Veterans benefits for post-traumatic stress disorder in the United States
The United States has sought to compensate military veterans for service-related injuries since the Revolutionary War, with the current indemnity model established near the end of World War I. The Department of Veterans Affairs (VA) began to provide disability benefits for post-traumatic stress disorder (PTSD) in the 1980s after the diagnosis became part of official psychiatric nosology.

Limited research suggests that VA disability benefits achieve their goal of helping veterans suffering from PTSD. The Veterans Benefits Administration (VBA), a component of the Department of Veterans Affairs, processes disability claims and administers all aspects of the VA disability program. Since 1988 VA disability claim decisions have been subject to federal court review.
Disability ratings theoretically represent a veteran's "average impairment in earnings capacity", on a scale from 0 to 100. Veterans who file a disability claim due to PTSD almost always receive a compensation and pension examination (C&P exam) by VA-employed or VA-contracted psychologists or psychiatrists. Social scientists and others have expressed concern about the consistency and accuracy of PTSD C&P exam findings, although the VA generally rejects such concerns as unfounded or exaggerated.
Recent efforts to change VA disability benefits for PTSD include urging the VA to place more emphasis on vocational rehabilitation and treatment versus cash payments; revising the General Rating Formula for Mental Disorders to better reflect problems experienced by veterans with PTSD; and considering a veteran's quality of life when determining the disability rating.
VA disability benefits for PTSD
The United States provides a wide range of benefits for veterans with posttraumatic stress disorder (PTSD), which was incurred in, or aggravated by, their military service.[1] The United States Department of Veterans Affairs (VA) will provide benefits[2] to veterans that the VA has determined suffer from PTSD, which developed during, or as a result of, their military service. These benefits not only include tax-free cash payments[3] but can also include free or low-cost mental health treatment and other healthcare;[4] vocational rehabilitation services;[5] employment assistance;[6][7] independent living support;[8] and more.[9]
History

Since the founding of the country, the United States has sought to compensate the men and women who have served in its armed forces.[10] Near the end of World War I, the U.S. Congress passed legislation establishing an indemnity model for veterans disability benefits.[11] Since that year, compensation has been provided to veterans suffering from physical or mental disabilities that were incurred during, or aggravated by, military service, and which have adversely impacted the veteran's ability to work. The amount of compensation provided—both cash payments and VA-sponsored services—are based on the veteran's average impairment in earnings capacity.[12]
Service-connection
Service-connected means that a veteran has a disease or injury that is "connected" to his or her military service; that is, the disease or injury was incurred in, or aggravated by, his or her military service.[13]
Post-traumatic stress disorder
Post-traumatic stress disorder[lower-alpha 1] (PTSD) may develop following exposure to an extremely threatening or horrific event. It is characterized by several of the following signs or symptoms: Unwanted re-experiencing of the traumatic event, such as vivid, intense, and emotionally-laden intrusive memories, dissociative flashback episodes, or nightmares; active avoidance of thoughts, memories, or reminders of the event; hyperarousal symptoms such as always being "on guard" for danger, enhanced (exaggerated) startle response, insomnia, trouble concentrating, or chronic irritability; anhedonia, social detachment, excessively negative thoughts about oneself or the world, marked guilt or shame, or a persistent depressed or anxious mood.[14][15]
PTSD is the third most compensated disability after hearing loss and tinnitus.[16]
Traumatic stressor
Matthew J. Friedman of the National Center for PTSD notes that PTSD is unique among mental health probelms because of the great importance placed upon the cause, the traumatic stressor.[17]
A traumatic stressor is an event that meets Criterion A of the DSM-5 diagnostic criteria for PTSD, which requires, in part, that an individual "... was exposed to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence ...."[18][19]
Veterans filing a disability claim for PTSD complete a form describing the traumatic stressors they endured during their military service.[20] VA has separate forms for PTSD generally[21] and PTSD "secondary to personal assault".[22]
Diagnosis
Prior to 2014, VA C&P examiners determined if a veteran suffered from PTSD based on DSM-IV diagnostic criteria for the disorder. VA updated most of its relevant regulations in August 2014 to reflect the publication of DSM-5.[23][lower-alpha 2][lower-alpha 3]
Effectiveness
Whether disability benefits adequately compensate veterans with PTSD for loss in average earning capacity has been debated. A 2007 study found that older veterans age 65 and up rated at 50% disabled or higher for PTSD, including individual unemployability (IU) benefits,[24] receive more in compensation (plus any earned income and retirement benefits such as Social Security or pensions) than nondisabled veterans earn in the workforce and/or receive in Social Security and other retirement benefits.[25] However, younger veterans (age 55 and below) generally receive less in compensation benefits (plus any earned income) than their non-disabled counterparts earn via employment. For example, the parity ratio[lower-alpha 4] for a 25-year-old veteran rated 100% disabled by PTSD is 0.75, and for a 35-year-old veteran rated 100% disabled by PTSD the ratio is 0.69. The parity ratio for a 75-year-old veteran receiving IU benefits is 6.81.[25]
Research based on data collected in the 1990s indicates that veterans receiving disability benefits for PTSD experience a reduction in PTSD symptom severity, and have lower rates of poverty and homelessness.[26] A 2017 study found that "denied" veterans (those who applied for—but did not receive—disability compensation) exhibit significantly worse overall health, functional limitations, poverty, and social isolation, when compared to veterans who were awarded VA disability benefits.[27]
In addition to lost income, a Congressionally-mandated commission,[28] argued that the VA disability benefits program should compensate veterans for non-economic losses, particularly with regard to a veteran's overall quality of life. The U.S. Government Accountability Office analyzed this recommendation and suggested that it be considered as one of three major changes to modernize the VA disability benefits program.[29]
Some scholars argue that the VA disability benefits program is "countertherapeutic" because it provides no incentives to overcome symptoms and problems caused by the disorder, and, in fact rewards veterans for staying sick,[30][31][32] while other researchers take issue with this assertion.[33] In a similar vein, a military scholar suggests that current VA disability benefits policy inculcates in veterans a lack of self-efficacy and fosters dependency.[34][35]
Claims process
Eligibility
In order to be eligible for VA benefits, a veteran must have been discharged under other than dishonorable conditions.[36] Stated differently, if a veteran received a Bad Conduct discharge or a Dishonorable discharge they will, under most circumstances, not be eligible for VA benefits.[37]
Types of military service

Federal regulations describe three categories of military service, active duty, active duty for training, and inactive duty training.[38] Eligibility for VA disability compensation requires that the veteran's service occurred during one of these three categories.[39] The definition of active duty military service includes "service at any time as a cadet at the United States Military, Air Force, or Coast Guard Academy, or as a midshipman at the United States Naval Academy."[38]
In line of duty and exceptions
There are exceptions to the general rule that injuries or diseases incurred in, or aggravated by, military service are eligible for VA disability compensation benefits. For example, such injuries or diseases must meet the in line of duty criteria. "In line of duty means an injury or disease incurred or aggravated during a period of active military, naval, or air service unless such injury or disease was the result of the veteran's own willful misconduct or ... was a result of his or her abuse of alcohol or drugs."[40]
Evidence
In order for a veteran to receive disability benefits for PTSD, the Veterans Benefits Administration (VBA), an organizational element of the VA, based on their review of medical and psychological evidence, must conclude that the veteran indeed has PTSD that developed as a result of military service. Reaching such a determination usually requires that the veteran receive a Compensation and Pension examination (C&P exam),[41] which is a forensic[lower-alpha 5] mental health evaluation[42] conducted by a psychologist or psychiatrist at a local VA medical facility or by a psychologist or psychiatrist in independent practice who conducts evaluations for a VA-contracted private vendor.
Benefits claim procedures
The VA provides a detailed description of the benefits claims process on its website.[43] Briefly, a VSR (Veterans Service Representative),[44] an employee of the Veterans Benefits Administration (VBA), reviews the information submitted by a veteran to determine if VBA needs any additional evidence (e.g., medical records) to adjudicate the claim.
VA has a legal obligation to help veterans obtain any evidence that will support their claim.[45] For example, the VSR might request a veteran's military personnel records, Social Security disability records, or private medical records. The VSR will almost always request a Compensation and Pension examination (C&P exam),[46] also referred to as a VA claim exam.[47]
After VBA obtains all relevant documentation (evidence), an RVSR (Ratings Veterans Service Representative)[48] renders a decision regarding the veteran's claim. The RVSR refers in part to the General Rating Formula for Mental Disorders[49] when making this determination.
Obtaining assistance
Veterans may receive assistance with filing a VA disability compensation claim from a Veterans Service Officer. As the VA states, "[veterans]... can work with a trained professional ... to get help filing a claim for disability compensation."[50] The veteran does not have to pay a Veterans Service Officer for their services.
VA publishes an annual directory of accredited veterans service organizations and state departments of veterans affairs.[51]
Some veterans advocates recommend that veterans learn how to file claims on their own so that they retain full control over the process.[52][53]
Federal court review
The Veterans Judicial Review Act of 1988 established the Court of Appeals for Veterans Claims, an Article I federal tribunal, to review decisions of the Board of Veterans Appeals.[54]
Post-adjudication representation
Veterans may appeal the VBA's decision regarding their compensation claim, and they may ask to be represented by an accredited Veterans Service Officer, attorney, or claims agent in the appeals process. Note that the VA does not require a veteran to be represented on appeal.
VA prohibits attorneys or claims agents from charging a veteran for professional services prior to the adjudication of the veteran's claim.[55]
Unless they agree to work on a pro bono basis, attorneys and claims agents who represent veterans before the Veterans Benefits Administration, Board of Veterans Appeals, and Court of Appeals for Veterans Claims require payment for their services. At the federal court level, most attorneys work for Equal Access to Justice Act fees. These are attorney fees ordered by the court to be paid by the federal government when the government's position in litigation was not "substantially justified."[55]
Disability rating
General rating formula for mental disorders
If VBA determines that a veteran suffers from service-connected PTSD, then they assign a disability rating, expressed as a percentage. This disability rating determines the amount of compensation[56] and other disability benefits the VA provides the veteran. The disability rating indicates the extent to which PTSD has deprived the veteran of his or her average earnings capacity. A rating of 0% indicates that a veteran has PTSD but the disorder has not affected his or her ability to work, whereas a 100% rating theoretically means that the veteran is not capable of working at all because of PTSD.[lower-alpha 6]
The VA assigns disability ratings for PTSD according to the General Rating Formula for Mental Disorders (38 C.F.R. § 4.130),[57] which specifies criteria for disability ratings of 0%, 10%, 30%, 50%, 70%, or 100%.
Some argue that by relying on the current Rating Formula, "VA uses decades-old regulations developed for mental disorders that do not resemble PTSD", and, consequently, "[i]rrelevant criteria ... may outweigh ... more relevant factors, leading VA to undercompensate veterans with valid diagnoses of PTSD."[58] Similarly, veterans service organizations have argued, for example, that a "... veteran service connected for schizophrenia and another veteran service connected for another psychiatric disorder should not be evaluated using the same general formula" and have supported efforts to revise the Rating Formula.[59]
Concern has been expressed by some RSVRs[48] (VBA "raters" who adjudicate claims) that automated software discourages their use of independent judgment to evaluate the claim as a whole, a charge senior VA officials reject.[60]
Since 2001, the VA has been revising its disability rating schedule to incorporate medical advances that have occurred since the last review, update medical terminology, add medical conditions not currently in the Rating Schedule, and refine criteria for further clarity, consistency and ease of rater application.[61] The General Rating Formula for Mental Disorders has not yet been updated.
Claims for an increased disability rating
A veteran currently receiving compensation for service-connected PTSD may file a claim for an increase in his or her disability rating if PTSD symptom severity and related functional impairment has worsened.[62]
Individual unemployability
Under certain conditions,[63] veterans receiving service-connected disability compensation for PTSD may file a claim for individual unemployability.[24][64] If the Veterans Benefits Administration concludes that PTSD, either alone or in combination with other service-connected disabilities, would make it "... impossible for the average person to follow a substantially gainful occupation...",[65] the veteran will receive disability compensation at the 100% rate, even though their actual ("schedular") rating[lower-alpha 7] is less than 100%.[66]
PTSD C&P exam
As noted above, VBA almost always requires a compensation and pension examination (C&P exam), also known as a VA claim exam,[47] for veterans claiming service-connected PTSD. There are two types of PTSD C&P exams: Initial and Review. The Initial PTSD exam must be conducted by a VA psychologist or psychiatrist certified by the VHA Office of Disability and Medical Assessment (DMA)[67] to evaluate veterans for this purpose.[68]
The definition of "VA psychologist or psychiatrist" includes psychologists and psychiatrists in the private sector who conduct C&P exams for a Medical Disability Evaluation (MDE) company under contract with the Veterans Benefits Administration (VBA).[69] The companies with current VBA contracts[70] are Logistics Health, Inc. (LHI);[71] Veterans Evaluation Services (VES);[72] Vet Fed;[73] and QTC[74] (QTC in turn contracts with Magellan Health to manage their network of providers).[75]
The Review PTSD exam may be completed by VA or non-VA psychologists and psychiatrists. Clinical or counseling psychology interns, psychiatric residents, licensed clinical social workers, nurse practitioners, physician assistants, and clinical nurse specialists may also conduct review PTSD exams, although they must be "closely supervised" by a psychologist or psychiatrist.[76]
Concerns about reliability
Researchers, current and former VA psychologists, investigative journalists, and individual veterans have expressed concerns about the inter-rater reliability and validity of C&P exams for PTSD. For example:
- Some current or former VA psychologists assert that VA medical centers do not allocate enough time for C&P psychologists and psychiatrists to conduct a thorough, evidence-based assessment, with less time presumably reducing the reliability and validity of the results.[77][78]
- Research has demonstrated marked regional variance with regard to the proportion of veteran claimants who receive VA disability compensation for PTSD.[79][80]
- A survey of C&P psychologists revealed that only 15% followed VA's own guidance regarding best practices[81] for PTSD compensation and pension exams.[82] For example, one of the best practice recommendations is to assess veterans for PTSD using the Clinician-Administered PTSD Scale (CAPS),[83] particularly given empirical evidence that using the CAPS improves PTSD C&P exam reliability and validity,[84] but the vast majority of C&P psychologists do not use this validated instrument according to the survey.
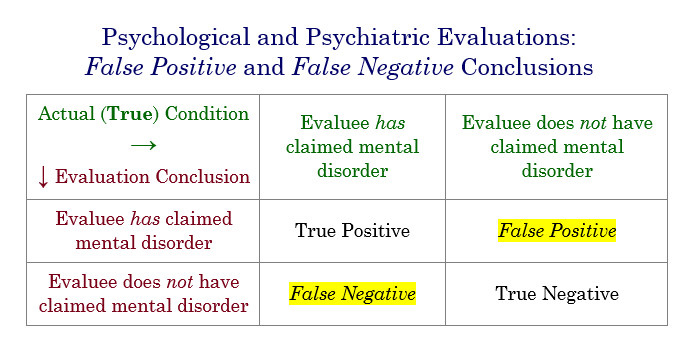 Four possible outcomes of a psychological evaluation, including false positive and false negative conclusions.
Four possible outcomes of a psychological evaluation, including false positive and false negative conclusions.- An empirical study published in 2017 suggested C&P examiner racial bias might have led to an increased rate of false negative[85] conclusions (regarding PTSD diagnosis and service connection) for Black veterans, and a high rate of false positive[86] conclusions for White veterans.[87] This finding corresponds with past research[88][89] and legal scholarship[90] discussing the potential for implicit racial biases on the part of mental health clinicians in general, and C&P psychologists and psychiatrists in particular.
- Some VA facilities prohibit examiners from using symptom validity tests to screen or assess for malingering and other forms of dissimulation.[78][91][92]
- Several researchers have published empirical studies in peer-reviewed scholarly journals pointing to significant rates of both false positive and false negative PTSD C&P exam conclusions.[93][94][95][96][97][98]
- Social scientists conducted independent PTSD assessments of veterans who had filed disability benefits claims for PTSD, some of whom had been awarded service-connected compensation for PTSD and some had not. The study found significant rates of both false positive and false negative VBA adjudicative decisions.[99] Although VBA adjudicators rely on other sources of evidence, in addition to C&P exam results, VBA almost always requests a C&P exam for PTSD claims,[100][101] and C&P exam results significantly influence VBA determinations.[102][103][104]
- Investigative journalists' reports,[105][106] newspaper editorials,[107][108] and individual combat veterans,[109][110][111][112] assert that a sizable percentage of veterans filing PTSD disability claims exaggerate or feign PTSD symptoms.
Disability Benefits Questionnaire
Mental health professionals document the results of Initial and Review PTSD C&P exams on a Disability Benefits Questionnaire (DBQ).[113] The VA developed Disability Benefit Questionnaires (DBQs) to streamline the VBA ratings process and thereby complete the claims process faster. In addition, veterans may ask their treating clinicians to complete a DBQ and possibly bypass the need for a C&P exam.[114] However, it is important to note that the VA discourages their mental health clinicians from completing DBQs for their patients,[115] and similar recommendations have been offered to private psychologists and psychiatrists whose patients ask them to complete DBQs,[116] because it potentially creates a conflict of interest due to a dual role relationship (serving simultaneously as a treating clinician and a forensic evaluator).[117][118]
C&P psychologists have expressed concern that the DBQ "Symptom List" (Section II, Number 5 on the Initial PTSD DBQ;[lower-alpha 8] Section VII on the Review PTSD DBQ;[119] and Section III on the Mental Disorders DBQ[120])[lower-alpha 9] contains a series of signs, symptoms, and descriptions of functional impairment without any guidance regarding when these items should be endorsed.[121][122] [lower-alpha 10] These C&P examiners argue that such guidance is important because otherwise C&P examiners will (necessarily) use their own idiosyncratic judgments regarding when to endorse each item in the "Symptom List". In addition, the disability rating may be based largely on which "Symptom List" items are endorsed, since these items are drawn verbatim from the examples given for each level of impairment in the General Rating Formula for Mental Disorders.[lower-alpha 11]
Notes
- The present article uses the hyphenated spelling, "post-traumatic", whereas the main Wikipedia article on the disorder, Posttraumatic stress disorder, uses the unhyphenated spelling preferred by the American Psychiatric Association and used in DSM-5.
- Claims that were appealed before August 4, 2014 would still use DSM-IV PTSD diagnostic criteria. See 79 Fed. Reg. 45093 at 45094 ("The Secretary does not intend for the provisions of this interim final rule to apply to claims that have been certified for appeal to the Board of Veterans' Appeals or are pending before the Board of Veterans' Appeals, the United States Court of Appeals for Veterans Claims, or the United States Court of Appeals for the Federal Circuit.")
- There is an exception: Although 38 C.F.R. § 3.304(f) ("Posttraumatic stress disorder") refers to 38 C.F.R. 4.125(a) ("Service connection for posttraumatic stress disorder requires medical evidence diagnosing the condition in accordance with §4.125(a) of this chapter ..."), which specifies use of DSM-5, 38 C.F.R. § 3.304(f)(3) was not changed to correspond with DSM-5 PTSD diagnostic criteria. Specifically, the definition of "fear of hostile military or terrorist activity" contains, almost verbatim, language from DSM-IV PTSD diagnostic criterion A: "For purposes of this paragraph, 'fear of hostile military or terrorist activity' means that a veteran experienced, witnessed, or was confronted with an event or circumstance that involved actual or threatened death or serious injury, or a threat to the physical integrity of the veteran or others, [DSM-IV criterion A1] ... and the veteran's response to the event or circumstance involved a psychological or psycho-physiological state of fear, helplessness, or horror." [DSM-IV criterion A2]). The VA's notice in the Federal Register does not explain why 38 C.F.R. § 3.304(f)(3) still uses DSM-IV diagnostic criteria.
- The CNA report cited herein describes the parity ratio as: "A ratio of exactly 1 would be perfect parity, indicating that the earnings of disabled veterans, plus their VA compensation, gives them the same lifetime earnings as their peers. A ratio of less than one would mean that the service-disabled veterans receive less than their peers on average, while a ratio of greater than one would mean that they receive more than their peers."
- Note that the term forensic in this context simply means legally-related and does not necessarily have anything to do with criminal law or law enforcement. The veterans disability benefits claims process for PTSD is ultimately a legal proceeding, which is why PTSD C&P examinations are categorized as psycholegal, medicolegal, or, most commonly, forensic mental health evaluations.
- The adverb 'theoretically' is used here because the Rating Formula is based on signs and symptoms, not occupational impairment. While the symptoms associated with the 100% rating for mental disorders often cause significant occupational impairment, e.g., "persistent delusions or hallucinations" or "persistent danger of hurting self or others", they do not necessarily render a veteran unable to work.
- VBA bases a veteran's schedular rating on the rating schedule. The rating schedule for PTSD and other mental disorders has a slightly different name than nonpsychiatric medical and audiological rating schedules. Instead of being called a "rating schedule", it's called the "General Rating Formula" (for Mental Disorders).
- The Initial PTSD DBQ is available on the VA intranet only.
- Note that the outline enumeration for the various parts of the DBQs, e.g., "Sections", in Roman numerals, or "Numbers", in Arabic numerals, differ from one DBQ to another, i.e., they are not uniform.
- See also (for a legal perspective): Ridgway, J. D. (2012). Mind reading and the art of drafting medical opinions in veterans benefits claims. Psychological Injury and Law, 5(1), 72–87. doi:10.1007/s12207-012-9119-6
- For example, the "Symptom List" contains the following items: flattened affect; circumstantial, circumlocutory, or stereotyped speech; panic attacks more than once a week; difficulty in understanding complex commands; impairment of short- and long-term memory (e.g., retention of only highly learned material, forgetting to complete tasks); impaired judgment; impaired abstract thinking; disturbances of motivation and mood; and difficulty in establishing and maintaining effective work and social relationships. Each of those signs, symptoms, or descriptions of functional impairment are the exact examples given for the 50% level of impairment in the General Rating Formula for Mental Disorders (38 C.F.R. § 4.130). Accordingly, if the C&P examiner endorses one or more of these items, the veteran will likely be assigned a 50% disability rating, all other factors being equal, particularly given the advent of VBA's automated Evaluation Builder software.[123]
References
- Direct service connection; wartime and peacetime—Posttraumatic stress disorder, 38 C.F.R. §3.304(f), eCFR—Code of Federal Regulations, retrieved 2019-10-02
- "Federal Benefits for Veterans, Dependents and Survivors, 2017 Edition". Department of Veterans Affairs. Retrieved 24 June 2018.
- "VA Compensation Rate Table". Department of Veterans Affairs. Retrieved 24 November 2018.
- "Access VA Health Benefits". Department of Veterans Affairs. Retrieved 20 October 2012.
- "VA Vocational Rehabilitation". Department of Veterans Affairs. Retrieved 20 October 2012.
- "Careers and Employment". VA.gov. Retrieved 25 November 2018.
- "Educational and Career Counseling (Chapter 36)". VA.gov. Retrieved 25 November 2018.
- "Independent Living Support for Veterans". Department of Veterans Affairs. Retrieved 25 November 2018.
- "Veterans Benefits". Veterans Benefits Administration. Archived from the original on 26 November 2012. Retrieved 30 November 2012.
- Ridgway, J. (2011). "The splendid isolation revisited: Lessons from the history of veterans benefits before judicial review". Veterans Law Review. 3: 135–219. SSRN 1598344.
- Economic Systems Inc (2004). VA disability compensation program: Legislative history. Washington, DC: VA Office of Policy, Planning and, Preparedness.
- An Act To amend and modify the War Risk Insurance Act, ch. 16, 41 Stat. 371, 373 (1919) ("A schedule of ratings of reductions in earning capacity from specific injuries or combinations of injuries of a permanent nature shall be adopted and applied by the bureau. Ratings may be as high as 100 per annum. The ratings shall be based, as far as practicable, upon the average impairments of earning capacity resulting from such injuries in civil occupations and not upon the impairment in earning capacity in each individual case ...").
- "38 CFR § 3.303 - Principles relating to service connection". Legal Information Institute at Cornell Law School. Retrieved 2019-10-02.
Service connection connotes many factors but basically it means that the facts, shown by evidence, establish that a particular injury or disease resulting in disability was incurred coincident with service in the Armed Forces, or if preexisting such service, was aggravated therein.
- World Health Organization, Post traumatic stress disorder (6B40), International Classification of Diseases, 11th rev., ICD-11 for Mortality and Morbidity Statistics (April 2019).
- Shalev, Arieh Y. and Charles R. Marmar. "Conceptual History of Post-Traumatic Stress Disorder." In Post-Traumatic Stress Disorder, edited by Charles B. Nemeroff and Charles Marmar, 3–30. New York: Oxford University Press, 2018. ISBN 978-0-19-025944-0
- Veterans Benefits Administration, VBA Annual Benefits Report Fiscal Year 2018, Compensation, p. 5, https://www.benefits.va.gov/REPORTS/abr/docs/2018-compensation.pdf
- Friedman, Matthew J. "PTSD History and Overview". National Center for PTSD. Retrieved 3 October 2019.
- Posttraumatic stress disorder, 38 C.F.R. § 3.304(f), ("Service connection for posttraumatic stress disorder requires medical evidence diagnosing the condition in accordance with §4.125(a) of this chapter; a link, established by medical evidence, between current symptoms and an in-service stressor; and credible supporting evidence that the claimed in-service stressor occurred.")
- Diagnosis of mental disorders, 38 C.F.R. § 4.125(a), ("Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), American Psychiatric Association (2013), is incorporated by reference into this section ....")
- "VA disability compensation for PTSD". U.S. Department of Veterans Affairs. 2019-09-27. Retrieved 2019-10-03.
When you file a disability claim, you’ll also need to fill out one of these additional forms: A Statement in Support of Claim for Service Connection for Post-Traumatic Stress Disorder (VA Form 21-0781) or A Statement in Support of Claim for Service Connection for Post-Traumatic Stress Disorder Secondary to Personal Assault (VA Form 21-0781a)
- Dep't Veterans Aff., Veterans Benefits Admin., Statement in Support of Claim for Service Connection for Post-Traumatic Stress Disorder (PTSD) (VA Form 21-0781, rev. July 2017)
- Dep't Veterans Aff., Veterans Benefits Admin., Statement in Support of Claim for Service Connection for Post-Traumatic Stress Disorder (PTSD) Secondary to Personal Assault (VA Form 21-0781a, rev. July 2017)
- Schedule for Rating Disabilities—Mental Disorders and Definition of Psychosis for Certain VA Purposes, Section 4.125: DSM Reference and DSM–5 Nomenclature Change, 79 Fed. Reg. 45093, 45094 (August 4, 2014) (codified at 38 C.F.R. §4.125(a))
- "Individual Unemployability". Veterans Benefits Administration – Compensation. Department of Veterans Affairs. Note: This VA web page briefly describes individual unemployability. Retrieved 15 August 2019.
- Final Report for the Veterans' Disability Benefits Commission: Compensation, Survey Results, and Selected Topics (PDF). The CNA Corporation. August 2007. p. 4. Retrieved 23 August 2014.
- Murdoch, Maureen (1 October 2011). "Long-term outcomes of disability benefits in US veterans with posttraumatic stress disorder". Archives of General Psychiatry. 68 (10): 1072–80. doi:10.1001/archgenpsychiatry.2011.105. PMID 21969464.
Regardless of claim outcome, veterans who apply for PTSD disability benefits are highly impaired. However, receiving PTSD benefits was associated with clinically meaningful reductions in PTSD symptoms and less poverty and homelessness.
- Fried, Dennis Adrian, Marian Passannante, Drew Helmer, Bart K. Holland, and William E. Halperin. "The Health and Social Isolation of American Veterans Denied Veterans Affairs Disability Compensation". Health & Social Work 42, no. 1 (2017). https://doi.org/10.1093/hsw/hlw051
- Scott (USA, Ret.), LTG James Terry (10 October 2007). "Findings Of The Veterans' Disability Benefits Commission". Testimony before the Committee on Veterans' Affairs, U.S. House of Representatives: U.S. Government Printing Office. Retrieved 20 June 2015.
We believe that the level of compensation should be based on the severity of the disability and should make up for the average impairments of earnings capacity and the impact of the disability on functionality and quality of life. ... Current compensation payments do not provide a payment above that required to offset earnings loss. Therefore, there is no current compensation for the impact of disability on the quality of life for most veterans. While permanent quality of life measures are developed, studied, and implemented, we recommend that compensation payments be increased up to 25 percent with priority to the more seriously disabled.
- Office, U. S. Government Accountability (10 September 2012). "VA disability compensation: Actions needed to address hurdles facing program modernization (GAO-12-846)" (GAO-12–846). U.S. Government Accountability Office. Retrieved 20 June 2015.
Three key approaches for modernizing VA's disability programs recommended by disability commissions and others—providing quality of life payments, providing integrated vocational services with transitional cash assistance, and systematically factoring the effects of assistive technology and medical interventions into rating decisions—hold opportunity and challenges. Experts and veteran groups GAO interviewed believe each approach holds at least some opportunity for serving veterans more fairly, equitably, and effectively.
Cite journal requires|journal=(help) - Mossman, D. (1994). "At the VA, it pays to be sick". The Public Interest. 114: 35–47. Retrieved 13 August 2014.
Sadly, a program with good intentions has yielded a series of perverse incentives that reward illness, encourage patients to view themselves as incapacitated, and poison the relationships between patients and their caregivers.
- Frueh, B. C.; Grubaugh, A. L.; Elhai, J. D.; Buckley, T. C. (December 2007). "US Department of Veterans Affairs disability policies for posttraumatic stress disorder: Administrative trends and implications for treatment, rehabilitation, and research". American Journal of Public Health. 97 (12): 2143–45. doi:10.2105/AJPH.2007.115436. PMC 2089098. PMID 17971542.
Department of Veterans Affairs (VA) psychiatric disability compensation and rehabilitation policies for combat-related posttraumatic stress disorder (PTSD), although well intentioned, are more than 60 years old and are seriously flawed.
- Satel, S. (February 2011). "PTSD's diagnostic trap". American Enterprise Institute. Retrieved 13 August 2014.
Told he is disabled, the veteran and his family may assume—often incorrectly—that he is no longer able to work. At home on disability, he risks adopting a "sick role" that ends up depriving him of the estimable therapeutic value of work. Lost are the sense of purpose work gives (or at least the distraction from depressive rumination it provides), the daily structure it affords, and the opportunity for socializing and cultivating friendships. The longer he is unemployed, the more his confidence in his ability and motivation to work erodes and his skills atrophy. Once a patient is caught in such a downward spiral of invalidism, it can be hard to throttle back out. What's more, compensation contingent upon being sick often creates a perverse incentive to remain sick. For example, even if a veteran wants very much to work, he understandably fears losing his financial safety net if he leaves the disability rolls to take a job that ends up proving too much for him. This is how full disability status can undermine the possibility of recovery.
- Marx, Brian P.; Miller, Mark W.; Sloan, Denise M.; Litz, Brett T.; Kaloupek, Danny G.; Keane, Terence M. (May 2008). "Military-related PTSD, current disability policies, and malingering". American Journal of Public Health. 98 (5): 773–74. doi:10.2105/AJPH.2007.133223. PMC 2374833. PMID 18381982.
Frueh et al. present an incomplete picture of the literature and neglect substantial evidence that contradicts their thesis
- Gade, Daniel. "A Better Way to Help Veterans" (PDF). National Affairs. 16 (Summer, 2013): 53–69. Retrieved 13 August 2014.
... VA benefit policies ... distort incentives and encourage veterans to live off of government support instead of working to their full capability. Adding to the problem is a culture of low expectations, fostered by the misguided understanding of 'disability' upon which both federal policy and private philanthropy are often based. The result is that, for many veterans, a state of dependency that should be temporary instead becomes permanent.
- Phillips, Dave (7 January 2015). "Iraq Veteran, Now a West Point Professor, Seeks to Rein In Disability Pay". New York Times. Retrieved 20 June 2015.
- "Disability Compensation: Eligibility". Department of Veterans Affairs. Retrieved 30 November 2012.
- Moering, Robert (2011). "Military service records: Searching for the truth" (PDF). Psychological Injury and Law. 4 (3–4): 217–34. doi:10.1007/s12207-011-9114-3.
- "Code of Federal Regulations (CFR), Title 38, Chapter I, Part 3, Subpart A, Subjgrp-General(Part 3), Section 3.6 – Duty periods" (PDF). U.S. Government Printing Office, Code of Federal Regulations (CFR). Retrieved 30 November 2012.
- "Disability Compensation". Veterans Benefits Administration. U.S. Department of Veterans Affairs. Retrieved 24 August 2015.
Disability compensation is a monthly tax-free benefit paid to Veterans who are at least 10% disabled because of injuries or diseases that were incurred in or aggravated during active duty, active duty for training, or inactive duty training.
- "Code of Federal Regulations, Title 38, Chapter I, Part 3, Subpart A, Subjgrp-General(Part 3), Section 3.1 – Definitions – (m) In line of duty" (PDF). U.S. Government Printing Office, Code of Federal Regulations (CFR). Retrieved 30 November 2012.
- The PTSD Compensation and Pension Examination. Institute of Medicine. National Academies Press. Retrieved 20 October 2012.
- Worthen, Mark; Moering, Robert (December 2011). "A practical guide to conducting VA compensation and pension exams for PTSD and other mental disorders" (PDF). Psychological Injury and Law. 4 (3–4): 187–216. doi:10.1007/s12207-011-9115-2. Retrieved 19 May 2013.
- "Claims Process – Compensation". Department of Veterans Affairs. Retrieved 21 September 2013.
- "Veterans Service Representative". MyCareer@VA. Department of Veterans Affairs. Retrieved 21 September 2013.
- "Veterans Claims Assistance Act of 2000" (PDF). Public Law 106-475. Nov. 9, 2000. Government Printing Office.
- The VA Medical Examination And Disability Rating Process: Hearing before the Subcomm. Disability Assistance & Memorial Aff. of the H. Comm. Veterans Aff., 110th Congress 63-65 (2008) (statement of Michael McGeary, Senior Program Officer & Study Dir., Comm. Med. Evaluation Veterans Disability Benefits, Bd. Mil. & Veterans Health, Inst. of Med., Nat'l Acad.) ("Applicants for disability compensation are asked to provide their medical records and, under the duty-to-assist law, VBA helps them obtain those records, especially their service medical records. In nearly every case, VBA has applicants undergo a compensation and pension, or C&P, examination performed by a Veterans Health Administration (VHA) or contractor clinician.")
- Veterans Benefits Administration (VBA) (December 2016). "Your VA Claim Exam: Know What's Next (Claim Exam Fact Sheet)" (PDF). www.VA.gov. Retrieved 11 October 2017.
The VA claim exam, also called a C&P exam, is different from a regular medical appointment because the examiner won't prescribe any medicine or treat you for your disability. This exam occurs only if you file a compensation or pension claim.
- "Ratings Veterans Service Representative". MyCareer@VA. Department of Veterans Affairs. Retrieved 21 September 2013.
- "Schedule of ratings – mental disorders" (DOC). 38 C.F.R. §4.130. Department of Veterans Affairs. Note: The General Rating Formula for Mental Disorders appears immediately under 9440 Chronic adjustment disorder on the third page. This placement is misleading because it appears as if the Rating Formula applies to Chronic Adjustment Disorder only, which is not the case. The Rating Formula applies to all mental disorders. Retrieved 28 December 2013.
- "How to file a VA disability claim". U.S. Department of Veterans Affairs. 2019-10-01. Retrieved 2019-10-03.
- Office of the Secretary, Dep't Veterans Aff., Veterans and Military Service Organizations and State Directors of Veterans Affairs: 2019 Directory.
- asknod (2012). Veterans Administration Claims: What You Need to Know to Be Successful. ISBN 978-1-4771-3951-6.
- "How To Win Your Claim". VAWatchdog dot org. VA Watchdog (Jim Strickland). Retrieved 28 April 2014.
- Veterans' Judicial Review Act, P.L. 100–687, 102 Stat. 4105, 100th Cong. (Nov. 18, 1988) (codified as amended at 38 U.S.C. §§ 7251–7299).
- "38 C.F.R. 14.636 – Payment of fees for representation by agents and attorneys in proceedings before Agencies of Original Jurisdiction and before the Board of Veterans' Appeals". Code of Federal Regulations. United States Government Printing Office (GPO). Retrieved 30 April 2013.
- "Veterans Compensation Benefits Rate Tables". Veterans Benefits Administration. Department of Veterans Affairs. Retrieved 28 December 2013.
- "Schedule of ratings – mental disorders". Code of Federal Regulations, Title 38: Pensions, Bonuses, and Veterans' Relief, Part 4 – Schedule for Rating Disabilities, Subpart B – Disability Ratings, Mental Disorders. Government Printing Office, Electronic Code of Federal Regulations (e-CFR). Note: Scroll down about one page to find the General Rating Formula for Mental Disorders – it appears immediately under 9440 Chronic adjustment disorder. This placement is misleading because it appears as if the Rating Formula applies to Chronic Adjustment Disorder only, which is not the case. The Rating Formula applies to all mental disorders. Retrieved 28 December 2013.
- Simonson, Scott (2008). "Back from war – A battle for benefits: Reforming VA's disability ratings system for veterans with post-traumatic stress disorder" (PDF). Arizona Law Review. 50: 1177–1204. Retrieved 10 June 2014.
- Wilson, John. "Statement of John L. Wilson, Assistant National Legislative Director, Disabled American Veterans at the Hearing of the Subcommittee on Disability Assistance and Memorial Affairs, House Veterans Affairs Committee, on the Implementation and Status Update on the Veterans' Benefits Improvement Act, P.L. 110-389, on 3 February 2010". archives.democrats.veterans.house.gov. U.S. House of Representatives. Retrieved 10 June 2014.
- Huang, Daniel (11 May 2015). "Automated System Often Unjustly Boosts Veterans' Disability Benefits: Reduction of VA staff input allows more patients to exaggerate symptoms" (12 May 2015 [print edition]). Wall Street Journal. p. A6. Retrieved 13 May 2015.
An effort by the Department of Veterans Affairs that aimed to speed the processing of disability-benefits applications also loosened controls that prevent veterans from exaggerating symptoms to receive more money, say current and former VA employees. A software system introduced in 2012 that automates veterans' disability levels for compensation relies almost solely on a patient's self-reported ailments, the employees say, even in the face of contradictory information. While the new system reduced paperwork and increased output, it limited the information that the VA's employees who determine compensation eligibility and dollar amounts—called raters—can consider, according to these employees. The result, raters contend: a more inaccurate process that approves higher levels of disability than veterans' military records, medical histories and other evidence might show—in some cases increasing payments to veterans by thousands of dollars a month. The process, they maintain, also ignores stated VA rules in which claims must be evaluated 'in light of the [veteran's] whole recorded history.' Senior VA officials counter that the software system still relies on raters' expertise to determine the accuracy of claims. They say it is designed to facilitate, but not replace, that process. Raters 'have every right to change [the symptoms] if there is other evidence in the file,' one official said.
- Office, U. S. Government Accountability (10 September 2012). "VA Disability Compensation: Actions Needed to Address Hurdles Facing Program Modernization (GAO-12-846)" (GAO-12–846). United States Government Accountability Office. Retrieved 5 August 2014. Cite journal requires
|journal=(help) - See Definitions, Initial claim, claim for increase, 38 C.F.R. § 3.1(p)(1)(ii). See also Veterans Benefits Admin., Adjudication Proc. Manual, Identification of Claims for Increase, M21-1, pt. III, subpt. ii, chap. 2, sec. E, subsec. 1.
- Total disability ratings for compensation based on unemployability of the individual, 38 CFR § 4.16 (2018), https://www.law.cornell.edu/cfr/text/38/4.16
- "Veteran's Application for Increased Compensation Based on Unemployability (VA Form 21-8940)" (PDF). Veterans Benefits Administration (PDF). Department of Veterans Affairs. Retrieved 15 August 2019.
- Total and permanent total ratings and unemployability, 38 C.F.R. § 3.340 (2018), https://www.law.cornell.edu/cfr/text/38/3.340
- Veterans Benefits Admin., Adjudication Proc. Manual, Compensation Based on Individual Unemployability (IU), M21-1, pt. IV, subpt. ii, chap. 2, sec. F (8 July 2019), accessed on 18 August 2019.
- Functional Organizational Manual (PDF). 3.1. Washington, DC: Department of Veterans Affairs. 2016. pp. 238–240.
The Office of Disability and Medical Assessment (DMA) (10NC8) provides executive leadership to VHA's disability programs worldwide, including both the traditional Compensation and Pension (C&P) and the Integrated Disability Evaluation System (IDES) programs.
- "Certification of Clinicians Performing VA Disability Evalutions [sic] (VHA Directive 1603)" (PDF). VHA Publications. Department of Veterans Affairs, Veterans Health Administration. 22 April 2013. Retrieved 23 August 2014.
- Murphy, Thomas (25 June 2014). "Witness Testimony of Mr. Thomas Murphy, Director, Compensation Service, Veterans Benefits Administration, U.S. Department of Veterans Affairs". VBA and VHA Interactions: Ordering and Conducting Medical Examinations: U.S. House of Representatives, Committee on Veterans Affairs. Retrieved 23 August 2014.
VHA supplements these C&P clinics' capabilities, as necessary, using contracted disability examination services. These contractors support the performance of required disability examinations during surges in claims processing, for periods of staffing vacancies, or for times when specialists are required. VHA may also use these services for Veterans who do not live near a VHA medical facility. The use of these "on demand" services allows VHA to maintain examination timeliness and quality to support VA's goals for processing disability claims. VHA medical facilities can use locally contracted services through an individual facility or utilize the centralized, national VHA Disability Examination Management (DEM) contract. ... In addition to examinations completed by VHA, VBA contracts with three vendors to conduct C&P examinations.
- Advisory Committee on Disability Compensation, Department of Veterans Affairs, June 20–21 Meeting Minutes (p. 4) (2017). https://www.va.gov/ADVISORY/docs/Minutes-ACDCJun2017.pdf
- "LHI: Care for Mission Critical". logisticshealth.com. Retrieved 2018-01-04.
- "Veterans Evaluation Services". Retrieved 23 August 2014.
- "VA—MDE|VetFed". www.vetfed.com. Retrieved October 12, 2017.
- "QTC - Quality, Timeliness, Customer Service". QTCM.com. QTC, A Lockheed-Martin Company. Retrieved 23 August 2014.
- "QTC". www.magellanprovider.com. Retrieved 2018-01-04.
QTC has chosen Magellan to maintain a network of providers offering Compensation and Pension (C&P) examinations to veterans and service members.
- "Review Post Traumatic Stress Disorder (PTSD) Disability Benefits Questionnaire (VA Form 21-0960P-3)" (PDF). Veterans Health Administration. October 2012. Retrieved 24 August 2014.
The following health care providers can perform REVIEW examinations for PTSD: a board-certified or board-eligible psychiatrist; a licensed doctorate-level psychologist; a doctorate-level mental health provider under the close supervision of a board-certified or board-eligible psychiatrist or licensed doctorate-level psychologist; a psychiatry resident under close supervision of a board-certified or board-eligible psychiatrist or licensed doctorate-level psychologist; a clinical or counseling psychologist completing a one-year internship or residency (for purposes of a doctorate-level degree) under close supervision of a board-certified or board-eligible psychiatrist or licensed doctorate-level psychologist; or a licensed clinical social worker (LCSW), a nurse practitioner, a clinical nurse specialist, or a physician assistant, under close supervision of a board-certified or board-eligible psychiatrist or licensed doctorate-level psychologist.
- Institute of Medicine and National Research Council (8 May 2007). PTSD Compensation and Military service. National Academies Press. pp. 204–05. Retrieved 16 November 2014.
- Russo, Arthur (5 Mar 2014). "Assessing veteran symptom validity" (PDF). Psychological Injury and Law. 7 (2): 178–90. doi:10.1007/s12207-014-9190-2. Retrieved 16 November 2014.
- Sparr, L. F.; White, R.; Friedman, M. J.; Wiles, D. B. (1994). "Veterans' psychiatric benefits: enter courts and attorneys". The Bulletin of the American Academy of Psychiatry and the Law. 22 (2): 205–222. ISSN 0091-634X. PMID 7949410.
Among regional offices, there has been considerable variability in adjudicating claims. For example from 1986 to 1990, the PTSD claim approval rate in 58 VA regional offices varied from 36.2 percent to 73.5 percent.
- Murdoch, Maureen; Hodges, James; Cowper, Diane; Sayer, Nina (February 2005). "Regional variation and other correlates of Department of Veterans Affairs Disability Awards for patients with posttraumatic stress disorder". Medical Care. 43 (2): 112–121. doi:10.1097/00005650-200502000-00004. ISSN 0025-7079. PMID 15655424.
... rates of PTSD service connection varied almost twofold across regions between 1994 and 1998. Consistent with earlier research, this variation could not be explained by regional dissimilarities in veterans' sociodemographic or military characteristics, rates of major medical comorbidity, or combat-injury status. We extend these findings to show that the regional variation in PTSD disability awards likewise could not be attributed to regional differences in veterans' current PTSD symptom severity or level of disability.
- Watson, P.; McFall, M.; McBrine, C.; Schnurr, P. P.; Friedman, M. J.; Keane, T.; Hamblen, J. L. (2002). Best Practice Manual for Posttraumatic Stress Disorder (PTSD) Compensation and Pension Examinations (PDF). Department of Veterans Affairs. Retrieved 13 May 2015.
This document provides information on Posttraumatic Stress Disorder and current recommendations regarding what is known about "best practice" procedures for assessing PTSD among veteran populations.
- Jackson, J. C.; et al. (October 2011). "Variation in practices and attitudes of clinicians assessing PTSD-related disability among veterans". Journal of Traumatic Stress. 24 (5): 609–13. doi:10.1002/jts.20688. PMID 21913226.
- "Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)". PTSD: For Professionals. National Center for PTSD. Retrieved 16 November 2014.
The CAPS is the gold standard in PTSD assessment.
- Speroff, T.; et al. (December 2012). "Impact of evidence-based standardized assessment on the disability clinical interview for diagnosis of service-connected PTSD: A cluster-randomized trial". Journal of Traumatic Stress. 25 (6): 607–15. doi:10.1002/jts.21759. PMID 23225029.
The findings of this study show that administering a standardized disability assessment resulted in more complete coverage of functional impairment and PTSD symptoms. Standardized assessment elicited an increase in relevant information and nearly eliminated variation between examiners and medical centers. Furthermore, this study found that standardized assessment substantially diminished the uncertainty in diagnosis, and increased concordance of diagnosis ...
- O'Toole, Marie T., ed. (2013). Mosby's Medical Dictionary (Kindle edition) (9th ed.). St. Louis, MO: Elsevier Health Sciences. Kindle Locations 77966-77971. ISBN 978-0-323-08541-0.
false negative - an incorrect result of a diagnostic test or procedure that falsely indicates the absence of a finding, condition, or disease. The rate of occurrence of false-negative results varies with the diagnostic accuracy and specificity of the test or procedure. As the accuracy and specificity of a test increase, the rate of false-negatives decreases. Certain tests are known to yield false negative results at a certain rate; in all tests a small number will occur by chance alone.
- Colman, Andrew M. (2015). "False positive". A Dictionary of Psychology (4th ed.). Oxford University Press. doi:10.1093/acref/9780199657681.001.0001. ISBN 9780199657681.
false positive, n. - An incorrect classification of an element as a member of a class to which it does not in fact belong, as when a decision procedure results in a person being wrongly diagnosed as having a disorder.
- Marx, Brian P.; Engel-Rebitzer, Eden; Bovin, Michelle J.; Parker-Guilbert, Kelly S.; Moshier, Samantha; Barretto, Kenneth; Szafranski, Derek; Gallagher, Matthew W.; Holowka, Darren W. (2017). "The influence of veteran race and psychometric testing on veterans affairs posttraumatic stress disorder (PTSD) disability exam outcomes". Psychological Assessment. 29 (6): 710–719. doi:10.1037/pas0000378. PMID 28594214.
... among veterans diagnosed with PTSD by an independent evaluator, Black veterans were significantly less likely than White veterans to receive both a C&P PTSD diagnosis and to be given PTSD service connection status. Further, among veterans not meeting diagnostic criteria for SCID PTSD, Black veterans tended to be more likely than White veterans to be denied both C&P PTSD status and PTSD service connection status.
- Murdoch, Maureen; Hodges, James; Cowper, Diane; Fortier, Larry; van Ryn, Michelle (April 2003). "Racial disparities in VA service connection for posttraumatic stress disorder disability". Medical Care. 41 (4): 536–549. doi:10.1097/01.MLR.0000053232.67079.A5. ISSN 0025-7079. PMID 12665717.
After adjusting for respondents' sociodemographic characteristics, symptom severity, functional status, and trauma histories, black persons' rate of service connection for PTSD was 43% compared with 56% for other respondents (P = 0.003).
- Rosen, Marc I.; Afshartous, David; Nwosu, Sam; Scott, Melanie C.; Jackson, James C.; Marx, Brian; Murdoch, Maureen; Sinnot, Patrica L.; Speroff, Theodore (2013-04-01). "Racial Differences in Veterans' Satisfaction With Examination of Disability From Posttraumatic Stress Disorder". Psychiatric Services. 64 (4): 354–359. doi:10.1176/appi.ps.201100526. ISSN 1075-2730. PMC 3677046. PMID 23318842.
- Wandler, Hillary A. (Spring 2013). "The Role of Culture in Advocating for Accurate Diagnosis and Rating of Veterans' Psychological Disabilities". Mental Health Law & Policy Journal. 2: 18.
The real potential for injustice comes when patient's whose culture's heavily influence the way they communicate distress meet clinicians who use a universalist or one-size-fits-all approach to assessment and diagnosis. As a patient may report symptoms differently across cultures, a clinician may interpret what the patient reports differently depending on the clinician's approach to assessment and diagnosis. The effect is even more significant when the patient and the clinician are from different cultures.
- Poyner, G. (27 May 2010). "Psychological evaluations of veterans claiming PTSD disability with the Department of Veterans Affairs: A clinician's viewpoint". Psychological Injury and Law. 3 (2): 130–32. doi:10.1007/s12207-010-9076-x.
- McMath, William (April 11, 2015). "Being Veteran-Centric". My Education at the VA: C&P Exams and PTSD. Retrieved December 20, 2017.
... the psychology supervisor at my facility refused to order psychological tests with titles containing the word 'malingering,' and patients who were obviously lying or faking were excused by the mantra 'veterans--even when they have PTSD--feel like they have to exaggerate just to be believed.'
- Arbisi, P. A.; Murdoch, M.; Fortier, L.; McNulty, J. (2004). "MMPI-2 validity and award of service connection for PTSD during the VA compensation and pension evaluation". Psychological Services. 1 (1): 56–67. doi:10.1037/1541-1559.1.1.56.
- Freeman, T.; Powell, M.; Kimbrell, T. (15 April 2008). "Measuring symptom exaggeration in veterans with chronic posttraumatic stress disorder". Psychiatry Research. 158 (3): 374–80. doi:10.1016/j.psychres.2007.04.002. PMID 18294699.
- Frueh, B. C.; Hamner, M. B.; Cahill, S. P.; Gold, P. B.; Hamlin, K. L. (October 2000). "Apparent symptom overreporting in combat veterans". Clinical Psychology Review. 20 (7): 853–85. doi:10.1016/S0272-7358(99)00015-X. PMID 11057375.
- Hall, R. C. W.; Hall, R. C. W. (December 2006). "Malingering of PTSD: forensic and diagnostic considerations, characteristics of malingerers and clinical presentations". General Hospital Psychiatry. 28 (6): 525–35. doi:10.1016/j.genhosppsych.2006.08.011. PMID 17088169.
- Gold, P. B.; Frueh, B. C. (November 1999). "Compensation-seeking and extreme exaggeration of psychopathology among combat veterans evaluated for posttraumatic stress disorder". The Journal of Nervous and Mental Disease. 187 (11): 680–84. doi:10.1097/00005053-199911000-00005. PMID 10579596.
- Wisdom, N. M.; et al. (2014). "PTSD and cognitive functioning: Importance of including performance validity testing". The Clinical Neuropsychologist. 28 (1): 128–45. doi:10.1080/13854046.2013.863977. PMID 24354897.
- Marx, Brian P.; Bovin, Michelle J.; Szafranski, Derek D.; Engel-Rebitzer, Eden; Gallagher, Matthew W.; Holowka, Darren W.; Schnurr, Paula P.; Rosen, Raymond C.; Keane, Terence M. (2016-01-19). "Validity of Posttraumatic Stress Disorder Service Connection Status in Veterans Affairs Electronic Records of Iraq and Afghanistan Veterans". The Journal of Clinical Psychiatry. 77 (4): 517–522. doi:10.4088/jcp.14m09666. ISSN 0160-6689. PMID 26797388.
This study examined the extent to which veterans' posttraumatic stress disorder (PTSD) service connection (SC) status corresponded to their PTSD diagnostic status, as determined by a semistructured diagnostic interview. ... For current PTSD, results showed a slightly higher proportion of false positives—individuals who did not meet SCID criteria but who did have SC for PTSD—than false negatives—individuals who met SCID criteria but did not have SC for PTSD. For lifetime PTSD, the proportion of false negatives was approximately twice the proportion of false positives. ... PTSD diagnostic and SC status are discordant for a significant minority of veterans.
- The VA Medical Examination And Disability Rating Process: Hearing before the Subcomm. Disability Assistance & Memorial Aff. of the H. Comm. Veterans Aff., 110th Congress 63-65 (2008) (statement of Michael McGeary, Senior Program Officer & Study Dir., Comm. Med. Evaluation Veterans Disability Benefits, Bd. Mil. & Veterans Health, Inst. of Med., Nat'l Acad.)(GPO Serial No. 110–70) ("Applicants for disability compensation are asked to provide their medical records and, under the duty-to-assist law, VBA helps them obtain those records, especially their service medical records. In nearly every case, VBA has applicants undergo a compensation and pension, or C&P, examination performed by a Veterans Health Administration (VHA) or contractor clinician.")
- U.S. Dep't Veterans Aff., Off. Inspector Gen., Review of Compensation and Pension Medical Examination Services, Rep. No. 7R1-A02-114 (1997) ("Disability benefit payments are based, in part, on interpretations of medical evidence by the Veterans Benefits Administration (VBA) disability rating specialists. That evidence is developed by physicians employed or supervised by the Veterans Health Administration (VHA), in the form of compensation and pension (C&P) examinations. ... VBA cannot complete payment action on veterans' disability claims until examination results are received.")
- Washington v. Nicholson, 21 Vet. App. 191, 197 (2007) (Hagel, J., concurring) ("Because of the immense importance of medical evidence in the VA claims process," [medical examinations and opinions] "can bear significantly upon the outcome of the claim for VA benefits.")
- Mathis v. McDonald, 834 F. 3d 1347, 1353, (Fed. Cir. 2016) (Reyna, J., dissenting from denial of rehearing en banc) ("VA regional offices use the opinions prepared by examiners in determining whether to award a veteran disability benefits. The decision whether to award benefits often turns on whether the disability is shown to be connected to the veteran's military service. ... In other words, as in this case, the service connection issue is often dispositive.")
- U.S. Government Accountability Office, Military sexual trauma: Improvements made, but VA can do more to track and improve the consistency of disability claim decisions (p. 18) (2014) (GAO-14-447) ("VBA adjudicators generally rely on examiners' assessments when deciding whether to approve a claim ...").
- Zarembo, Alan (3 August 2014). "As disability awards grow, so do concerns with veracity of PTSD claims". Los Angeles Times. Retrieved 19 November 2014.
Even some veterans whose diagnosis falls under deep suspicion have managed to keep their disability ratings. In one case that Moering reviewed in 2009, he searched military records and concluded that a Navy veteran on the disability rolls for PTSD had lied to VA clinicians about having served in the elite SEALs and concocted his combat history. The VA responded by reducing his PTSD rating from 50% to 30%, records show.
- Huang, Daniel (27 October 2014). "VA Disability Claims Soar: Some See Higher Fraud Risk as More Vets Seek Compensation, Overloading Doctors". The Wall Street Journal. Dow Jones & Company. Retrieved 19 November 2014.
Requests for disability pay by veterans have ballooned during the past five years, overloading many doctors who evaluate the claims and increasing the possibility of fraud, according to current and former VA staff and government watchdogs.
- McVay, Mark (21 June 2014). "When PTSD benefits are abused". Denver Post. Retrieved 20 June 2015.
I ran into John a few years back for the first time since the early 1970s when we both returned to Michigan from Vietnam. But John was clearly excited to see me. 'Hey man,' he said, 'have you applied for PTSD benefits yet? You can get a couple thousand a month. All you have to do is go to this counseling program for two weeks. Nothing to it. You ought to go.'
- Harbaugh, Ken (1 June 2015). "The Risk of Over-Thanking Our Veterans". New York Times. Retrieved 20 June 2015.
And while most vets who receive disability checks deserve them, one of the worst kept secrets among those seeking a disability rating is that the system can be beaten. Claim the right combination of symptoms, whether you are suffering or not, and there is a decent chance you can get a monthly disability check, tax free, for the rest of your life. There are even blogs out there to walk you through the process of claiming an injury that cannot be disproved.
- Hernandez, Christopher (10 February 2014). "PTSD: Fakers and frauds and WTAF?". Breach Bang Clear. Retrieved 13 October 2017.
I think all of us combat veterans of Iraq and Afghanistan know of someone faking PTSD for free money. ... As with any form of welfare, people are going to jump on it if it's easy money. If we make it so simple to get diagnosed as "disabled" by PTSD, we shouldn't be surprised that so many people get diagnosed.
- Hernandez, Christopher (26 February 2014). "PTSD, Reading Comprehension and the Great American Love of Victimhood". Breach Bang Clear. Retrieved 13 October 2017.
I'm proud as hell of being a veteran. I'm proud of the men and women I served with. ¶ I didn't join the military so that my country could give me a free ride for the rest of my life, I joined to defend it from its worst enemies. I expected pain, fear and hardship from war. I believe our job as soldiers is to endure that pain, fear and hardship so our citizens don't have to. We are the barrier between our people and foreign threats. ¶ Being part of that barrier doesn't require heroism. But it does require integrity, courage and strength. The same integrity, courage and strength my great uncle Leo undoubtedly showed before he marched to his death on Bataan, and my great uncle Jesse showed when he jumped into Sicily, Normandy and Holland, and my great uncle Richard showed as he fought his way through Korea. And by generations of other American warriors on battlegrounds from Lexington to the Korengal Valley. ¶ Every time a veteran makes a false claim of PTSD, that barrier is weakened. Every time a veteran is exposed as a fraud, the barrier loses precious integrity. Every story that hints we're all damaged by PTSD, that we're all unstable, that we're all victims, gouges chunks from the barrier's foundation.
- Hernandez, Christopher (21 February 2016). "Thieves and Liars: PTSD Fakers and the VA". Breach Bang Clear. Retrieved 13 October 2017.
John [the VA-employed C&P psychologist] can't give specifics, but two Army veterans who served during a particular war told stories of being traumatized by their experiences at a notorious attack. However, the attack they claimed to have witnessed happened years after their war and discharge, and involved a different service. 'I told one of those veterans he couldn't have been there, because his DD-214 showed he wasn't even in the military when it happened. He stopped talking, glared at me, grabbed his DD-214 and walked out.' ¶ So he was kicked out of the VA for malingering, right? Of course not. 'In my notes I wrote that the veteran was clearly malingering, and could not have been at his claimed qualifying event,' John said. 'But the evaluator either didn't bother to read my notes, or wanted to be nice to the veteran. So he's on 100% disability for PTSD, even after I caught him making up trauma.'
- Overcoming PTSD: Assessing VA's Efforts to Promote Wellness and Healing, H. Comm. Veterans Affairs, 115th Cong. (2017) (statement of Brendan O'Byrne, Veteran, United States Army) ("[During group psychotherapy sessions] I heard stories that sounded a lot like a bad day rather than a traumatic moment. As weeks went by, I realized the sad truth about a portion of the veterans there, they were scammers, seeking a higher rating without a real trauma. This was proven when I overheard one vet say to another that he had to 'pay the bills' and how he 'was hoping this in-patient was enough for a 100% rating'. I vowed never to participate in group counseling through the VA again. ... The trend I have seen among the combat veterans, the most traumatized group, [is to] stay away from the VA, or at the very least, [stay away from] the group counseling settings. They have no patience for the fraudulent veterans scamming the system to get a pay check and they are definitely not going to open up about their worst days to those who know nothing about them.")
- "Disability Benefits Questionnaire". Veterans Health Administration. Retrieved 24 August 2014.
- "VA Claims Process: Review of VA's Transformation Efforts" (PDF). U.S. Senate Committee on Veterans Affairs. 13 March 2013. p. 12. Retrieved 24 August 2014.
DBQs replace traditional VA examination reports and are designed to capture all the needed medical information relevant to a specific condition at once and up front so that claims can be developed and processed in a more timely and accurate manner, with the end result being faster service for Veterans. DBQs change the way medical evidence is collected, giving Veterans the option of having their private physician complete a DBQ that provides the medical information needed to rate their claims—minimizing the need for a VA exam which adds additional time to the claim development process. Information in the DBQs maps to the VA Schedule for Rating Disabilities, and provides all of the necessary information to decide a disability claim.
- "Documentation of Medical Evidence for Disability Evaluation Purposes (VHA Directive 2013-002)" (PDF). 4(e)(1)(c): Veterans Health Administration. January 14, 2013. p. 4. Retrieved 24 August 2014.
For mental health disability examination requests, it is recommended that the Veteran's treating provider not complete the disability examination to maintain the integrity of the patient-provider relationship.
- Worthen, M. D.; Moering, R. G. (December 2011). "A Practical Guide to Conducting VA Compensation and Pension Exams for PTSD and Other Mental Disorders" (PDF). Psychological Injury and Law. 4 (3–4): 193. doi:10.1007/s12207-011-9115-2.
... we strongly recommend not completing a DBQ for a veteran the private practitioner is seeing for psychotherapy or psychiatric treatment as it will create the awkward position of a dual role relationship with the patient, viz., psychologist or doctor and independent evaluator ...
- Strasburger, L. G.; Gutheil, T. G.; Brodsky, A. (1 April 1997). "On wearing two hats: Role conflict in serving as both psychotherapist and expert witness" (PDF). The American Journal of Psychiatry. 154 (4): 448–56. doi:10.1176/ajp.154.4.448. PMID 9090330. Retrieved 24 August 2014.
The process of psychotherapy is a search for meaning more than for facts. In other words, it may be conceived of more as a search for narrative truth (a term now in common use) than for historical truth. Whereas the forensic examiner is skeptical, questioning even plausible assertions for purposes of evaluation, the therapist may be deliberately credulous, provisionally 'believing' even implausible assertions for therapeutic purposes. The therapist accepts the patient's narrative as representing an inner, personal reality, albeit colored by biases and misperceptions. This narrative is not expected to be a veridical history; rather, the therapist strives to see the world 'through the patient's eyes.' [citation footnote numbers omitted]
- Greenberg, S. A.; Shuman, D. W. (1997). "Irreconcilable conflict between therapeutic and forensic roles" (PDF). Professional Psychology: Research and Practice. 28 (1): 50–57. CiteSeerX 10.1.1.454.652. doi:10.1037/0735-7028.28.1.50.
The therapist is a care provider and usually supportive, accepting, and empathic; the forensic evaluator is an assessor and usually neutral, objective, and detached as to the forensic issues. A forensic evaluator's task is to gain an empathic understanding of the person but to remain dispassionate as to the psycholegal issues being evaluated. For therapists, empathy and sympathy–generating a desire to help–usually go hand-in-hand. For forensic evaluators, the task is a dispassionate assessment of the psycholegal issues.
- "Review Post Traumatic Stress Disorder (PTSD) Disability Benefits Questionnaire (VA Form 21-0960P-3, OCT 2012)" (PDF). VBA Forms. Department of Veterans Affairs. Retrieved 13 May 2015.
- "Mental Disorders (Other Than PTSD and Eating Disorders) Disability Benefits Questionnaire (VA Form 21-0960P-3, Oct 2012)" (PDF). VBA Forms. Department of Veterans Affairs. Retrieved 13 May 2015.
- Worthen, M. D.; Moering, R. G. (December 2011). "A Practical Guide to Conducting VA Compensation and Pension Exams for PTSD and Other Mental Disorders" (PDF). Psychological Injury and Law. 4 (3–4): 192. doi:10.1007/s12207-011-9115-2.
One section of every mental health-related DBQ is a symptom checklist where, for example, examiners are asked to check off a box if a veteran has "depressed mood" or "anxiety." Unfortunately, the DBQ does not provide any guidance with regard to how one determines the level of symptom frequency, severity, or duration required to endorse a given symptom. Thus, for example, if a veteran reports that she feels "a little depressed" once or twice a week, it is not clear if the examiner should check off the "depressed mood" box or not.
- Russo, A. C. (March 2013). "Ethical, Legal and Risk Management Considerations in the Neuropsychological Assessment of Veterans". Psychological Injury and Law. 6 (1): 21–30. doi:10.1007/s12207-013-9145-z.
VHA neuropsychologists performing VBA C&P examinations [should be] aware of the limitations of the DEMO training modules and the Disability Benefit Questionnaires (DBQ) as used for VBA C&P examination report templates.
- Huang, Daniel (11 May 2015). "Automated System Often Unjustly Boosts Veterans' Disability Benefits". Wall Street Journal. Dow Jones & Company. Retrieved 24 August 2015.
A software system introduced in 2012 that automates veterans' disability levels for compensation relies almost solely on a patient's self-reported ailments, the employees say, even in the face of contradictory information. While the new system reduced paperwork and increased output, it limited the information that the VA's employees who determine compensation eligibility and dollar amounts—called raters—can consider, according to these employees.
External links
U.S. Department of Veterans Affairs
- Federal Benefits for Veterans, Dependents, & Survivors
- Apply for Benefits Online
- VA Benefits in Brief
- Compensation and Pension Service
- VA Healthcare Benefits Overview - Updated annually; print (PDF) & online versions.
- Veterans Health Benefits Handbook - Registration required (available to veterans & family members only).
- Online VA Healthcare Eligibility Check
- Directory of Veterans Service Organizations - Provided by the United States Department of Veterans Affairs.
U.S. government resources
- Information for Active Duty Service Personnel
- Information for National Guard & Reservists
- U.S. Department of Veterans Affairs Resource Locator - Search engine specific to VA services.
- National Resource Directory (NRD) - The NRD is a partnership among the U.S. Department of Defense, Department of Labor, and Department of Veterans Affairs. The NRD.gov website connects wounded warriors, service members, veterans, their families, and caregivers to programs and services that support them.
VA treatment resources
- Learn about PTSD - "Learn more about PTSD, treatment options, self-help tools, and resources to help you recover."
- Where to get help for PTSD
- Understanding PTSD
- PTSD Treatment Programs in the US Department of Veterans Affairs
- My HealtheVet: The Gateway to Veteran Health and Wellness
- Military Sexual Trauma Resources Provided by the VA