Benign tumor
A benign tumor is a mass of cells (tumor) that lacks the ability to invade neighboring tissue (spread throughout the body) or metastasize. However, they can sometimes be quite large. When removed, benign tumors usually do not grow back, whereas malignant tumors sometimes do. Unlike most benign tumors elsewhere in the body, benign brain tumors can be life threatening.[1] Benign tumors generally have a slower growth rate than malignant tumors and the tumor cells are usually more differentiated (cells have normal features).[2][3][4] They are typically surrounded by an outer surface (fibrous sheath of connective tissue) or remain with the epithelium.[5] Common examples of benign tumors include moles and uterine fibroids.
| Benign tumor | |
|---|---|
| Normal Epidermis and Dermis with Intradermal Nevus 10x-cropped | |
| Specialty | Pathology |
| Prognosis | I |
Although benign tumors will not metastasize or locally invade tissues, some types may still produce negative health effects. The growth of benign tumors produces a "mass effect" that can compress tissues and may cause nerve damage, reduction of blood to an area of the body (ischaemia), tissue death (necrosis) and organ damage. The health effects of the tumor may be more prominent if the tumor is within an enclosed space such as the cranium, respiratory tract, sinus or inside bones. Tumors of endocrine tissues may overproduce certain hormones, especially when the cells are well differentiated. Examples include thyroid adenomas and adrenocortical adenomas.[2]
Although most benign tumors are not life-threatening, many types of benign tumors have the potential to become cancerous (malignant) through a process known as tumor progression.[6] For this reason and other possible negative health effects, some benign tumors are removed by surgery.[7]
Signs and symptoms
Benign tumors are very diverse, and may be asymptomatic or may cause specific symptoms depending on their anatomic location and tissue type. They grow outwards, producing large rounded masses, which can cause what is known as a "mass effect". This growth can cause compression of local tissues or organs, which can cause many effects such as blockage of ducts, reduced blood flow (ischaemia), tissue death (necrosis) and nerve pain or damage.[2] Some tumors also produce hormones that can lead to life-threatening situations. Insulinomas can produce large amounts of insulin leading to hypoglycemia.[8][9] Pituitary adenomas can cause elevated levels of hormones such as growth hormone and insulin-like growth factor-1, which cause acromegaly; prolactin; ACTH and cortisol, which cause Cushings disease; TSH, which causes hyperthyroidism; and FSH and LH.[10] Bowel intussusception can occur with various benign colonic tumors.[11] Cosmetic effects can be caused by tumors, especially those of the skin, possibly causing psychological effects on the person with the tumor.[12] Vascular tumors can bleed, which in some cases can be substantial, leading to anemia.[13]
Causes
PTEN hamartoma syndrome
PTEN hamartoma syndrome comprises four distinct hamartomatous disorders characterised by genetic mutations in the PTEN gene; Cowden syndrome, Bannayan-Riley-Ruvalcaba syndrome, Proteus syndrome and Proteus-like syndrome. Although they all have distinct clinical features, the formation of hamartomas is present in all four syndromes. PTEN is a tumor suppressor gene that is involved in cellular signalling. Absent or dysfunctional PTEN protein allows cells to over-proliferate, causing hamartomas.[14]
Cowden syndrome is an autosomal dominant genetic disorder characterised by multiple benign hamartomas (trichilemmomas and mucocutaneous papillomatous papules) as well as a predisposition for cancers of multiple organs including the breast and thyroid.[15][16] Bannayan-Riley-Ruvalcaba syndrome is a congenital disorder characterised by hamartomatous intestinal polyposis, macrocephaly, lipomatosis, hemangiomatosis and glans penis macules.[14][17] Proteus syndrome is characterised by nevi, asymmetric overgrowth of various body parts, adipose tissue dysregulation, cystadenomas, adenomas, vascular malformation.[18][19]

Familial adenomatous polyposis
Familial adenomatous polyposis (FAP) is a familial cancer syndrome caused by mutations in the APC gene. In this disorder adenomatous polyps are present in the colon that invariably progress into colon cancer.[20] The APC gene is a tumor suppressor and its product is involved in many cellular processes. Inactivation of the APC gene leads to a buildup of a protein called β-catenin, which activates two transcription factors; T-cell factor (TCF) and lymphoid enhancer factor (LEF). These cause the upregulation of many genes involved in cell proliferation, differentiation, migration and apoptosis (programmed cell death), causing the growth of benign tumors.[21]
Tuberous sclerosis complex
Tuberous sclerosis complex (TSC) is an autosomal dominant genetic disorder caused by mutations in the genesTSC1 and TSC2, which produce the proteins hamartin and tuberin, respectively. This disorder presents with many benign hamartomatous tumors including angiofibromas, renal angiomyolipomas, pulmonary lymphangiomyomatosis. Tuberin and hamartin inhibit the mTOR protein in normal cellular physiology and the inactivation of the TSC tumor suppressors causes an increase in mTOR activity. This leads to the activation of genes and the production of proteins that increase cell growth.[22][23][24]
Von Hippel-Lindau disease
Von Hippel-Lindau disease is a dominantly inherited cancer syndrome that massively increases the risk of various tumors including benign hemangioblastomas and malignant pheochromocytomas, renal cell carcinomas, pancreatic endocrine tumors and endolymphatic sac tumors. It is caused by genetic mutations in the Von Hippel–Lindau tumor suppressor gene. The VHL protein (pVHL) is involved in cellular signalling in oxygen starved (hypoxic) cells. One role of pVHL is to cause the cellular degradation of another protein, HIF1α. Dysfunctional pVHL leads to accumulation of HIF1α, which in turn activates the production of several genes involved in cell growth and blood vessel production (VEGF, PDGFβ, TGFα and erythropoietin).[25]
Mechanism
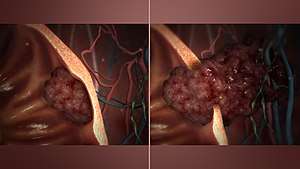
Benign vs malignant
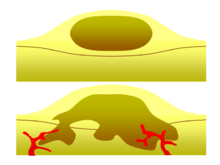
One of the most important factors in classifying a tumor as benign or malignant is its invasive potential. If a tumor lacks the ability to invade adjacent tissues or spread to distant sites by metastasizing then it is benign, whereas invasive or metastatic tumors are malignant.[2] For this reason, benign tumors are not classed as cancer.[3] Benign tumors will grow in a contained area usually encapsulated in a fibrous connective tissue capsule. The growth rates of benign and malignant tumors also differ; benign tumors generally grow more slowly than malignant tumors. Although benign tumors pose a lower health risk than malignant tumors, they both can be life-threatening in certain situations. There are many general characteristics which apply to either benign or malignant tumors, but sometimes one type may show characteristics of the other. For example, benign tumors are mostly well differentiated and malignant tumors are often undifferentiated. However, undifferentiated benign tumors and differentiated malignant tumors can occur.[26][27] Although benign tumors generally grow slowly, cases of fast-growing benign tumors have also been documented.[28] Some malignant tumors are mostly non-metastatic such as in the case of basal cell carcinoma.[4] CT and chest radiography can be a useful diagnostic exam in visualizing a benign tumor and differentiating it from a malignant tumor. The smaller the tumor on a radiograph the more likely it is to be benign as 80% of lung nodules less than 2 cm in diameter are benign. Most benign nodules are smoothed radiopaque densities with clear margins but these are not exclusive signs of benign tumors.[29]
Multistage carcinogenesis
Tumors are formed by carcinogenesis, a process in which cellular alterations lead to the formation of cancer. Multistage carcinogenesis involves the sequential genetic or epigenetic changes to a cell's DNA, where each step produces a more advanced tumor. It is often broken down into three stages; initiation, promotion and progression, and several mutations may occur at each stage. Initiation is where the first genetic mutation occurs in a cell. Promotion is the clonal expansion (repeated division) of this transformed cell into a visible tumor that is usually benign. Following promotion, progression may take place where more genetic mutations are acquired in a sub-population of tumor cells. Progression changes the benign tumor into a malignant tumor.[6][30] A prominent and well studied example of this phenomenon is the tubular adenoma, a common type of colon polyp which is an important precursor to colon cancer. The cells in tubular adenomas, like most tumors which frequently progress to cancer, show certain abnormalities of cell maturation and appearance collectively known as dysplasia. These cellular abnormalities are not seen in benign tumors that rarely or never turn cancerous, but are seen in other pre-cancerous tissue abnormalities which do not form discrete masses, such as pre-cancerous lesions of the uterine cervix. Some authorities prefer to refer to dysplastic tumors as "pre-malignant", and reserve the term "benign" for tumors which rarely or never give rise to cancer.
Diagnosis
Classification
Benign neoplasms are typically but not always composed of cells which bear a strong resemblance to a normal cell type in their organ of origin. These tumors are named for the cell or tissue type from which they originate, followed by the suffix "-oma" (but not -carcinoma, -sarcoma, or -blastoma, which are generally cancers). For example, a lipoma is a common benign tumor of fat cells (lipocytes), and a chondroma is a benign tumor of cartilage-forming cells (chondrocytes). Adenomas are benign tumors of gland-forming cells, and are usually specified further by their cell or organ of origin, as in hepatic adenoma (a benign tumor of hepatocytes, or liver cells). Teratomas contain many cell types such as skin, nerve, brain and thyroid, among others, because they are derived from germ cells.[4] Hamartomas are a group of benign tumors that have relatively normal cellular differentiation but the architecture of the tissue is disorganised.[22] There are a few cancers with 'benign-sounding' names which have been retained for historical reasons, including melanoma (a cancer of pigmented skin cells, or melanocytes) and seminoma (a cancer of male reproductive cells).[32] Skin tags, vocal chord polyps and hyperplastic polyps of the colon are often referred to as benign but they are actually overgrowths of normal tissue rather than neoplasms.[4]
Treatment
Some benign tumors need no treatment; others may be removed if they cause problems such as seizures, discomfort or cosmetic concerns. Surgery is usually the most effective approach and is used to treat most benign tumors. In some case other treatments may be of use. Adenomas of the rectum may be treated with sclerotherapy, a treatment in which chemicals are used to shrink blood vessels in order to cut off the blood supply.[13] Most benign tumors do not respond to chemotherapy or radiation therapy, although there are exceptions; benign intercranial tumors are sometimes treated with radiation therapy and chemotherapy under certain circumstances.[33][34] Radiation can also be used to treat hemangiomas in the rectum.[13] Benign skin tumors are usually surgically resected but other treatments such as cryotherapy, curettage, electrodesiccation, laser therapy, dermabrasion, chemical peels and topical medication are used.[35][36]
References
- "What Is Cancer?". National Cancer Institute. Retrieved 2017-11-26.

- Wilson, Kathleen Atkins; Waugh, Anne; Chambers, Graeme; Grant, Allison; Ross, Janet (2006). Ross and Wilson anatomy and physiology in health and illness. Edinburgh: Churchill Livingstone. pp. 53–54. ISBN 0-443-10101-9.
- Nunn, Laura Silverstein; Silverstein, Alvin; Silverstein, Virginia B. (2006). Cancer. Brookfield, Conn: Twenty-First Century Books. pp. 11–12. ISBN 0-7613-2833-5.
- David Lowell Strayer; Raphael Rubin; Rubin, Emanuel (2008). Rubin's pathology: clinicopathologic foundations of medicine. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 138–139. ISBN 0-7817-9516-8.
- Ober, William B.; Martini, Frederic (2006). Fundamentals of anatomy & physiology. San Francisco: Pearson Benjamin Cummings. ISBN 0-321-31198-1.
- Clark WH (October 1991). "Tumour progression and the nature of cancer". Br. J. Cancer. 64 (4): 631–44. doi:10.1038/bjc.1991.375. PMC 1977704. PMID 1911211.
- Reece, Jane; Campbell, Neil; Urry, Lisa (2005). Biology. San Francisco: Pearson Benjamin Cummings. p. 232. ISBN 0-321-27045-2.
- Marks V, Teale JD (June 1991). "Tumours producing hypoglycaemia". Diabetes Metab Rev. 7 (2): 79–91. doi:10.1002/dmr.5610070202. PMID 1665409.
- Grant CS (October 2005). "Insulinoma". Best Pract Res Clin Gastroenterol. 19 (5): 783–98. doi:10.1016/j.bpg.2005.05.008. PMID 16253900.
- Charis Eng; DeLellis, Ronald A.; Lloyd, Ricardo V.; Phillipp U. Heitz (2004). Pathology and genetics of tumours of endocrine organs. Lyon: IARC Press. ISBN 92-832-2416-7.
- Gill SS, Heuman DM, Mihas AA (October 2001). "Small intestinal neoplasms". J. Clin. Gastroenterol. 33 (4): 267–82. doi:10.1097/00004836-200110000-00004. PMID 11588539.
- Tromberg J, Bauer B, Benvenuto-Andrade C, Marghoob AA (2005). "Congenital melanocytic nevi needing treatment". Dermatol Ther. 18 (2): 136–50. doi:10.1111/j.1529-8019.2005.05012.x. PMID 15953143.
- M. Zuber; F. Harder (2001). Benign tumors of the colon and rectum. Munich: Zuckschwerdt: Surgical Treatment: Evidence-Based and Problem-Oriented.
- Hobert JA, Eng C (October 2009). "PTEN hamartoma tumor syndrome: an overview". Genet. Med. 11 (10): 687–94. doi:10.1097/GIM.0b013e3181ac9aea. PMID 19668082.
- Pilarski R, Eng C (May 2004). "Will the real Cowden syndrome please stand up (again)? Expanding mutational and clinical spectra of the PTEN hamartoma tumour syndrome". J. Med. Genet. 41 (5): 323–6. doi:10.1136/jmg.2004.018036. PMC 1735782. PMID 15121767.
- Eng C (November 2000). "Will the real Cowden syndrome please stand up: revised diagnostic criteria". J. Med. Genet. 37 (11): 828–30. doi:10.1136/jmg.37.11.828. PMC 1734465. PMID 11073535.
- Eng C (September 2003). "PTEN: one gene, many syndromes". Hum. Mutat. 22 (3): 183–98. doi:10.1002/humu.10257. PMID 12938083.
- Blumenthal GM, Dennis PA (November 2008). "PTEN hamartoma tumor syndromes". Eur. J. Hum. Genet. 16 (11): 1289–300. doi:10.1038/ejhg.2008.162. PMID 18781191.
- Cohen MM (August 2005). "Proteus syndrome: an update". Am J Med Genet C Semin Med Genet. 137C (1): 38–52. doi:10.1002/ajmg.c.30063. PMID 16010681.
- Galiatsatos P, Foulkes WD (February 2006). "Familial adenomatous polyposis". Am. J. Gastroenterol. 101 (2): 385–98. doi:10.1111/j.1572-0241.2006.00375.x. PMID 16454848.
- Aoki K, Taketo MM (October 2007). "Adenomatous polyposis coli (APC): a multi-functional tumor suppressor gene". J. Cell Sci. 120 (Pt 19): 3327–35. doi:10.1242/jcs.03485. PMID 17881494.
- Inoki K, Corradetti MN, Guan KL (January 2005). "Dysregulation of the TSC-mTOR pathway in human disease". Nat. Genet. 37 (1): 19–24. doi:10.1038/ng1494. PMID 15624019.
- Crino PB, Nathanson KL, Henske EP (September 2006). "The tuberous sclerosis complex". N. Engl. J. Med. 355 (13): 1345–56. doi:10.1056/NEJMra055323. PMID 17005952.
- Kwiatkowski DJ (January 2003). "Tuberous sclerosis: from tubers to mTOR". Ann. Hum. Genet. 67 (Pt 1): 87–96. doi:10.1046/j.1469-1809.2003.00012.x. PMID 12556239.
- Maher ER (December 2004). "Von Hippel-Lindau disease". Curr. Mol. Med. 4 (8): 833–42. doi:10.2174/1566524043359827. PMID 15579030.
- Skorić T, Korsić M, Zarković K, et al. (June 1999). "Clinical and morphological features of undifferentiated monomorphous GH/TSH-secreting pituitary adenoma". Eur. J. Endocrinol. 140 (6): 528–37. doi:10.1530/eje.0.1400528. PMID 10366409.
- Song HJ, Xue YL, Qiu ZL, Luo QY (2012). "Uncommon metastases from differentiated thyroid carcinoma". Hell J Nucl Med. 15 (3): 233–40. doi:10.1967/s002449910059. PMID 23106056.
- Sagel SS, Ablow RC (November 1968). "Hamartoma: on occasion a rapidly growing tumor of the lung". Radiology. 91 (5): 971–2. doi:10.1148/91.5.971. PMID 5681331.
- Erasmus, J.J; Connolly, J.E; McAdams, H.P; Roggli, V.L. (2000). "Solitary pulmonary nodules: Part I. Morphologic evaluation for differentiation of benign and malignant lesions". Scientific exhibit. 20 (1): 43–58. doi:10.1148/radiographics.20.1.g00ja0343. PMID 10682770.
- Barrett JC (April 1993). "Mechanisms of multistep carcinogenesis and carcinogen risk assessment". Environ. Health Perspect. 100: 9–20. doi:10.1289/ehp.931009. PMC 1519586. PMID 8354184.
- Wujcik, Debra; Yarbro, Connie Henke; Barbara H. Gobel (2011). Cancer nursing: principles and practice. Boston: Jones and Bartlett Publishers. ISBN 0-7637-6357-8.
- Ramzi Cotran; Vinay Kumar; Tucker Collins (1999). Robbins Pathologic Basis of Disease (6th ed.). W.B. Saunders. ISBN 0-7216-7335-X.
- Brada M (February 2013). "Radiotherapy for benign brain tumours coming of age; example of vestibular schwannoma". Radiother Oncol. 106 (2): 157–60. doi:10.1016/j.radonc.2013.01.009. PMID 23462704.
- Sioka C, Kyritsis AP (March 2009). "Chemotherapy, hormonal therapy, and immunotherapy for recurrent meningiomas". J. Neurooncol. 92 (1): 1–6. doi:10.1007/s11060-008-9734-y. PMID 19023520.
- Luba MC, Bangs SA, Mohler AM, Stulberg DL (February 2003). "Common benign skin tumors". Am Fam Physician. 67 (4): 729–38. PMID 12613727.
- Marghoob AA, Borrego JP, Halpern AC (December 2007). "Congenital melanocytic nevi: treatment modalities and management options". Semin Cutan Med Surg. 26 (4): 231–40. doi:10.1016/j.sder.2008.03.007. PMID 18395671.
External links
| Classification |
|---|