Betahistine
Betahistine, sold under the brand name Serc among others, is an anti-vertigo medication. It is commonly prescribed for balance disorders or to alleviate vertigo symptoms, e.g. those associated with Ménière's disease. It was first registered in Europe in 1970 for the treatment of Ménière's disease.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Serc, others |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | By mouth Pregnancy category= c(risk not ruled out) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ~100%[1] |
| Protein binding | <5%[1] |
| Metabolism | Liver[1] |
| Metabolites | • 2-(2-Aminoethyl)pyridine • 2-Pyridylacetic acid[1] |
| Onset of action | <1 hour (peak)[2] |
| Elimination half-life | 3.5 hours[3] |
| Excretion | Urine: 91%[1] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.024.625 |
| Chemical and physical data | |
| Formula | C8H12N2 |
| Molar mass | 136.194 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Medical uses
Betahistine is used in the treatment of Ménière's disease and vertigo.[3] The supporting evidence for the efficacy of betahistine for Ménière's disease is of poor quality.[3] A 2011 Cochrane review of seven trials consisting of 243 patients with Ménière's disease concluded that there was insufficient evidence for any beneficial effect of betahistine on symptoms.[3] Most of the trials found a reduction in symptoms of vertigo and to a lesser extent tinnitus, but these effects may have been due to bias in study methodology.[3]
Contraindications
Betahistine is contraindicated for patients with pheochromocytoma. Patients with bronchial asthma or a history of peptic ulcer need to be closely monitored.
Side effects
Patients taking betahistine may experience following side effects:[4]
- Headache
- Low level of gastric side effects
- Nausea can be a side effect, but the patient is generally already experiencing nausea due to the vertigo so it goes largely unnoticed.
- Patients taking betahistine may experience several hypersensitivity and allergic reactions. In the November 2006 issue of "Drug Safety," Dr. Sabine Jeck-Thole and Dr. Wolfgang Wagner reported that betahistine may cause several allergic and skin-related side effects. These include rash in several areas of the body; itching and hives; and swelling of the face, tongue and mouth. Other hypersensitivity reactions reported include tingling, numbness, burning sensations, shortness of breath and laboured breathing. The study authors suggest that hypersensitivity reactions may be a direct result of betahistine's role in increasing histamine levels throughout the body. Hypersensitivity reactions quickly subside after betahistine has been discontinued.
Digestive
Betahistine may also cause several digestive-related side effects. The package insert for Serc, a trade name for betahistine, states that patients may experience several gastrointestinal side effects. These may include nausea, upset stomach, vomiting, diarrhea and stomach cramping. These symptoms are usually not serious and subside between doses. Patients experiencing chronic digestive problems may lower their dose to the minimum effective range and by taking betahistine with meals. Additional digestive problems may require that patients consult their physician in order to find a possible suitable alternative.
Others
People taking betahistine may experience several other side effects ranging from mild to serious. The package insert for Serc states that patients may experience nervous-system side effects, including headache. Some nervous system events may also partly be attributable to the underlying condition rather than the medication used to treat it. The study by Jeck-Thole and Wagner also reports that patients may experience headache and liver problems, including increased liver enzymes and bile-flow disturbances. Any side effects that persist or outweigh the relief of symptoms of the original condition may warrant that the patient consult their physician to adjust or change the medication.
Pharmacology
Pharmacodynamics
Betahistine is a strong antagonist of the histamine H3 receptor and a weak agonist of the histamine H1 receptor.[1]
Betahistine has two mechanisms of action. Primarily, it is a weak agonist on the H1 receptors located on blood vessels in the inner ear. This gives rise to local vasodilation and increased permeability, which helps to reverse the underlying problem of endolymphatic hydrops.
More importantly, betahistine has a powerful antagonistic effects at H3 receptors, thereby increasing the levels of neurotransmitters histamine, acetylcholine, norepinephrine, serotonin, and GABA released from the nerve endings. The increased amounts of histamine released from histaminergic nerve endings can stimulate receptors. This stimulation explains the potent vasodilatory effects of betahistine in the inner ear, that are well documented.
Betahistine seems to dilate the blood vessels within the inner ear which can relieve pressure from excess fluid and act on the smooth muscle.
It is postulated that betahistine's increase in the level of serotonin in the brainstem inhibits the activity of vestibular nuclei.
Pharmacokinetics
Betahistine comes in both a tablet form as well as an oral solution, and is taken orally. It is rapidly and completely absorbed. The mean plasma elimination half-life is 3 to 4 hours, and excretion is virtually complete in the urine within 24 hours. Plasma protein binding is very low. Betahistine is transformed into aminoethylpyridine and hydroxyethylpyridine and excreted with the urine as pyridylacetic acid. There is some evidence that one of these metabolites, aminoethylpyridine, may be active and exert effects similar to those of betahistine on ampullar receptors.[5]
Chemistry
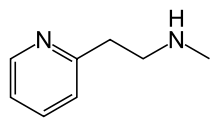
Betahistine chemically is 2-[2-(methylamino)ethyl]pyridine, and is formulated as the dihydrochloride salt. Its chemical structure closely resembles those of phenethylamine and histamine.
Society and culture
Brand names
Betahistine is marketed under a number of brand names, including Veserc, Serc, Hiserk, Betaserc, Solvay, and Vergo.
Availability
Betahistine is widely used and available in Europe, including in the United Kingdom.[1] It was approved by the Food and Drug Administration in the early 1970s for Ménière’s disease, but approval was later withdrawn for lack of evidence of efficacy. The withdrawal was upheld by a US court of appeals in 1968.
References
- Anthony Dickenson (12 January 2017). Drugs in Neurology. Oxford University Press. pp. 408–409. ISBN 978-0-19-966436-8.
- Rebecca White; Vicky Bradnam (11 March 2015). Handbook of Drug Administration via Enteral Feeding Tubes, 3rd edition. Pharmaceutical Press. pp. 125–. ISBN 978-0-85711-162-3.
- Adriana P. Tiziani (1 June 2013). Havard's Nursing Guide to Drugs. Elsevier Health Sciences. pp. 1063–. ISBN 978-0-7295-8162-2.
- Sokolova L, Hoerr R, Mishchenko T (2014). "Treatment of Vertigo: A Randomized, Double-Blind Trial Comparing Efficacy and Safety of Ginkgo biloba Extract EGb 761 and Betahistine". Int J Otolaryngol. 2014: 682439. doi:10.1155/2014/682439. PMC 4099171. PMID 25057270.
- Botta L, Mira E, Valli S, Zucca G, Perin P, Benvenuti C, Fossati A, Valli P (June 2001). "Effects of betahistine and of its metabolites on vestibular sensory organs". Acta Otorhinolaryngol Ital. 21 (3 Suppl 66): 24–30. PMID 11677836.