Urinary incontinence
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life.[1] It has been identified as an important issue in geriatric health care.[2] The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis (bed wetting).[3]
| Urinary incontinence | |
|---|---|
| Other names | Involuntary urination |
| Specialty | Urology, gynecology |
Pelvic surgery, pregnancy, childbirth, and menopause are major risk factors.[4] Urinary incontinence is often a result of an underlying medical condition but is under-reported to medical practitioners.[5] There are four main types of incontinence:[6]
- Urge incontinence due to an overactive bladder
- Stress incontinence due to poor closure of the bladder
- Overflow incontinence due to either poor bladder contraction or blockage of the urethra
- Functional incontinence due to medications or health problems making it difficult to reach the bathroom
Treatments include pelvic floor muscle training, bladder training, surgery, and electrical stimulation.[7] Behavioral therapy generally works better than medication for stress and urge incontinence.[8] The benefit of medications is small and long term safety is unclear.[7] Urinary incontinence is more common in older women.[9]
Causes
Urinary incontinence can result from both urologic and non-urologic causes. Urologic causes can be classified as either bladder or urethral dysfunction and may include detrusor overactivity, poor bladder compliance, urethral hypermobility, or intrinsic sphincter deficiency. Non-urologic causes may include infection, medication or drugs, psychological factors, polyuria, stool impaction, and restricted mobility.[10]
The most common types of urinary incontinence in women are stress urinary incontinence and urge urinary incontinence. Women with both problems have mixed urinary incontinence. After menopause, estrogen production decreases and in some women urethral tissue will demonstrate atrophy with the tissue of the urethra becoming weaker and thinner.[4] Stress urinary incontinence is caused by loss of support of the urethra which is usually a consequence of damage to pelvic support structures as a result of childbirth. It is characterized by leaking of small amounts of urine with activities which increase abdominal pressure such as coughing, sneezing and lifting. Additionally, frequent exercise in high-impact activities can cause athletic incontinence to develop. Urge urinary incontinence is caused by uninhibited contractions of the detrusor muscle . It is characterized by leaking of large amounts of urine in association with insufficient warning to get to the bathroom in time.
- Polyuria (excessive urine production) of which, in turn, the most frequent causes are: uncontrolled diabetes mellitus, primary polydipsia (excessive fluid drinking), central diabetes insipidus and nephrogenic diabetes insipidus.[11] Polyuria generally causes urinary urgency and frequency, but doesn't necessarily lead to incontinence.
- Enlarged prostate is the most common cause of incontinence in men after the age of 40; sometimes prostate cancer may also be associated with urinary incontinence. Moreover, drugs or radiation used to treat prostate cancer can also cause incontinence.
- Disorders like multiple sclerosis, spina bifida, Parkinson's disease, strokes and spinal cord injury can all interfere with nerve function of the bladder.
- Urinary incontinence is a likely outcome following a radical prostatectomy procedure.[12]
- About 33% of all women experience UI after giving birth; women who deliver vaginally are about twice as likely to have urinary incontinence as women who give birth via a Caesarean section.[13]
Mechanism
Continence and micturition involve a balance between urethral closure and detrusor muscle activity. Urethral pressure normally exceeds bladder pressure, resulting in urine remaining in the bladder. The proximal urethra and bladder are both within the pelvis. Intra abdominal pressure increases (from coughing and sneezing) are transmitted to both urethra and bladder equally, leaving the pressure differential unchanged, resulting in continence. Normal voiding is the result of changes in both of these pressure factors: urethral pressure falls and bladder pressure rises.
The body stores urine — water and wastes removed by the kidneys — in the urinary bladder, a balloon-like organ. The bladder connects to the urethra, the tube through which urine leaves the body.
During urination, detrusor muscles in the wall of the bladder contract, forcing urine out of the bladder and into the urethra. At the same time, sphincter muscles surrounding the urethra relax, letting urine pass out of the body. Incontinence will occur if the bladder muscles suddenly contract (detrusor muscle) or muscles surrounding the urethra suddenly relax (sphincter muscles).
Children
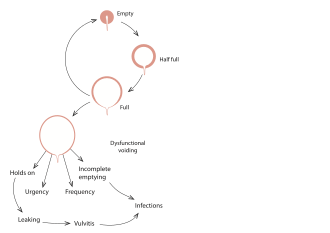
Urination, or voiding, is a complex activity. The bladder is a balloonlike muscle that lies in the lowest part of the abdomen. The bladder stores urine, then releases it through the urethra, the canal that carries urine to the outside of the body. Controlling this activity involves nerves, muscles, the spinal cord and the brain.
The bladder is made of two types of muscles: the detrusor, a muscular sac that stores urine and squeezes to empty, and the sphincter, a circular group of muscles at the bottom or neck of the bladder that automatically stay contracted to hold the urine in and automatically relax when the detrusor contracts to let the urine into the urethra. A third group of muscles below the bladder (pelvic floor muscles) can contract to keep urine back.
A baby's bladder fills to a set point, then automatically contracts and empties. As the child gets older, the nervous system develops. The child's brain begins to get messages from the filling bladder and begins to send messages to the bladder to keep it from automatically emptying until the child decides it is the time and place to void.
Failures in this control mechanism result in incontinence. Reasons for this failure range from the simple to the complex.
Diagnosis
A careful history taking is essential especially in the pattern of voiding and urine leakage as it suggests the type of incontinence faced. Other important points include straining and discomfort, use of drugs, recent surgery, and illness.
The physical examination will focus on looking for signs of medical conditions causing incontinence, such as tumors that block the urinary tract, stool impaction, and poor reflexes or sensations, which may be evidence of a nerve-related cause.
A test often performed is the measurement of bladder capacity and residual urine for evidence of poorly functioning bladder muscles.
Other tests include:
- Stress test – the patient relaxes, then coughs vigorously as the doctor watches for loss of urine.
- Urinalysis – urine is tested for evidence of infection, urinary stones, or other contributing causes.
- Blood tests – blood is taken, sent to a laboratory, and examined for substances related to causes of incontinence.
- Ultrasound – sound waves are used to visualize the kidneys and urinary bladder.
- Cystoscopy – a thin tube with a tiny camera is inserted in the urethra and used to see the inside of the urethra and bladder.
- Urodynamics – various techniques measure pressure in the bladder and the flow of urine.
Patients are often asked to keep a diary for a day or more, up to a week, to record the pattern of voiding, noting times and the amounts of urine produced.
Research projects that assess the efficacy of anti-incontinence therapies often quantify the extent of urinary incontinence. The methods include the 1-h pad test, measuring leakage volume; using a voiding diary, counting the number of incontinence episodes (leakage episodes) per day; and assessing of the strength of pelvic floor muscles, measuring the maximum vaginal squeeze pressure.
Types
- Stress incontinence, also known as effort incontinence, is due essentially to insufficient strength of the pelvic floor muscles to prevent the passage of urine, especially during activities that increase intra-abdominal pressure, such as coughing, sneezing, or bearing down.
- Urge incontinence is involuntary loss of urine occurring for no apparent reason while suddenly feeling the need or urge to urinate.
- Overflow incontinence: Sometimes people find that they cannot stop their bladders from constantly dribbling or continuing to dribble for some time after they have passed urine. It is as if their bladders were constantly overflowing, hence the general name overflow incontinence.
- Mixed incontinence is not uncommon in the elderly female population and can sometimes be complicated by urinary retention.
- Structural incontinence: Rarely, structural problems can cause incontinence, usually diagnosed in childhood (for example, an ectopic ureter). Fistulas caused by obstetric and gynecologic trauma or injury are commonly known as obstetric fistulas and can lead to incontinence. These types of vaginal fistulas include, most commonly, vesicovaginal fistula and, more rarely, ureterovaginal fistula. These may be difficult to diagnose. The use of standard techniques along with a vaginogram or radiologically viewing the vaginal vault with instillation of contrast media.[14]
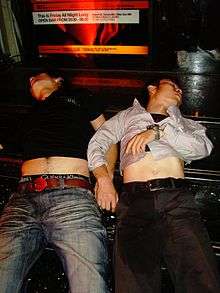
- Functional incontinence occurs when a person recognizes the need to urinate but cannot make it to the bathroom. The loss of urine may be large. There are several causes of functional incontinence including confusion, dementia, poor eyesight, mobility or dexterity, unwillingness to toilet because of depression or anxiety or inebriation due to alcohol.[15] Functional incontinence can also occur in certain circumstances where no biological or medical problem is present. For example, a person may recognise the need to urinate but may be in a situation where there is no toilet nearby or access to a toilet is restricted.
- Nocturnal enuresis is episodic UI while asleep. It is normal in young children.
- Transient incontinence is a temporary incontinence most often seen in pregnant women when it subsequently resolves after the birth of the child.[16]
- Giggle incontinence is an involuntary response to laughter. It usually affects children.
- Double incontinence. There is also a related condition for defecation known as fecal incontinence. Due to involvement of the same muscle group (levator ani) in bladder and bowel continence, patients with urinary incontinence are more likely to have fecal incontinence in addition.[17] This is sometimes termed "double incontinence".
- Post-void dribbling is the phenomenon where urine remaining in the urethra after voiding the bladder slowly leaks out after urination.
- Coital incontinence (CI) is urinary leakage that occurs during either penetration or orgasm and can occur with a sexual partner or with masturbation. It has been reported to occur in 10% to 24% of sexually active women with pelvic floor disorders.[18]
- Climacturia is urinary incontinence at the moment of orgasm. It can be a result of radical prostatectomy.
Screening
Yearly screening is recommended for women by the Women's Preventive Services Initiative. Screening questions should inquire about what symptoms they have experienced, how severe the symptoms are, and if the symptoms affect their daily lives.[19] As of 2018, studies have not shown a change in outcomes with urinary incontinence screenings in women.[20]
Management
Treatment options range from conservative treatment, behavior management, bladder retraining,[21] pelvic floor therapy, collecting devices (for men), fixer-occluder devices for incontinence (in men), medications and surgery.[22] The success of treatment depends on the correct diagnoses.[23] Weight loss is recommended in those who are obese.[24]
Behavioral therapy
Behavioral therapy involves the use of both suppressive techniques (distraction, relaxation) and learning to avoid foods that may worsen urinary incontinence. This may involve avoiding or limiting consumption of caffeine and alcohol. Behavioral therapy is not curative for urinary incontinence, but it can improve a person's quality of life. Behavioral therapy has benefits as both a monotherapy and as an adjunct to medications for symptom reduction.[25]
Lifestyle changes
Avoiding heavy lifting and preventing constipation may help with uncontrollable urine leakage. Stopping smoking is also recommended as it is associated with improvements in urinary incontinence in men and women.[26]
Exercises
Exercising the muscles of the pelvis such as with Kegel exercises are a first line treatment for women with stress incontinence.[24] Efforts to increase the time between urination, known as bladder training, is recommended in those with urge incontinence.[24] Both these may be used in those with mixed incontinence.[24]
Small vaginal cones of increasing weight may be used to help with exercise.[27][28] They seem to be better than no active treatment in women with stress urinary incontinence, and have similar effects to training of pelvic floor muscles or electrostimulation.[28]
Biofeedback uses measuring devices to help the patient become aware of his or her body's functioning. By using electronic devices or diaries to track when the bladder and urethral muscles contract, the patient can gain control over these muscles. Biofeedback can be used with pelvic muscle exercises and electrical stimulation to relieve stress and urge incontinence.
Time voiding while urinating and bladder training are techniques that use biofeedback. In time voiding, the patient fills in a chart of voiding and leaking. From the patterns that appear in the chart, the patient can plan to empty his or her bladder before he or she would otherwise leak. Biofeedback and muscle conditioning, known as bladder training, can alter the bladder's schedule for storing and emptying urine. These techniques are effective for urge and overflow incontinence[29]
A 2013 randomized controlled trial found no benefit of adding biofeedback to pelvic floor muscle exercise in stress urinary incontinence, but observing improvements in both groups.[30] In another randomized controlled trial the addition of biofeedback to the training of pelvic floor muscles for the treatment of stress urinary incontinence, improved pelvic floor muscle function, reduced urinary symptoms, and improved of the quality of life.[31]
Preoperative pelvic floor muscle training (PFMT) in men undergoing radical prostatectomy was not effective in reducing urinary incontinence.[12]
Alternative exercises have been studied for stress urinary incontinence in women.[32] Evidence was insufficient to support the use of Paula method, abdominal muscle training, Pilates, Tai Chi, breathing exercises, postural training, and generalized fitness.[32]
Devices
Individuals who continue to experience urinary incontinence need to find a management solution that matches their individual situation. The use of mechanical devices has not been well studied in women, as of 2014.[33]
- Collecting systems (for men) – consists of a sheath worn over the penis funneling the urine into a urine bag worn on the leg. These products come in a variety of materials and sizes for individual fit. Studies [34] show that urisheaths and urine bags are preferred over absorbent products – in particular when it comes to ‘limitations to daily activities’. Solutions exist for all levels of incontinence. Advantages with collecting systems are that they are discreet, the skin stays dry all the time, and they are convenient to use both day and night. Disadvantages are that it is necessary to get measured to ensure proper fit, and in some countries a prescription is needed.
- Absorbent products (include shields, undergarments, protective underwear, briefs, diapers, adult diapers and underpants) are the best-known product types to manage incontinence. They are widely available in pharmacies and supermarkets. The advantages of using these are that they barely need any fitting or introduction by a health-care specialist. The disadvantages with absorbent products are that they can be bulky, leak, have odors and can cause skin breakdown due to the constant dampness.
- Fixer-occluder devices (for men) are strapped around the penis, softly pressing the urethra and stopping the flow of urine. This management solution is only suitable for light or moderate incontinence.
- Intermittent catheters are single-use catheters that are inserted into the bladder to empty it, and once the bladder is empty they are removed and discarded. Intermittent catheters are primarily used for urinary retention (inability to empty the bladder), but for some people they can be used to reduce or avoid incontinence. These are prescription-only medical devices.
- Indwelling catheters (also known as foleys) are often used in hospital settings, or if the user is not able to handle any of the above solutions himself/herself (e.g. severe neurologic injury or neurodegenerative disease). These are also prescription-only medical devices. The indwelling catheter is typically connected to a urine bag that can be worn on the leg or hung on the side of the bed. Indwelling catheters need to be monitored and changed on a regular basis by a health-care professional. The advantage of indwelling catheters is that because the urine is funneled away from the body, the skin remains dry. However, the disadvantage is that it is very common to incur urinary-tract infections when using indwelling catheters. Bladder spasms and other problems can also occur with long-term use of indwelling catheters.[35]
Medications
A number of medications exist to treat urinary incontinence including: fesoterodine, tolterodine and oxybutynin.[36] These medications work by relaxing smooth muscle in the bladder.[37][38][39] While some of these medications appear to have a small benefit, the risk of side effects are a concern.[36] Medications are effective for about one in ten people, and all medications have similar efficacy.[36]
Medications are not recommended for those with stress incontinence and are only recommended in those with urge incontinence who do not improve with bladder training.[24]
Surgery
Surgery may be used to help stress or overflow incontinence.[6] Common surgical techniques for stress incontinence include slings, tension-free vaginal tape, and bladder suspension among others.[6] However, the use of transvaginal mesh implants and bladder slings is controversial. Due to the risk of debilitating painful side effects such as vaginal erosion,[40] and in 2012 transvaginal mesh implants were classified as a high risk device by the US Food and Drug Administration.[41] Urodynamic testing seems to confirm that surgical restoration of vault prolapse can cure motor urge incontinence. In those with problems following prostate surgery there is little evidence regarding the use of surgery.[42]
Traditional suburethal sling operations probably reduce urinary incontinence in women compared to open abdominal retropubic suspension but appear to be no better or worse than minimally invasive sling operations or injectable treatments. There is probably little or no difference in effectiveness between the different types of traditional suburethal sling operations and there is insufficient evidence to be certain about the effectiveness of traditional slings compared to bladder neck needle suspension.[43] Similarly, there is insufficient evidence to be certain about the effectiveness or safety of single-incision sling operations for urinary incontinence in women.[44] Suburethal slings may have a higher risk of complications than bladder neck needle suspension or minimally invasive slings.[43]
Laparoscopic colposuspension (keyhole surgery through the abdomen) with sutures is as effective as open colposuspension for curing incontinence in women up to 18 months after surgery, but it is unclear whether there are fewer risk of complications during or after surgery.[45] There is probably a higher risk of complications with traditional suburethal slings than with open abdominal retropubic suspension.[45]
Epidemiology
Globally, up to 35% of the population over the age of 60 years is estimated to be incontinent.[48] In 2014, urinary leakage affected between 30% and 40% of people over 65 years of age living in their own homes or apartments in the U.S.[49] Twenty-four percent of older adults in the U.S. have moderate or severe urinary incontinence that should be treated medically.[49]
Bladder control problems have been found to be associated with higher incidence of many other health problems such as obesity and diabetes. Difficulty with bladder control results in higher rates of depression and limited activity levels.[50]
Incontinence is expensive both to individuals in the form of bladder control products and to the health care system and nursing home industry. Injury related to incontinence is a leading cause of admission to assisted living and nursing care facilities. More than 50% of nursing facility admissions are related to incontinence.[51]
Children
Incontinence happens less often after age 5: About 10 percent of 5-year-olds, 5 percent of 10-year-olds, and 1 percent of 18-year-olds experience episodes of incontinence. It is twice as common in girls as in boys.[52]
Women
Bladder symptoms affect women of all ages. However, bladder problems are most prevalent among older women.[53] Women over the age of 60 years are twice as likely as men to experience incontinence; one in three women over the age of 60 years are estimated to have bladder control problems.[48] One reason why women are more affected is the weakening of pelvic floor muscles by pregnancy.[54]
Men
Men tend to experience incontinence less often than women, and the structure of the male urinary tract accounts for this difference. It is common with prostate cancer treatments. Both women and men can become incontinent from neurologic injury, congenital defects, strokes, multiple sclerosis, and physical problems associated with aging.
While urinary incontinence affects older men more often than younger men, the onset of incontinence can happen at any age. Estimates in the mid-2000s suggested that 17 percent of men over age 60, an estimated 600,000 men, experienced urinary incontinence, with this percentage increasing with age.[55]
History
The management of urinary incontinence with pads is mentioned in the earliest medical book known, the Ebers Papyrus (1500 BC).[56]
Incontinence has historically been a taboo subject in Western culture. However, this situation changed some when Kimberly-Clark aggressively marketed adult diapers in the 1980s with actor June Allyson as spokeswoman. Allyson was initially reticent to participate, but her mother, who had incontinence, convinced her that it was her duty in light of her successful career. The product proved a success.[57]
References
- Ackley B (2010). Nursing diagnosis handbook : an evidence-based guide to planning care (9th ed.). Maryland Heights, Mo: Mosby. ISBN 9780323071505.
- Venes D (2013). Taber's cyclopedic medical dictionary. Philadelphia: F.A. Davis. ISBN 9780803629776.
- "Enuresis". medicaldictionaryweb.com.
- "Urinary incontinence fact sheet". Womenshealth.gov. July 16, 2012. Retrieved 2016-12-05.
- "Medicinewise News". NPS MedicineWise. Archived from the original on 2012-06-30. Retrieved 2013-09-24.
- Ghosh AK (2008). Mayo Clinic internal medicine concise textbook. Rochester, MN: Mayo Clinic Scientific Press. p. 339. ISBN 9781420067514.
- Shamliyan T, Wyman J, Kane RL (April 2012). "Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness". AHRQ Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality (US). PMID 22624162. Cite journal requires
|journal=(help) - Balk EM, Rofeberg VN, Adam GP, Kimmel HJ, Trikalinos TA, Jeppson PC (March 2019). "Pharmacologic and Nonpharmacologic Treatments for Urinary Incontinence in Women: A Systematic Review and Network Meta-analysis of Clinical Outcomes". Annals of Internal Medicine. 170 (7): 465–479. doi:10.7326/M18-3227. PMID 30884526.
- "Urinary Incontinence in Older Adults". National Institute on Aging. Retrieved 18 March 2018.
- "American Urological Association - Medical Student Curriculum: Urinary Incontinence". www.auanet.org. Retrieved 11 January 2018.
- merck.com > Polyuria: A Merck Manual of Patient Symptoms podcast. Last full review/revision September 2009 by Seyed-Ali Sadjadi, MD
- Wang W, Huang QM, Liu FP, Mao QQ (December 2014). "Effectiveness of preoperative pelvic floor muscle training for urinary incontinence after radical prostatectomy: a meta-analysis". BMC Urology. 14 (1): 99. doi:10.1186/1471-2490-14-99. PMC 4274700. PMID 25515968.
- Thom DH, Rortveit G (December 2010). "Prevalence of postpartum urinary incontinence: a systematic review". Acta Obstetricia et Gynecologica Scandinavica. 89 (12): 1511–22. doi:10.3109/00016349.2010.526188. PMID 21050146.
- Macaluso JN, Appell RA, Sullivan JW (September 1981). "Ureterovaginal fistula detected by vaginogram". JAMA. 246 (12): 1339–40. doi:10.1001/jama.246.12.1339. PMID 7265431.
- "Functional incontinence". Australian Government Department of Health and Ageing. 2008. Archived from the original on 2008-07-23. Retrieved 2008-08-29.
- Sangsawang B, Sangsawang N (June 2013). "Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment". International Urogynecology Journal. 24 (6): 901–12. doi:10.1007/s00192-013-2061-7. PMC 3671107. PMID 23436035.
- Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ (December 2007). "Prevention of urinary and fecal incontinence in adults". Evidence Report/Technology Assessment (161): 1–379. PMC 4781595. PMID 18457475.
- Karlovsky, Matthew E. MD, Female Urinary Incontinence During Sexual Intercourse (Coital Incontinence): A Review, The Female Patient (retrieved 22 August 2010)
- O'Reilly N, Nelson HD, Conry JM, Frost J, Gregory KD, Kendig SM, et al. (September 2018). "Screening for Urinary Incontinence in Women: A Recommendation From the Women's Preventive Services Initiative". Annals of Internal Medicine. 169 (5): 320–328. doi:10.7326/M18-0595. PMID 30105360.
- Nelson, Heidi D.; Cantor, Amy; Pappas, Miranda; Miller, Liev (2018-09-04). "Screening for Urinary Incontinence in Women: A Systematic Review for the Women's Preventive Services Initiative". Annals of Internal Medicine. 169 (5): 311–319. doi:10.7326/M18-0225. ISSN 0003-4819. PMID 30105353.
- Bladder retraining ichelp.org Interstitial Cystitis Association Accessed July 13, 2012
- Price N, Jackson SR (2004). "Clinical audit of the use of tension-free vaginal tape as a surgical treatment for urinary stress incontinence, set against NICE guidelines". J Obstet Gynaecol. 24 (5): 534–538. doi:10.1080/01443610410001722590. PMID 15369935.
- What is Male Urinary Incontinence? Retrieved on 2010-03-02
- Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Shekelle P (September 2014). "Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 161 (6): 429–40. doi:10.7326/m13-2410. PMID 25222388.
- Elavsky M (February 2018). "Urinary Incontinence: What Pharmacists Should Know". DrugTopics. 162 (2): 24.
- Wyman JF, Burgio KL, Newman DK (August 2009). "Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence". International Journal of Clinical Practice. 63 (8): 1177–91. doi:10.1111/j.1742-1241.2009.02078.x. PMC 2734927. PMID 19575724.
- Chelsea (September 4, 2012). "How to Use Vaginal Weights". National Incontinence. Retrieved 10 October 2012.
- Herbison GP, Dean N (July 2013). "Weighted vaginal cones for urinary incontinence". The Cochrane Database of Systematic Reviews (7): CD002114. doi:10.1002/14651858.CD002114.pub2. PMID 23836411.
- Health, Beaumont. "Treatment for Incontinence". www.beaumont.org. Retrieved 19 October 2018.
- Hirakawa T, Suzuki S, Kato K, Gotoh M, Yoshikawa Y (August 2013). "Randomized controlled trial of pelvic floor muscle training with or without biofeedback for urinary incontinence". International Urogynecology Journal. 24 (8): 1347–54. doi:10.1007/s00192-012-2012-8. PMID 23306768.
- Fitz FF, Resende AP, Stüpp L, Costa TF, Sartori MG, Girão MJ, Castro RA (November 2012). "[Effect the adding of biofeedback to the training of the pelvic floor muscles to treatment of stress urinary incontinence]". Revista Brasileira de Ginecologia e Obstetricia. 34 (11): 505–10. doi:10.1590/S0100-72032012001100005. PMID 23288261.
- Bø K, Herbert RD (September 2013). "There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review". Journal of Physiotherapy. 59 (3): 159–68. doi:10.1016/S1836-9553(13)70180-2. PMID 23896331.
There is not yet strong evidence that alternative exercise regimens can reduce urinary leakage in women with stress urinary incontinence.
- Lipp A, Shaw C, Glavind K (December 2014). "Mechanical devices for urinary incontinence in women". The Cochrane Database of Systematic Reviews. 12 (12): CD001756. doi:10.1002/14651858.CD001756.pub6. PMID 25517397.
- Chartier-Kastler E, Ballanger P, Petit J, Fourmarier M, Bart S, Ragni-Ghazarossian E, Ruffion A, Le Normand L, Costa P (July 2011). "Randomized, crossover study evaluating patient preference and the impact on quality of life of urisheaths vs absorbent products in incontinent men". BJU International. 108 (2): 241–7. doi:10.1111/j.1464-410X.2010.09736.x. PMID 20950307.
- Cravens DD, Zweig S (January 2000). "Urinary catheter management". American Family Physician. 61 (2): 369–76. PMID 10670503.
- Shamliyan T, Wyman JF, Ramakrishnan R, Sainfort F, Kane RL (June 2012). "Benefits and harms of pharmacologic treatment for urinary incontinence in women: a systematic review". Annals of Internal Medicine. 156 (12): 861–74, W301–10. doi:10.7326/0003-4819-156-12-201206190-00436. PMID 22711079.
- "Oxybutynin Chloride Monograph for Professionals". Drugs.com. Retrieved 2019-08-05.
- "Tolterodine Tartrate Tablets - FDA prescribing information, side effects and uses". Drugs.com. Retrieved 2019-08-05.
- "Fesoterodine Tablets - FDA prescribing information, side effects and uses". Drugs.com. Retrieved 2019-08-05.
- "Vaginal Mesh & Bladder Sling Complications and Lawsuits". Lieff Cabraser Heimann & Bernstein, LLP. Retrieved 2018-05-10.
- Davey M (2017-08-31). "What does pelvic mesh do and why are women suing over it? – explainer". the Guardian. Retrieved 2018-05-10.
- Silva LA, Andriolo RB, Atallah ÁN, da Silva EM (September 2014). "Surgery for stress urinary incontinence due to presumed sphincter deficiency after prostate surgery". The Cochrane Database of Systematic Reviews. 9 (9): CD008306. doi:10.1002/14651858.CD008306.pub3. PMID 25261861.
- Rehman, H; Bezerra, CA; Bruschini, H; Cody, JD; Aluko, P (26 July 2017). "Traditional suburethral sling operations for urinary incontinence in women". The Cochrane Database of Systematic Reviews. 7: CD001754. doi:10.1002/14651858.CD001754.pub4. PMC 6483312. PMID 28743177.
- Nambiar, A; Cody, JD; Jeffery, ST; Aluko, P (26 July 2017). "Single-incision sling operations for urinary incontinence in women". The Cochrane Database of Systematic Reviews. 7: CD008709. doi:10.1002/14651858.CD008709.pub3. PMC 6483163. PMID 28746980.
- Freites, Jawad; Stewart, Fiona; Omar, Muhammad Imran; Mashayekhi, Atefeh; Agur, Wael I (2019-12-10). Cochrane Incontinence Group (ed.). "Laparoscopic colposuspension for urinary incontinence in women". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD002239.pub4.
- Kirchin, Vivienne; Page, Tobias; Keegan, Phil E; Atiemo, Kofi OM; Cody, June D; McClinton, Samuel; Aluko, Patricia (2017-07-25). "Urethral injection therapy for urinary incontinence in women". Cochrane Database of Systematic Reviews. 7: CD003881. doi:10.1002/14651858.cd003881.pub4. ISSN 1465-1858. PMC 6483304. PMID 28738443.
- Matsuoka PK, Locali RF, Pacetta AM, Baracat EC, Haddad JM (February 2016). "The efficacy and safety of urethral injection therapy for urinary incontinence in women: a systematic review". Clinics. 71 (2): 94–100. doi:10.6061/clinics/2016(02)08. PMC 4760362. PMID 26934239.
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S (November 2000). "A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag". Journal of Clinical Epidemiology. 53 (11): 1150–7. doi:10.1016/S0895-4356(00)00232-8. PMID 11106889.
- U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (June 2014). "Prevalence of Incontinence Among Older Americans" (PDF). CDC. Retrieved 23 August 2014.
- Nygaard I, Turvey C, Burns TL, Crischilles E, Wallace R (January 2003). "Urinary incontinence and depression in middle-aged United States women". Obstetrics and Gynecology. 101 (1): 149–56. doi:10.1016/s0029-7844(02)02519-x. PMID 12517660.
- Thom DH, Haan MN, Van Den Eeden SK (September 1997). "Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality". Age and Ageing. 26 (5): 367–74. doi:10.1093/ageing/26.5.367. PMID 9351481.
- Pediatric incontinence - Franco - 2015 - Wiley Online Books - Wiley Online Library. 2015. doi:10.1002/9781118814789. ISBN 9781118814789.
- Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ (June 2001). "How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study". BJU International. 87 (9): 760–6. doi:10.1046/j.1464-410x.2001.02228.x. PMID 11412210.
- Graham J (July 29, 2014). "An 'Emotional Burden' Rarely Discussed". New York Times. Retrieved August 23, 2014.
- Stothers L, Thom D, Calhoun E (2007). "Chapter 6: Urinary Incontinence in Men". Urologic Diseases in America Report. National Institutes of Health.
- Becker H, Stenzl A, Wallwiener D, Zittel TT (2005). Urinary and fecal incontinence : an interdisciplinary approach; with 89 tables. Berlin [u.a.]: Springer. p. 232. ISBN 978-3540222255.
- O'Reilly T (8 June 2017). "Now Splinter Free: How Marketing Broke Taboos". CBC Radio One. Pirate Radio. Retrieved 10 June 2017.
External links
| Classification | |
|---|---|
| External resources |
- Urinary incontinence at Curlie
- Patient-centered information from the European Urological Association