected ("debulking"), and at some time thereafter, BSH was administered by a slow infusion, usually intra-arterially, but later intravenously. Twelve to 14 hours later, BNCT was carried out at one or another of several different nuclear reactors using low-energy thermal neutron beams. The poor tissue-penetrating properties of the thermal neutron beams necessitated reflecting the skin and raising a bone flap in order to directly irradiate the exposed brain, a procedure first used by Sweet and his collaborators.
Approximately 200+ patients were treated by Hatanaka, and subsequently by his associate, Nakagawa.[8] Due to the heterogeneity of the patient population, in terms of the microscopic diagnosis of the tumor and its grade, size, and the ability of the patients to carry out normal daily activities (Karnofsky performance status), it was not possible to come up with definitive conclusions about therapeutic efficacy. However, the survival data were no worse than those obtained by standard therapy at the time, and there were several patients who were long-term survivors, and most probably they were cured of their brain tumors.[8]
More recent clinical studies in the US and Japan
BNCT of patients with brain tumors was resumed in the United States in the mid-1990s by Chanana, Diaz, and Coderre[9] and their co-workers at the Brookhaven National Laboratory Medical Research Reactor (BMRR) and at Harvard/Massachusetts Institute of Technology (MIT) using the MIT Research Reactor (MITR).[10] For the first time, BPA was used as the boron delivery agent, and patients were irradiated with a collimated beam of higher energy epithermal neutrons, which had greater tissue-penetrating properties than thermal neutrons. A research group headed up by Zamenhof at the Beth Israel Deaconess Medical Center/Harvard Medical School and MIT was the first to use an epithermal neutron beam for clinical trials. Initially patients with cutaneous melanomas were treated and this was expanded to include patients with brain tumors, specifically melanoma metastatic to the brain and primary glioblastomas (GBMs). Included in the research team were Otto Harling at MIT and the Radiation Oncologist Paul Busse at the Beth Israel Deaconess Medical Center in Boston. A total of 22 patients were treated by the Harvard-MIT research group. Five patients with cutaneous melanomas were treated using an epithermal neutron beam at the MIT research reactor (MITR-II) and subsequently patients with brain tumors were treated using a redesigned beam at the MIT reactor which possessed far superior characteristics to the original MITR-II beam, and BPA as the capture agent. The clinical outcome of the cases treated at Harvard-MIT has been summarized by Busse.[10] Although the treatment was well tolerated, there were no significant differences in the mean survival times of patients that had received BNCT compared to those who received conventional external beam X-irradiation.[10]
Miyatake and Kawabata at Osaka Medical College in Japan[13][14] have carried out extensive clinical studies employing BPA (500 mg/kg) either alone or in combination with BSH (100 mg/kg), infused intravenously (i.v.) over 2 h, followed by neutron irradiation at Kyoto University Research Reactor Institute (KURRI). The Mean Survival Time (MST) of 10 patients in the first of their trials was 15.6 months, with one long-term survivor (>5 years).[14] Based on experimental animal data,[39] which showed that BNCT in combination with X-irradiation produced enhanced survival compared to BNCT alone, Miyatake and Kawabata combined BNCT, as described above, with an X-ray boost.[13] A total dose of 20 to 30 Gy was administered, divided into 2 Gy daily fractions. The MST of this group of patients was 23.5 months and no significant toxicity was observed, other than hair loss (alopecia). However, a significant subset of these patients, a high proportion of which had small cell variant glioblastomas, developed cerebrospinal fluid dissemination of their tumors.[40] In another Japanese trial, carried out by Yamamoto et al., BPA and BSH were infused over 1 h, followed by BNCT at the Japan Research Reactor (JRR)-4 reactor.[41] Patients subsequently received an X-ray boost after completion of BNCT. The overall median survival time (MeST) was 27.1 months, and the 1 year and 2-year survival rates were 87.5 and 62.5%, respectively. Based on the reports of Miyatake, Kawabata, and Yamamoto, it appears that combining BNCT with an X-ray boost can produce a significant therapeutic gain. However, further studies are needed to optimize this combined therapy alone or in combination with other approaches including chemo- and immunotherapy, and to evaluate it using a larger patient population.[42]
Clinical studies in Finland
A team of clinicians led by Heikki Joensuu and Leena Kankaanranta and nuclear engineers led by Iro Auterinen and Hanna Koivunoro at the Helsinki University Central Hospital and VTT Technical Research Center of Finland have treated approximately 200+ patients with recurrent malignant gliomas (glioblastomas) and head and neck cancer who had undergone standard therapy, recurred, and subsequently received BNCT at the time of their recurrence using BPA as the boron delivery agent.[11][12] The median time to progression in patients with gliomas was 3 months, and the overall MeST was 7 months. It is difficult to compare these results with other reported results in patients with recurrent malignant gliomas, but they are a starting point for future studies using BNCT as salvage therapy in patients with recurrent tumors. Due to a variety of reasons, including financial,[43] no further studies have been carried out at this facility, which is scheduled for decommissioning. However, a new facility for BNCT treatment will be opened at Meilahti Tower Hospital in 2019 using an accelerator designed and fabricated by Neutron Therapeutics. This is the first BNCT accelerator specifically designed to be used in a hospital, and the BNCT treatment and clinical studies will be continued there. Both Finnish and foreign patients are expected to be treated at the facility.[44][45][46]
| Reactor Facility* | No. of patients & duration of trial | Delivery agent | Median survival time (months) | Reference no. |
|---|---|---|---|---|
| BMRR, U.S.A | 53 (1994–1999) | BPA 250–330 mg/kg | 12.8 | [9] |
| MITR, MIT, U.S.A. | 20 (1996–1999) | BPA 250 or 350 mg/kg | 11.1 | [10] |
| KURRI, Japan | 40 (1998–2008) | BPA 500 mg/kg | 23.5 (primary + X-ray) | [13][14] |
| JRR4, Japan | 15 (1998–2007) | BPA 250 mg/kg + BSH 5 g | 10.8 (recurrent), 27.1 (+ X-ray) | [41] |
| R2-0, Studsvik Medical AB, Sweden | 30 (2001–2007) | BPA 900 mg/kg | 17.7 (primary) | [47][48] |
| FiR1, Finland | 50 (1999–2012) | BPA 290–400 mg/kg | 11.0 – 21.9 (primary), 7.0 (recurrent) | [11] |
| HFR, Netherlands | 26 (1997–2002) | BSH 100 mg/kg | 10.4 – 13.2 | [49] |
| * A more comprehensive compilation of data relating to BNCT clinical trials can be found in Radiation Oncology 7:146–167, 2012[2] | ||||
Clinical studies in Sweden
Finally, to conclude this section, the following is a brief summary of a clinical trial that was carried out by Stenstam, Sköld, Capala and their co-workers in Sweden using BPA and an epithermal neutron beam at the Studsvik nuclear reactor, which had greater tissue penetration properties than the thermal beams originally used in Japan. This study differed significantly from all previous clinical trials in that the total amount of BPA administered was increased (900 mg/kg), and it was infused i.v. over 6 hours. This was based on experimental animal studies in glioma bearing rats demonstrating enhanced uptake of BPA by infiltrating tumor cells following a 6-hour infusion.[37][47][48][50] The longer infusion time of the BPA was well tolerated by the 30 patients who were enrolled in this study. All were treated with 2 fields, and the average whole brain dose was 3.2–6.1 Gy (weighted), and the minimum dose to the tumor ranged from 15.4 to 54.3 Gy (w). There has been some disagreement among the Swedish investigators regarding the evaluation of the results. Based on incomplete survival data, the MeST was reported as 14.2 months and the time to tumor progression was 5.8 months.[47] However, more careful examination[48] of the complete survival data revealed that the MeST was 17.7 months compared to 15.5 months that has been reported for patients who received standard therapy of surgery, followed by radiotherapy (RT) and the drug temozolomide (TMZ).[51] Furthermore, the frequency of adverse events was lower after BNCT (14%) than after radiation therapy (RT) alone (21%) and both of these were lower than those seen following RT in combination with TMZ. If this improved survival data, obtained using the higher dose of BPA and a 6-hour infusion time, can be confirmed by others, preferably in a randomized clinical trial, it could represent a significant step forward in BNCT of brain tumors, especially if combined with a photon boost.
Clinical Studies of BNCT for extracranial tumors
Head and neck cancers
The single most important clinical advance over the past 15 years[52] has been the application of BNCT to treat patients with recurrent tumors of the head and neck region who had failed all other therapy. These studies were first initiated by Kato et al. in Japan[53][52] and subsequently followed by several other Japanese groups and by Kankaanranta, Joensuu, Auterinen, Koivunoro and their co-workers in Finland.[12] All of these studies employed BPA as the boron delivery agent, usually alone but occasionally in combination with BSH. A very heterogeneous group of patients with a variety of histopathologic types of tumors have been treated, the largest number of which had recurrent squamous cell carcinomas. Kato et al. have reported on a series of 26 patients with far-advanced cancer for whom there were no further treatment options.[52] Either BPA + BSH or BPA alone were administered by a 1 or 2 h i.v. infusion, and this was followed by BNCT using an epithermal beam. In this series, there were complete regressions in 12 cases, 10 partial regressions, and progression in 3 cases. The MST was 13.6 months, and the 6-year survival was 24%. Significant treatment related complications ("adverse" events) included transient mucositis, alopecia and, rarely, brain necrosis and osteomyelitis.
Kankaanranta et al. have reported their results in a prospective Phase I/II study of 30 patients with inoperable, locally recurrent squamous cell carcinomas of the head and neck region.[12] Patients received either two or, in a few instances, one BNCT treatment using BPA (400 mg/kg), administered i.v. over 2 hours, followed by neutron irradiation. Of 29 evaluated patients, there were 13 complete and 9 partial remissions, with an overall response rate of 76%. The most common adverse event was oral mucositis, oral pain, and fatigue. Based on the clinical results, it was concluded that BNCT was effective for the treatment of inoperable, previously irradiated patients with head and neck cancer. Some responses were durable but progression was common, usually at the site of the previously recurrent tumor. As previously indicated in the section on neutron sources, all clinical studies have ended in Finland, based on a variety of reasons including economic difficulties of the two companies directly involved, VTT and Boneca. However, there are plans to resume clinical studies using an accelerator neutron source designed and fabricated by Neutron Therapeutics. Finally, a group in Taiwan, led by Ling-Wei Wang and his co-workers at the Taipei Veterans General Hospital, have treated 17 patients with locally recurrent head and neck cancers at the Tsing Hua Open-pool Reactor (THOR) of the National Tsing Hua University.[54] Two-year overall survival was 47% and two-year loco-regional control was 28%. Further studies are in progress to further optimize their treatment regimen.
Other types of tumors
Melanoma and extramammary Paget's disease
Other extracranial tumors that have been treated include malignant melanomas, which originally was carried out in Japan by the late Yutaka Mishima and his clinical team in the Department of Dermatology at Kobe University[55] using BPA and a thermal neutron beam. It is important to point out that it was Mishima who first used BPA as a boron delivery agent and this subsequently was extended to other types of tumors based on the experimental studies of Coderre et al. at the Brookhaven National Laboratory.[56] Local control was achieved in almost all patients, and some were cured of their melanomas. More recently, Junichi Hiratsuka and his colleagues at Kawasaki Medical School Hospital have treated patients with melanoma of the head and neck region, vulva, and extramammary Paget's disease of the genital region with impressive clinical results.[57] The first clinical trial of BNCT in Argentina for the treatment of melanomas was performed in October 2003[58] and since then several patients with cutaneous melanomas have been treated as part of a Phase II clinical trial at the RA-6 nuclear reactor in Bariloche. The neutron beam has a mixed thermal-hyperthermal neutron spectrum that can be use to treat superficial tumors.[58] Finally, as recently reported,[29] the in-hospital neutron irradiator (IHNI) in Beijing has been used to treat three patients with cutaneous melanomas with a complete response of the primary lesion and no evidence of late radiation injury during a 24+-month follow-up period. The ultimate aim of the group in Beijing is to initiate a multi-institutional randomized clinical trial to evaluate BNCT of melanomas.[28][29]
Colorectal cancer
Two patients with colon cancer, which had spread to the liver, have been treated by Zonta and his co-workers at the University of Pavia in Italy.[59] The first was treated in 2001 and the second in mid-2003. The patients received an i.v. infusion of BPA, followed by removal of the liver (hepatectomy), which was irradiated outside of the body (extracorporeal BNCT) and then re-transplanted into the patient. The first patient did remarkably well and survived for over 4 years after treatment, but the second died within a month of cardiac complications.[60] Clearly, this is a very challenging approach for the treatment of hepatic metastases, and it is unlikely that it will ever be widely used. Nevertheless, the good clinical results in the first patient established proof of principle. Finally, Yanagie and his colleagues at Meiji Pharmaceutical University in Japan have treated several patients with recurrent rectal cancer using BNCT. Although no long-term results have been reported, there was evidence of short-term clinical responses.[61]
Conclusions
BNCT represents a joining together of nuclear technology, chemistry, biology, and medicine to treat brain tumors, recurrent head and neck cancers, and cutaneous and extracutaneous melanomas. Sadly, the lack of progress in developing more effective treatments for these tumors has been part of the driving force that continues to propel research in this field. BNCT may be best suited as an adjunctive treatment, used in combination with other modalities, including surgery, chemotherapy, immunotherapy, and external beam radiation therapy for those malignancies, whether primary or recurrent, for which there are no effective therapies. Clinical studies have demonstrated the safety of BNCT. The challenge facing clinicians and researchers is how to move forward. A significant advantage of BNCT is the potential ability to selectively deliver a radiation dose to the tumor with a much lower dose to surrounding normal tissues. This is an important feature that makes BNCT particularly attractive for salvage therapy of patients with a variety of malignancies who already have been heavily irradiated. Although it may be only palliative, BNCT can produce striking clinical responses, as evidenced by the experiences of several groups treating patients with recurrent, therapeutically refractory head and neck cancers.
Challenges that need to be addressed include:
- Optimizing the dosing and delivery paradigms and administration of BPA and BSH.
- The development of more tumor-selective boron delivery agents for BNCT.
- Accurate, real time dosimetry to better estimate the radiation doses delivered to the tumor and normal tissues.
- Evaluation of recently constructed accelerator-based neutron sources as an alternative to nuclear reactors.
For a more detailed discussion of these challenges and their solutions in BNCT, readers are referred to the published abstracts of the 17th and 18th International Congresses on Neutron Capture Therapy[32][33], two reviews on the current status of BNCT[2][3], and a recent Commentary that provides a realistic appraisal of the future of BNCT. If the problems enumerated above can be solved BNCT could have an important role in twenty-first century cancer treatment of those malignancies that are loco-regional and that are presently incurable by other therapeutic modalities.[62][63]
See also
- Particle therapy, Neutrons, protons, or heavy ions (e.g. carbon)
References
- "The Roles of Radiation, Neutrons, and N-Ray in Medicine". Phoenix | High Flux Neutron Generators. Retrieved 13 June 2019.
- Barth, R.F.; Vicente, M.G.H.; Harling, O.K.; Kiger, W.S.; Riley, K.J.; Binns, P.J.; Wagner, F.M.; Suzuki, M.; Aihara, T.; Kato, I.; Kawabata, S. (2012). "Current status of boron neutron capture therapy of high grade gliomas and recurrent head and neck cancer". Radiation Oncology. 7: 146. doi:10.1186/1748-717X-7-146. PMC 3583064. PMID 22929110.
- Moss, R.L. (2014). "Critical review with an optimistic outlook on boron neutron capture therapy (BNCT)". Applied Radiation and Isotopes. 88: 2–11. doi:10.1016/j.apradiso.2013.11.109. PMID 24355301.
- Sweet, W.H. (1951). "The uses of nuclear disintegration in the diagnosis and treatment of brain tumor". New England Journal of Medicine. 245 (23): 875–8. doi:10.1056/NEJM195112062452301. PMID 14882442.
- Farr, L.E.; Sweet, W.H.; Robertson, J.S.; Foster, C.G.; Locksley, H.B.; Sutherland, D.L.; Mendelsohn, M.L.; Stickley, E.E. (1954). "Neutron capture therapy with boron in the treatment of glioblastoma multiforme". The American Journal of Roentgenology, Radium Therapy, and Nuclear Medicine. 71 (2): 279–93. PMID 13124616.
- Barth, R.F.; Coderre, J.A.; Vicente, M.G.H.; Blue, T.E. (2005). "Boron neutron capture therapy of cancer: Current status and future prospects". Clinical Cancer Research. 11 (11): 3987–4002. doi:10.1158/1078-0432.CCR-05-0035. PMID 15930333.
- Vicente, M.G.H. (2006). "Boron in medicinal chemistry". Anti-Cancer Agents in Medicinal Chemistry. 6 (2): 73. doi:10.2174/187152006776119162.
- Nakagawa, Y.; Pooh, K.; Kobayashi, T.; Kageji, T.; Uyama, S.; Matsumura, A.; Kumada, H. (2003). "Clinical review of the Japanese experience with boron neutron capture therapy and a proposed strategy using epithermal neutron beams". Journal of Neuro-Oncology. 62 (1–2): 87–99. doi:10.1023/A:1023234902479. PMID 12749705.
- Diaz, A.Z. (2003). "Assessment of the results from the phase I/II boron neutron capture therapy trials at the Brookhaven National Laboratory from a clinician's point of view". Journal of Neuro-Oncology. 62 (1–2): 101–9. doi:10.1023/A:1023245123455. PMID 12749706.
- Busse, P.M.; Harling, O.K.; Palmer, M.R.; Kiger, W.S.; Kaplan, J.; Kaplan, I.; Chuang, C.F.; Goorley, J.T.; et al. (2003). "A critical examination of the results from the Harvard-MIT NCT program phase I clinical trial of neutron capture therapy for intracranial disease". Journal of Neuro-Oncology. 62 (1–2): 111–21. doi:10.1007/BF02699938. PMID 12749707.
- Kankaanranta, L.; Seppälä, T.; Koivunoro, H.; Välimäki, P.; Beule, A.; Collan, J.; Kortesniemi, M.; Uusi-Simola, J.; et al. (2011). "L-Boronophenylalanine-mediated boron neutron capture therapy for malignant glioma progressing after external beam radiation therapy: A Phase I study". International Journal of Radiation Oncology • Biology • Physics. 80 (2): 369–76. doi:10.1016/j.ijrobp.2010.02.031. PMID 21236605.
- Kankaanranta, L.; Seppälä, T.; Koivunoro, H.; Saarilahti, K.; Atula, T.; Collan, J.; Salli, E.; Kortesniemi, M.; et al. (2012). "Boron neutron capture therapy in the treatment of locally recurred head-and-neck cancer: Final analysis of a Phase I/II trial". International Journal of Radiation Oncology • Biology • Physics. 82 (1): e67–75. doi:10.1016/j.ijrobp.2010.09.057. PMID 21300462.
- Kawabata, S.; Miyatake, S.-I.; Kuroiwa, T.; Yokoyama, K.; Doi, A.; Iida, K.; Miyata, S.; Nonoguchi, N.; et al. (2009). "Boron neutron capture therapy for newly diagnosed glioblastoma". Journal of Radiation Research. 50 (1): 51–60. Bibcode:2009JRadR..50...51K. doi:10.1269/jrr.08043. PMID 18957828.
- Miyatake, S.-I.; Kawabata, S.; Yokoyama, K.; Kuroiwa, T.; Michiue, H.; Sakurai, Y.; Kumada, H.; Suzuki, M.; et al. (2008). "Survival benefit of boron neutron capture therapy for recurrent malignant gliomas". Journal of Neuro-Oncology. 91 (2): 199–206. doi:10.1007/s11060-008-9699-x. PMID 18813875.
- Coderre, J.A.; Morris, G.M. (1999). "The radiation biology of boron neutron capture therapy". Radiation Research. 151 (1): 1–18. Bibcode:1999RadR..151....1C. doi:10.2307/3579742. JSTOR 3579742. PMID 9973079.
- Ono, Koji (28 March 2016). "An analysis of the structure of the compound biological effectiveness factor". Journal of Radiation Research. 57 (S1): i83–i89. Bibcode:2016JRadR..57I..83O. doi:10.1093/jrr/rrw022. PMC 4990111. PMID 27021218.
- Nigg, D.W. (2003). "Computational dosimetry and treatment planning considerations for neutron capture therapy". Journal of Neuro-Oncology. 62 (1–2): 75–86. doi:10.1023/A:1023241022546. PMID 12749704.
- Soloway, A.H., Tjarks, W., Barnum, B.A., Rong, F-G., Barth, R.F., Codogni, I.M., and Wilson, J.G.: The chemistry of neutron capture therapy. Chemical Rev 98: 1515-1562, 1998.
- Barth, R.F.; Mi, P.; Yang, W. (2018). "Boron delivery agents for neutron capture therapy of cancer". Cancer Communications. 38 (35): 35. doi:10.1186/s40880-018-0299-7. PMC 6006782. PMID 29914561.
- Cerullo, N.; Bufalino, D.; Daquino, G. (2009). "Progress in the use of gadolinium for NCT". Applied Radiation and Isotopes. 67 (7–8): S157–60. doi:10.1016/j.apradiso.2009.03.109. PMID 19410468.
- Yasui, L.S.; Andorf, C.; Schneider, L.; Kroc, T.; Lennox, A.; Saroja, K.R. (2008). "Gadolinium neutron capture in glioblastoma multiforme cells". International Journal of Radiation Biology. 84 (12): 1130–9. doi:10.1080/09553000802538092. PMID 19061138.
- Nemoto, H.; Cai, J.; Nakamura, H.; Fujiwara, M.; Yamamoto, Y. (1999). "The synthesis of a carborane gadolinium–DTPA complex for boron neutron capture therapy". Journal of Organometallic Chemistry. 581 (1–2): 170–5. doi:10.1016/S0022-328X(99)00049-2.
- Tokumitsu, H.; Hiratsuka, J.; Sakurai, Y.; Kobayashi, T.; Ichikawa, H.; Fukumori, Y. (2000). "Gadolinium neutron-capture therapy using novel gadopentetic acid–chitosan complex nanoparticles: In vivo growth suppression of experimental melanoma solid tumor". Cancer Letters. 150 (2): 177–82. doi:10.1016/S0304-3835(99)00388-2. PMID 10704740.
- De Stasio, G.; Rajesh, D.; Ford, J.M.; Daniels, M.J.; Erhardt, R.J.; Frazer, B.H.; Tyliszczak, T.; Gilles, M.K.; et al. (2006). "Motexafin-gadolinium taken up in vitro by at least 90% of glioblastoma cell nuclei". Clinical Cancer Research. 12 (1): 206–13. doi:10.1158/1078-0432.CCR-05-0743. PMID 16397044.
- Geninatti-Crich, S.; Alberti, D.; Szabo, I.; Deagostino, A.; Toppino, A.; Barge, A.; Ballarini, F.; Bortolussi, S.; et al. (2011). "MRI-guided neutron capture therapy by use of a dual gadolinium/boron agent targeted at tumour cells through upregulated low-density lipoprotein transporters". Chemistry. 17 (30): 8479–86. doi:10.1002/chem.201003741. hdl:2318/130944. PMID 21671294.
- Harling, O.K. (2009). "Fission reactor based epithermal neutron irradiation facilities for routine clinical application in BNCT—Hatanaka memorial lecture". Applied Radiation and Isotopes. 67 (7–8): S7–11. doi:10.1016/j.apradiso.2009.03.095. PMID 19428265.
- Koivunoro, H.; Gonzalez, S.; Provenzano, L.; Kankaanranta, L.; Joensuu, H. (28 October 2018). 18th International Congress on Neutron Capture Therapy. Taipei, Taiwan: International Congress on Neutron Capture Therapy. pp. 122–124.
- Zhang, Zizhu; Liu, Tong (2018). "A review of the development of In-Hospital Neutron Irradiator-1 and boron neutron capture therapy clinical research on malignant melanoma". Ther. Radiol. Oncol. 2 (49): 49. doi:10.21037/tro.2018.10.03.
- Yong, Z.; Song, Z.; Zhou, Y.; Liu, T.; Zhang, Z.; Zhao, Y.; Chen, Y.; Jin, C.; et al. (2016). "Boron neutron capture therapy for malignant melanoma: first clinical case report in China". Chin. J. Cancer Res. 28: 1–7. doi:10.21147/j.issn.1000-9604.2016.06.00 (inactive 14 December 2019).
- Naito, Fujio (2018). "Introduction to accelerators for boron neutron capture therapy". Ther. Radiol. Oncol. 2 (54): 54. doi:10.21037/tro.2018.10.11.
- Kiyanagi, Yosshiaki (2018). "Accelerator-based neutron source for boron neutron capture therapy". Ther. Radiol. Oncol. 2 (55): 55. doi:10.21037/tro.2018.10.05.
- Jalisatgi, S. (ed.). "ICNCT-17 Abstract Book". www.icnct17.org. Retrieved 4 January 2017.
- "18th International Congress on Neutron Capture Therapy Abstract Book". www.icnct18.org. Retrieved 17 April 2019.
- Mitsumoto T, Yajima S, Tsutsui H, et al. Cyclotron-based neutron source for BNCT (PDF). New Challenges in Neutron Capture Therapy 2010: Proceedings of the 14th International Congress on Neutron Capture Therapy. Buenos Aires. pp. 519–22. Archived from the original (PDF) on 29 October 2013.
- "Novel Accelerator-Based BNCT Suite to be Delivered to a Top European Cancer Hospital".
- Sweet WH (1983). Practical problems in the past in the use of boron-slow neutron capture therapy in the treatment of glioblastoma multiforme. Proceedings of the First International Symposium on Neutron Capture Therapy. pp. 376–8.
- Barth, R.F. (2015). "From the laboratory to the clinic: How translational studies in animals have lead [sic] to clinical advances in boron neutron capture therapy". Appl Radiat Isotopes. 106: 22–28. doi:10.1016/j.apradiso.2015.06.016. PMID 26149807.
- Hatanaka, H.; Nakagawa, Y. (1994). "Clinical results of long-surviving brain tumor patients who underwent boron neutron capture therapy". International Journal of Radiation Oncology • Biology • Physics. 28 (5): 1061–6. doi:10.1016/0360-3016(94)90479-0. PMID 8175390.
- Barth, R.F.; Grecula, J.C.; Yang, W.; Rotaru, J.H.; Nawrocky, M.; Gupta, N.; Albertson, B.J.; Ferketich, A.K.; et al. (2004). "Combination of boron neutron capture therapy and external beam radiotherapy for brain tumors". International Journal of Radiation Oncology • Biology • Physics. 58 (1): 267–77. doi:10.1016/S0360-3016(03)01613-4. PMID 14697448.
- Kondo, N.; Barth, R.F.; Miyatake, S.-I.; Kawabata, S.; Suzuki, M.; Ono, K.; Lehman, N.L. (2017). "Cerebrospinal fluid dissemination of high-grade gliomas following boron neutron capture therapy (BNCT) occurs more frequently in the small cell subtype of IDH1R132H mutation-negative glioblastoma". Journal of Neuro-Oncology. 133 (1): 107–18. doi:10.1007/s11060-017-2408-x. PMC 5786264. PMID 28534152.
- Yamamoto, T.; Nakai, K.; Nariai, T.; Kumada, H.; Okumura, T.; Mizumoto, M.; Tsuboi, K.; Zaboronok, A.; et al. (2011). "The status of Tsukuba BNCT trial: BPA-based boron neutron capture therapy combined with X-ray irradiation". Applied Radiation and Isotopes. 69 (12): 1817–8. doi:10.1016/j.apradiso.2011.02.013. PMID 21393005.
- Kawabata, S.; Miyatake, S.; Hiramatsu, R.; Hirota, Y.; Miyata, S.; Takekita, Y.; Kuroiwa, T.; Kirihata, M.; Sakurai, Y.; Maruhashi, A.; Ono, K. (2011). "Phase II clinical study of boron neutron capture therapy combined with X-ray radiotherapy/temozolomide in patients with newly diagnosed glioblastoma multiforme--study design and current status report". Appl. Radiat. Isot. 69 (12): 1796–1799. doi:10.1016/j.apradiso.2011.03.014. PMID 21459588.
- Kulvik, M.; Hermans, R.; Linnosmaa, I.; Shalowitz, J. (2015). "An economic model to assess the cost-benefit of BNCT". Appl Radiat Isotopes. 106: 3–9. doi:10.1016/j.apradiso.2015.08.021. PMID 26365901.
- "HUS - BNCT-sädehoitolaite HUS:iin ensimmäisenä maailmassa". www.hus.fi (in Finnish and English). Retrieved 27 July 2017.
- Kivimäki, Antti (15 September 2016). "Helsingissä testataan mullistavaa syöpähoitoa – nyt ilman ydinreaktoria". Helsingin Sanomat (in Finnish). Retrieved 27 July 2017.
- "Faculty of Medicine – University of Helsinki". www.med.helsinki.fi. 10 June 2016. Retrieved 27 July 2017.
- Henriksson, R.; Capala, J.; Michanek, A.; Lindahl, S.-Å.; Salford, L.G.; Franzén, L.; Blomquist, E.; Westlin, J.-E.; et al. (2008). "Boron neutron capture therapy (BNCT) for glioblastoma multiforme: A phase II study evaluating a prolonged high-dose of boronophenylalanine (BPA)". Radiotherapy and Oncology. 88 (2): 183–91. doi:10.1016/j.radonc.2006.04.015. PMID 18336940.
- Sköld, K.; Gorlia, T.; Pellettieri, L.; Giusti, V.; H-Stenstam, B.; Hopewell, J.W. (2010). "Boron neutron capture therapy for newly diagnosed glioblastoma multiforme: An assessment of clinical potential". British Journal of Radiology. 83 (991): 596–603. doi:10.1259/bjr/56953620. PMC 3473677. PMID 20603410.
- Wittig A, Hideghety K, Paquis P, et al. (2002). Sauerwein W, Mass R, Wittig A (eds.). Current clinical results of the EORTC – study 11961. Research and Development in Neutron Capture Therapy Proc. 10th Intl. Congress on Neutron Capture Therapy. pp. 1117–22.
- Smith, D.R.; Chandra, S.; Barth, R.F.; Yang, W.; Joel, D.D.; Coderre, J. (15 November 2001). "Quantitative imaging and microlocalization of boron-10 in brain tumors and infiltrating tumor cells by SIMS ion microscopy: Relevance to neutron capture therapy" (PDF). Cancer Research. 61: 8179–8187.
- Stupp, R.; Hegi, M.E.; Mason, W.P.; Van Den Bent, M.J.; Taphoorn, M.J.B.; Janzer, R.C.; Ludwin, S.K.; Allgeier, A.; et al. (2009). "Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial". The Lancet Oncology. 10 (5): 459–66. doi:10.1016/S1470-2045(09)70025-7. PMID 19269895.
- Kato, I.; Fujita, Y.; Maruhashi, A.; Kumada, H.; Ohmae, M.; Kirihata, M.; Imahori, Y.; Suzuki, M.; et al. (2009). "Effectiveness of boron neutron capture therapy for recurrent head and neck malignancies". Applied Radiation and Isotopes. 67 (7–8): S37–42. doi:10.1016/j.apradiso.2009.03.103. PMID 19409799.
- Kato, I.; Ono, K.; Sakurai, Y.; Ohmae, M.; Maruhashi, A.; Imahori, Y.; Kirihata, M.; Nakazawa, M.; Yura, Y. (2004). "Effectiveness of BNCT for recurrent head and neck malignancies". Appl. Radiat. Isot. 61 (5): 1069–73. doi:10.1016/j.apradiso.2004.05.059. PMID 15308194.
- Wang, Ling-Wei; Liu, Yen-Wan Hsueh; Chou, Fong-In; Jiang, Shiang-Huei (2018). "Clinical trials for treating recurrent head and neck cancer with boron neutron capture therapy using the Tsing-Hua Open Pool Reactor". Cancer Communications. 38 (37): 37. doi:10.1186/s40880-018-0295-y. PMC 6006853. PMID 29914577.
- Mishima, Y. (1996). "Selective thermal neutron capture therapy of cancer cells using their specific metabolic activities—melanoma as prototype". In Mishima, Y. (ed.). Cancer neutron capture therapy. pp. 1–26. doi:10.1007/978-1-4757-9567-7_1. ISBN 978-1-4757-9569-1.
- Coderre, Jeffrey A.; Joel, Darrel D.; Micca, Peggy L.; Nawrocky, Marta M.; Slatkin, Daniel N. (1 January 1992). "Control of Intracerebral Gliosarcomas in Rats by Boron Neutron Capture Therapy with p-Boronophenylalanine". Radiation Research. 129 (3): 290–296. Bibcode:1992RadR..129..290C. doi:10.2307/3578028. JSTOR 3578028.
- Hiratsuka, J.; Kamitani, N.; Tanaka, R.; Yoden, E.; Tokiya, R.; Suzuki, M.; Barth, R.F.; Ono, K.; et al. (2018). "Boron neutron capture therapy for vulvar melanoma and genital extramammary Paget's disease, with curative responses". Cancer Communications. 38 (1): 38. doi:10.1186/s40880-018-0297-9. PMC 6006671. PMID 29914570.
- "The BNCT Project at the National Atomic Energy Commission (CNEA)". Comision Nacional de Energia Atomica. Archived from the original on 23 March 2012.CS1 maint: unfit url (link)
- Zonta, A.; Pinelli, T.; Prati, U.; Roveda, L.; Ferrari, C.; Clerici, A.M.; Zonta, C.; Mazzini, G.; et al. (2009). "Extra-corporeal liver BNCT for the treatment of diffuse metastases: What was learned and what is still to be learned". Applied Radiation and Isotopes. 67 (7–8): S67–75. doi:10.1016/j.apradiso.2009.03.087. PMID 19394837.
- Zonta, A.; Prati, U.; Roveda, L.; Ferrari, C.; Zonta, S.; Clerici, A.M.; Zonta, C.; Pinelli, T.; et al. (2006). "Clinical lessons from the first applications of BNCT on unresectable liver metastases". Journal of Physics: Conference Series. 41 (1): 484–95. Bibcode:2006JPhCS..41..484Z. doi:10.1088/1742-6596/41/1/054.
- Yanagie, H., Oyama, K., Hatae, R. et al. Clinical experiences of boron neutron capture therapy to recurrenced rectal cancers. Abstracts 16th Intl' Congress on Neutron Capture Therapy. Helsinki, Finland, June 14–19, 2014
- Barth, R.F.; Zhang, Z.; Liu, T. (2018). "A realistic appraisal of boron neutron capture therapy as a cancer treatment modality". Cancer Communications. 38 (1): 36. doi:10.1186/s40880-018-0280-5. PMC 6006699. PMID 29914575.
- Yu, T.L. (2018). "Prof. Rolf F. Barth: the future of boron neutron capture therapy will depend on the clinical trials of accelerator-based boron neutron capture therapy". Ther. Radiol. Oncol. 2 (58): 58. doi:10.21037/tro.2018.11.03.