Attention deficit hyperactivity disorder management
Attention deficit hyperactivity disorder management options are evidence-based practices with established treatment efficacy for ADHD. The American Academy of Pediatrics recommends different treatment paradigms depending on the age of the person being treated. For those aged 4–5, the Academy recommends evidence-based parent- and/or teacher-administered behavior therapy, with the addition of methylphenidate only if there is continuing moderate-to-severe functional disturbances. For those aged 6–11, the use of medication in combination with behavior therapy is recommended, with the evidence for stimulant medications being stronger than that for other classes. For those aged 12–18, medication should be prescribed with the consent of the treated adolescent, preferably in combination with behavioral therapy. The evidence for the utility of behavioral interventions in this aged group was rated only "C" quality, however.[1]
There are a number of stimulant and non-stimulant medications indicated for the treatment of ADHD. The most commonly used stimulant medications include methylphenidate (Ritalin, Concerta), mixed amphetamine salts (Adderall, Mydayis), dextroamphetamine (Dexedrine), and lisdexamfetamine (Vyvanse). Non-stimulant medications with a specific indication for ADHD include atomoxetine (Strattera), guanfacine (Intuniv), and clonidine (Kapvay). Other medicines which may be prescribed off-label include bupropion (Wellbutrin), tricyclic antidepressants, SNRIs, or MAOIs.[2][3][4] The presence of comorbid (co-occurring) disorders can make finding the right treatment and diagnosis much more complicated, costly, and time-consuming. So it is recommended to assess and simultaneously treat any comorbid disorders.[5]
A variety of psychotherapeutic and behavior modification approaches to managing ADHD including psychotherapy and working memory training may be used. Improving the surrounding home and school environment with parent management training and classroom management can improve the behavior of children with ADHD.[6] Specialized ADHD coaches provide services and strategies to improve functioning, like time management or organizational suggestions. Self-control training programs have been shown to have limited effectiveness.
As of 2006 there was a shortage of data regarding ADHD drugs' potential adverse effects,[7] with very few studies assessing the safety or efficacy of treatments beyond four months,[8] and no randomized controlled trials assessing for periods of usage longer than two years.[9][10]
Psychosocial
There are a variety of psychotherapeutic approaches employed by psychologists and psychiatrists; the one used depends on the patient and the patient's symptoms. The approaches include psychotherapy, cognitive-behavior therapy, support groups, parent training, meditation, and social skills training.
Parents and classroom
Improving the surrounding home and school environment can improve the behavior of children with ADHD.[6] Parents of children with ADHD often show similar deficits themselves, and thus may not be able to sufficiently help the child with his or her difficulties.[11] Improving the parents' understanding of the child's behavior and teaching them strategies to improve functioning and communication and discourage unwanted behavior has measurable effect on the children with ADHD.[6] The different educational interventions for the parents are jointly called Parent Management Training. Techniques include operant conditioning: a consistent application of rewards for meeting goals and good behavior (positive reinforcement) and punishments such as time-outs or revocation of privileges for failing to meet goals or poor behavior.[6] Classroom management is similar to parent management training; educators learn about ADHD and techniques to improve behavior applied to a classroom setting. Strategies utilized include increased structuring of classroom activities, daily feedback, and token economy.[6] In order for Token Economy to benefit students with ADHD, all staff must be consistent in rewarding the same behaviors. Additionally, establishing classroom routines will help to ensure that students with ADHD remain focused throughout the day.
Cognitive training
A 2013 paper published by two researchers from the University of Oslo concluded that working memory training provides short term improvements, but that there was limited evidence that these improvements were sustained or that they were generalized to improved verbal ability, mathematical skills, attention, or word decoding.[12] A 2014 paper published by a group of researchers from the University of Southampton presented the result of meta analysis study of 14 recently published randomized controlled trials (RCTs). The authors concluded that "more evidence from well-blinded studies is required before cognitive training can be supported as a frontline treatment of core ADHD symptoms".[13]
Medications
Stimulants
Stimulants are the most commonly prescribed medications for ADHD. The stimulant medications indicated to treat ADHD are methylphenidate (Ritalin, Concerta), dexmethylphenidate (Focalin), mixed amphetamine salts (Adderall),[14] dextroamphetamine (Dexedrine), lisdexamfetamine (Vyvanse),[15] and in rare cases methamphetamine (Desoxyn).[16] Controlled-release pharmaceuticals may allow once daily administration of medication in the morning. This is especially helpful for children who do not like taking their medication in the middle of the school day. Several controlled-release methods are used.
Stimulants used to treat ADHD raise the extracellular concentrations of the neurotransmitters dopamine and norepinephrine, which increases cellular communication between neurons that utilize these compounds. The therapeutic benefits are due to noradrenergic effects at the locus coeruleus and the prefrontal cortex and dopaminergic effects at the ventral tegmental area, nucleus accumbens, and prefrontal cortex.[17][18]
Stimulant medications are considered safe when used under medical supervision.[6] Nonetheless, there are concerns that the long term safety of these drugs has not been adequately documented,[7][8][10][9] as well as social and ethical issues regarding their use and dispensation. The U.S. FDA has added black-box warnings to some ADHD medications, warning that abuse can lead to psychotic episodes, psychological dependence, and that severe depression may occur during withdrawal from abusive use.[19]
Stimulants are the most effective medications available for the treatment of ADHD.[20] Seven different formulations of stimulants have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of ADHD: four amphetamine-based formulations, two methylphenidate-based formulations, and dextromethamphetamine hydrochloride. Atomoxetine, guanfacine and clonidine are the only non-controlled, non-stimulant FDA approved drugs for the treatment of ADHD.
Short-term clinical trials have shown medications to be effective for treating ADHD, but the trials usually use exclusion criteria, meaning knowledge of medications for ADHD is based on a small subset of the typical patients seen in clinical practice.[21] They have not been found to improve school performance and data is lacking on long-term effectiveness and the severity of side effects. Stimulants, however, may reduce the risk of unintentional injuries in children with ADHD.[22][23]
This class of medicines is generally regarded as one unit; however, they affect the brain differently.[24] Some investigations are dedicated to finding the similarities of children who respond to a specific medicine.[24] The behavioral response to stimulants in children is similar regardless of whether they have ADHD or not.[25]
Stimulant medication is an effective treatment[26] for adult attention-deficit hyperactivity disorder[27][28] although the response rate may be lower for adults than children.[29] Some physicians may recommend antidepressant drugs as the first line treatment instead of stimulants[30] although antidepressants have much lower treatment effect sizes than stimulant medication.[31]
Amphetamine
| Brand name |
United States Adopted Name |
(D:L) ratio |
Dosage form |
Marketing start date |
Sources |
|---|---|---|---|---|---|
| Adderall | – | 3:1 (salts) | tablet | 1996 | [32][33] |
| Adderall XR | – | 3:1 (salts) | capsule | 2001 | [32][33] |
| Mydayis | – | 3:1 (salts) | capsule | 2017 | [34] |
| Adzenys XR | amphetamine | 3:1 (base) | ODT | 2016 | [35][36] |
| Dyanavel XR | amphetamine | 3.2:1 (base) | suspension | 2015 | |
| Evekeo | amphetamine sulfate | 1:1 (salts) | tablet | 2012 | [39][40] |
| Dexedrine | dextroamphetamine sulfate | 1:0 (salts) | capsule | 1976 | [32][33] |
| ProCentra | dextroamphetamine sulfate | 1:0 (salts) | liquid | 2010 | [33] |
| Zenzedi | dextroamphetamine sulfate | 1:0 (salts) | tablet | 2013 | [33] |
| Vyvanse | lisdexamfetamine dimesylate | 1:0 (prodrug) | capsule | 2007 | [32][41] |
| tablet |
Amphetamine is a chiral compound which is composed of two isomers: levoamphetamine and dextroamphetamine. Levoamphetamine and dextroamphetamine have the same chemical formula but are mirror images of each other, the same way that a person's hands are the same but are mirror images of each other. This mirror difference is enough to produce a small difference in their pharmacological properties; levoamphetamine has a slightly longer half-life than dextroamphetamine, but dextroamphetamine is a more potent central nervous system stimulant. Although it is effective in reducing primary ADHD symptoms such as hyperactivity and inattention, multiple adverse side effects presented. Included in these were headaches, anxiety, nausea and insomnia.[42]
Five different amphetamine-based pharmaceuticals are currently used in ADHD treatment: racemic amphetamine, dextroamphetamine, lisdexamfetamine, and two mixed enantiomer products (Adderall and Dyanavel XR).[32][39] Lisdexamfetamine is an inactive prodrug of dextroamphetamine (i.e., lisdexamfetamine itself doesn't do anything in the body, but it metabolizes into dextroamphetamine).[32] Adderall is a proprietary mixture of (75%) dextroamphetamine and (25%) levoamphetamine salts, which results in very mild differences between their effects.[32] Dyanavel XR contains a similar mixture. Adderall begins to work before dextroamphetamine because of levoamphetamine.[43] Levoamphetamine also provides Adderall with a longer clinical effect than dextroamphetamine. Some children with ADHD and comorbid disorders respond well to levoamphetamine.[24]
Methamphetamine
The body metabolizes methamphetamine into amphetamine (in addition to less active metabolites). A quarter of methamphetamine will ultimately become amphetamine.[44] After comparing only the common ground between dextroamphetamine and dextromethamphetamine, the latter is said to be the stronger stimulant.[45]
Methylphenidate
| Brand name(s) | Generic name(s)[lower-alpha 1] | Duration | Dosage form |
|---|---|---|---|
| Ritalin | methylphenidate | 3–4 hours[50] | tablet |
| Focalin (US) | dexmethylphenidate (US)[lower-alpha 2] | 3–4 hours[50] | tablet |
| Aptensio XR (US); Biphentin (CA) |
Currently unavailable | 12 hours[lower-alpha 3] | XR capsule |
| Concerta (US/CA); Concerta XL (UK) |
methylphenidate ER (US/CA);[lower-alpha 4] methylphenidate ER‑C (CA)[lower-alpha 5] |
12 hours[53] | OROS tablet |
| Focalin XR (US) | dexmethylphenidate XR (US)[lower-alpha 6] | 12 hours[50] | XR capsule |
| Quillivant XR (US) | Currently unavailable | 12 hours[53] | oral suspension |
| Daytrana (US) | Currently unavailable | 11 hours[54] | transdermal patch |
| Metadate CD (US); Equasym XL (UK) |
methylphenidate ER (US)[lower-alpha 7] | 8–10 hours[53] | CD/XL capsule |
| QuilliChew ER (US) | Currently unavailable | 8 hours[55] | chewable tablet |
| Ritalin LA (US); Medikinet XL (UK) |
methylphenidate ER (US)[lower-alpha 8] | 8 hours[53] | ER capsule |
| Ritalin SR (US/CA/UK); Rubifen SR (NZ) |
Metadate ER (US);[lower-alpha 9] Methylin ER (US);[lower-alpha 10] methylphenidate SR (US/CA)[lower-alpha 11] |
5–8 hours[53] | CR tablet |
| |||
Like amphetamine, methylphenidate (MPH) is a chiral compound which is composed of two isomers: d-threo-methylphenidate (also known as dexmethylphenidate, d-methylphenidate, or d-MPH) and l-threo-methylphenidate (also known as l-methylphenidate or l-MPH). Both isomers have the same chemical formula but are mirror images of each other, the same way that a person's hands are the same but are mirror images of each other. Unlike amphetamine, the difference in pharmacological properties between d-MPH and l-MPH is significant, as l-MPH is markedly inferior to d-MPH in its effects, which is due to a number of major differences between the isomers.[56][57]
There are two major medications derived from methylphenidate's isomers: a racemic mixture of half d-threo-methylphenidate and half l-threo-methylphenidate called methylphenidate (Ritalin, Concerta), and an enantiopure formulation containing just d-threo-methylphenidate called dexmethylphenidate (Focalin).
Non-stimulants
Atomoxetine,[58] guanfacine, and clonidineare drugs approved for the treatment of ADHD that have been classified as "non-stimulant".
- Atomoxetine
- Atomoxetine is less effective than stimulants for ADHD, is associated with rare cases of liver damage,[59]:5 and carries a U.S. FDA black box warning regarding suicidal ideation.[60] Controlled studies show increases in heart rate, decreases of body weight, decreased appetite and treatment-emergent nausea.[61]
- Guanfacine
- The extended release form has been approved by the FDA for the treatment of attention-deficit hyperactivity disorder (ADHD) in children as an alternative to stimulant medications. Its beneficial actions are likely due to its ability to strengthen prefrontal cortical regulation of attention and behavior.[62]
- Clonidine
- An α2A adrenergic receptor agonist has also been approved in the US. Clonidine was initially developed as a treatment for high blood pressure. Low doses in evenings and/or afternoons are sometimes used in conjunction with stimulants to help with sleep and because clonidine sometimes helps moderate impulsive and oppositional behavior and may reduce tics.[63] It may be more useful for comorbid Tourette syndrome.
Other
Some medications used to treat ADHD are prescribed off-label,[64] outside the scope of their FDA-approved indications for various reasons. The U.S. FDA requires two clinical trials to prove a potential drug's safety and efficacy in treating ADHD. The drugs below have not been through these tests, so the efficacy is unproven (however these drugs have been licensed for other indications, so have been proven to be safe in those populations), however proper dosage and usage instructions are not as well characterized.
- Bupropion
- Bupropion is classified as an atypical antidepressant. It is the most common of off-label prescription for ADHD. It inhibits the reuptake of norepinephrine, and to a lesser extent, dopamine, in neuronal synapses,[65] and has little or no effect on serotonergic reuptake.[66] Bupropion is not a controlled substance. It is commonly prescribed as a timed release formulation to decrease the risk of side effects.
- Modafinil
- A wakefulness-promoting agent that operates primarily as a selective, relatively weak, and atypical dopamine reuptake inhibitor. Double-blind randomized controlled trials have demonstrated the efficacy and tolerability of modafinil in pediatric ADHD,[67][68] however there are risks of serious side effects such as skin reactions and modafinil is not recommended for use in children.[69]:7 In the United States, it was originally pending marketing on-label as Sparlon, but approval was denied by the FDA due to major concerns over the occurrence of Stevens-Johnson Syndrome in clinical trials.[70]
Other medications which may be prescribed off-label include certain antidepressants such as tricyclic antidepressants (TCAs), SNRIs, SSRIs, or MAOIs.[3][4][2]
Antipsychotic medication
Atypical antipsychotic medications, which are approved for the treatment of certain behavioral disorders, are sometimes prescribed off-label as a combination therapy with stimulants for the treatment of comorbid (i.e., co-occurring diseases) ADHD and disruptive behavioral disorders.[71][72] Canadian clinical practice guidelines only support the use of dopaminergic antipsychotics with selectivity for D2-type dopamine receptors, particularly risperidone, as a third-line treatment for both disorders following the failure of stimulant monotherapy and psychosocial interventions.[71][73] Combined use of D2-type receptor antagonists and ADHD stimulants for the treatment of ADHD with comorbid behavioral disorders does not appear to have significantly worse adverse effects than ADHD stimulant or antipsychotic monotherapy.[71][74] Research suggests, but has not yet confirmed, the treatment efficacy of antipsychotic and stimulant combination treatment for both disorders;[71] it is unclear if the combination therapy for both disorders is superior to stimulant or antipsychotic monotherapy.[71] There is no evidence to support the use of any subclass of antipsychotics for the treatment of the core symptoms of ADHD (i.e., inattention and hyperactivity) without comorbid behavioral disorders.[75]
Dopaminergic antipsychotics affect dopamine neurons by binding to postsynaptic dopamine receptors, where they function as receptor antagonists;[74] in contrast, ADHD stimulants are indirect agonists of postsynaptic dopamine receptors;[74] in other words, these stimulants increase levels of synaptic dopamine which then binds to postsynaptic receptors.[74] Stimulants increase the concentration of synaptic dopamine by activating certain presynaptic receptors (i.e., TAAR1) or by blocking or altering the function of reuptake transporters (e.g., DAT, VMAT2) in the presynaptic neuron.
Comparison
| Generic Name (INN) | Brand Name(s) | TGA-labelled for ADHD? | MHRA-labelled for ADHD? | FDA-labelled for ADHD? | Pharmacological class[76] | Level of support | Efficacy and miscellany[lower-alpha 1] | |
|---|---|---|---|---|---|---|---|---|
| Central nervous system stimulants | ||||||||
| Classical | ||||||||
| Amphetamine (racemic) |
Evekeo[39][40] | Not available | Not available | Children ≥3 years & adults | Monoamine reuptake inhibitor & releasing agent | Approved | Highly efficacious with rapid onset of action. 1:1 mix of d-amp & l-amp. | |
| Adderall[lower-alpha 2] | Adderall[81] | Not available | Not available | Children ≥3 years & adults | Monoamine reuptake inhibitor & releasing agent | Approved | Highly efficacious,[82][83] therapeutic effects are usually seen within an hour of oral administration. 3:1 mix of d-amp and l-amp. | |
| Dexamfetamine | Dexedrine, Dexrostat |
Children ≥6 years & adults | Children ≥6 years & adults | Children ≥3 years & adults | Monoamine reuptake inhibitor & releasing agent | Approved | Highly efficacious,[82][83] therapeutic effects are usually seen within 1–1.5 hours of oral administration. | |
| Lisdexamfetamine | Vyvanse, Elvanse[84] |
Children ≥6 years & adults | Children ≥6 years & adults | Children ≥6 years & adults | Monoamine reuptake inhibitor & releasing agent | Approved | Highly efficacious,[82] therapeutic effects are usually seen within 1–3 hours of oral administration. This is a prodrug formulation of d-amp. | |
| Methamphetamine | Desoxyn[85] | Not available | Not available | Children ≥6 years & adults | Monoamine reuptake inhibitor & releasing agent | Approved | Highly efficacious, therapeutic effects are usually seen within an hour of oral administration. | |
| Methylphenidate | Ritalin, Concerta[86] |
Children ≥6 years & adults | Children ≥6 years & adults | Children ≥6 years & adults | NDRI | Approved | Highly efficacious,[82][83] therapeutic effects are usually seen within 0.5–1.5 hours of oral administration (depending on formulation). | |
| Dexmethylphenidate | Focalin[87] | Not available | Not available | Children ≥6 years & adults | NDRI | Approved | Highly efficacious,[83] therapeutic effects are usually seen within 0.5–1.5 hours of oral administration (depending on formulation). No significant advantages over methylphenidate at equipotent dosages. | |
| Non-classical | ||||||||
| Atomoxetine | Strattera[88] | Children ≥6 years & adults | Children ≥6 years & adults | Children ≥6 years & adults | NRI | Approved | Less efficacious than classical stimulants[82][83] and slower onset of action (usually takes at least a couple weeks). | |
| Modafinil | Provigil, Modavigil[89] |
No | No | No | Dopamine reuptake inhibitor | Very high | Rapid onset of action (several hours). Level of support enough to potentially gain approval for pediatric ADHD, however the FDA rejected approval due to concerns over serious skin reactions.[70] Poorly evaluated for adult ADHD as most published research trials focus on pediatric ADHD.[70] | |
| α2 adrenoceptor agonists | ||||||||
| Clonidine | Catapres, Dixarit, Kapvay[90] |
No | No | Children ≥6 years | α2 adrenoceptor agonist | Approved | Delayed onset of action (1 week). Insufficient data to judge its relative efficacy. Only the more sedating, immediate-release formulations are available in some countries, including Australia.[91] | |
| Guanfacine | Intuniv, Tenex[92] |
Not available | Children ≥6 years | Children ≥6 years | α2 adrenoceptor agonist | Approved | Delayed onset of action (1 week). May be slightly less efficacious than stimulant medications.[82] Not available in many countries. | |
| Antidepressants/Anxiolytics | ||||||||
| Amitriptyline | Elavil, Endep[93] |
No | No | No | Tricyclic | Low[94] | Delayed onset of action. | |
| Bupropion | Wellbutrin[95] | No | No | No | NDRI & nAChR antagonist | High[96] | Delayed onset of action. Probably less efficacious than atomoxetine and classical stimulant medications in children. May be slightly more effective than atomoxetine in adults, however. | |
| Buspirone | Buspar[97] | No | No | No | 5-HT1A partial agonist | Low[lower-alpha 3] | Delayed onset of action. Being a 5-HT1A receptor partial agonist may afford it the ability to increase dopamine release in the prefrontal cortex.[102][103] | |
| Clomipramine | Anafranil | No | No | No | Tricyclic | Low[104] | Delayed onset of action. | |
| Desipramine | Norpramin[105] | No | No | No | Tricyclic | Moderate[106] | Delayed onset of action. | |
| Duloxetine | Cymbalta[107] | No | No | No | SNRI | Moderate[108] | Delayed onset of action. | |
| Imipramine | Tofranil[109] | No | No | No | Tricyclic | Low[110] | Delayed onset of action. | |
| Milnacipran | Savella, Ixel[111] |
No | No | No | SNRI | Negligible[112] | Delayed onset of action. | |
| Moclobemide | Aurorix | No | No | Not available | Reversible MAO-A inhibitor | Low[113] | Delayed onset of action. | |
| Nortriptyline | Pamelor, Allegron[114] |
No | No | No | Tricyclic | Low[lower-alpha 4] | Delayed onset of action. | |
| Reboxetine | Edronax | No | No | Not available | Norepinephrine reuptake inhibitor | Low[117] | Delayed onset of action. | |
| Selegiline | Emsam | No | No | No | Monoamine oxidase inhibitor | Low[118] | Delayed onset of action. | |
| Venlafaxine | Effexor[119] | No | No | No | SNRI | Moderate[120] | Delayed onset of action. | |
| Miscellaneous others | ||||||||
| Amantadine | Endantadine, Symmetrel[121] |
No | No | No | NMDA antagonist and dopamine agonist | Low[122] | ? | |
| Carbamazepine | Equetro, Tegretol[123] |
No | No | No | Sodium channel blocker | Moderate[124] | Use in ADHD is generally considered clinically inadvisable.[125] | |
| Memantine | Namenda[126] | No | No | No | NMDA antagonist | Low[127] | ? | |
|
Levels of support
| ||||||||
| Notes | ||||||||
Concerns regarding stimulants
Some parents and professionals have raised questions about the side effects of drugs and their long-term use.[64]
Increasing use
Outpatient treatment rates have held steady in the U.S. recently. Prior to this, outpatient treatment for ADHD in the U.S. grew from 0.9 children per 100 in 1987 to 3.4 per 100 in 1997.[128] A survey conducted by the Centers for Disease Control and Prevention in 2011–2012 found 11% of children between the ages of 4 and 17 were reported to have ever received a health care provider diagnosis of ADHD at some point (15% of boys and 7% of girls), a 16% increase since 2007 and a 41% increase over the last decade.[129] The CDC notes that community samples suggest the incidence of ADHD in American children is higher than the five percent stated by the American Psychiatric Association in DSM-5, with 8.8% of U.S. children having a current diagnosis in the 2011 survey.[129][130] However, only 6.1% of children in the 2011 survey were taking ADHD medication, suggesting as many as 17.5% of children with current ADHD were not receiving treatment.[129]
Use in preschoolers
Parents of children with ADHD note that they usually display their symptoms at an early age. There have been few longitudinal studies on the long-term effects of stimulant use in children.[131] The use of stimulant medication has not been approved by the FDA for children under the age of six.[132] A growing trend is the diagnosis of younger children with ADHD. Prescriptions for children under the age of 5 rose nearly 50 percent from 2000 to 2003.[133][134] Research on this issue has indicated that stimulant medication can help younger children with "severe ADHD symptoms" but typically at a lower dose than older children. It was also found that children at this age are more sensitive to side effects and should be closely monitored.[132] Evidence suggests that careful assessment and highly individualized behavioural interventions significantly improve both social and academic skills,[1][135] while medication only treats the symptoms of the disorder. "One of the primary reasons cited for the growing use of psychotropic interventions was that many physicians realize that psychological interventions are costly and difficult to sustain."[136]
Side effects
Growth delay and weight loss
There is some evidence of mild reductions in growth rate with prolonged stimulant treatment in children, but no causal relationship has been established and reductions do not appear to persist long-term.[137] Weight loss almost always corresponds with loss of appetite, which may result from the medication. Severe weight loss is very uncommon though. Loss of appetite is very temporary and typically comes back as daily effects of stimulates wear off. Nausea, dizziness, and headaches, other side effect, can also indirectly affect appetite and result in weight loss.[138]
Cardiovascular
There is concern that stimulants and atomoxetine, which increase the heart rate and blood pressure, might cause serious cardiovascular problems.[139] Recent extremely large-scale studies by the FDA indicate that, in children, young adults, and adults, there is no association between serious adverse cardiovascular events (sudden death, myocardial infarction, and stroke) and the medical use of amphetamine, methylphenidate, or other ADHD stimulants.[140][141][142][143]
Psychiatric
Many of these drugs are associated with physical and psychological dependence.[144] Sleep problems may occur.[145]
Methylphenidate can worsen psychosis in psychotic patients, and in very rare cases it has been associated with the emergence of new psychotic symptoms.[146] It should be used with extreme caution in patients with bipolar disorder due to the potential induction of mania or hypomania.[147] There have been very rare reports of suicidal ideation, but evidence does not support a link.[137] The long-term effects on mental health disorders in later life of chronic use of methylphenidate is unknown.[148]
A 2009 FDA review of 49 clinical trials found that approximately 1.5% of children in clinical trials of medications for ADHD had experienced signs or symptoms of psychosis or mania. Postmarketing reports were also analyzed, with nearly half of them involving children under the age of eleven. Approximately 90% of cases had no reported previous history of similar psychiatric events. Hallucinations involving snakes, worms or insects were the most commonly reported symptoms.[149]
Long-term use
Long-term methylphenidate or amphetamine exposure in some species is known to produce abnormal dopamine system development or nerve damage,[150][151] but humans experience normal development and nerve growth.[152][153][154] Magnetic resonance imaging studies suggest that long-term treatment with amphetamine or methylphenidate decreases abnormalities in brain structure and function found in subjects with ADHD, and improves function of the right caudate nucleus.[152][153][154]
Reviews of clinical stimulant research have established the safety and effectiveness of long-term amphetamine use for ADHD.[155][156] Controlled trials spanning two years have demonstrated continuous treatment effectiveness and safety.[156][157] One review highlighted a 9-month randomized controlled trial of amphetamine in children that found an average increase of 4.5 IQ points and continued improvements in attention, disruptive behaviors, and hyperactivity.[157]
Withdrawal and rebound
Tolerance to the therapeutic effects of stimulants can occur,[158] and rebound of symptoms may occur when the dose wears off.[159] Rebound effects are often the result of the stimulant dosage being too high or the individual not being able to tolerate stimulant medication. Signs that the stimulant dose is too high include irritability, feeling stimulated or blunting of affect and personality.[160]
Stimulant withdrawal or rebound reactions can occur and can be minimised in intensity via a gradual tapering off of medication over a period of weeks or months.[161] A small study of abrupt withdrawal of stimulants did suggest that withdrawal reactions are not typical, and may only occur in susceptible individuals.[162]
Cancer
Concerns about chromosomal aberrations and possible cancer later in life was raised by a small-scale study on the use of methylphenidate, though a review by the Food and Drug Administration (FDA) found significant methodological problems with the study.[163] A follow-up study performed with improved methodology found no evidence that methylphenidate might cause cancer, stating "the concern regarding a potential increase in the risk of developing cancer later in life after long-term MPH treatment is not supported."[164]
History
The first reported evidence of stimulant medication used to treat children with concentration and hyperactivity problems came in 1937.[165] Charles Bradley in Providence, Rhode Island reported that a group of children with behavioral problems improved after being treated with the stimulant Benzedrine.[165][166] In 1954, the stimulant methylphenidate (Ritalin, which was first produced in 1944) became available; it remains one of the most widely prescribed medications for ADHD.[165] Initially the drug was used to treat narcolepsy, chronic fatigue, depression, and to counter the sedating effects of other medications.[165] The drug began to be used for ADHD in the 1960s and steadily rose in use.
In 1975, pemoline (Cylert) was approved by the U.S. FDA for use in the treatment of ADHD. While an effective agent for managing the symptoms, the development of liver failure in 14 cases over the next 27 years would result in the manufacturer withdrawing this medication from the market. New delivery systems for medications were invented in 1999 that eliminated the need for multiple doses across the day or taking medication at school. These new systems include pellets of medication coated with various time-release substances to permit medications to dissolve hourly across an 8–12 hour period (Metadate CD, Adderall XR, Focalin XR) and an osmotic pump that extrudes a liquid methylphenidate sludge across an 8–12 hour period after ingestion (Concerta).
In 2003, atomoxetine (Strattera) received the first FDA approval for a nonstimulant drug to be used specifically for ADHD.[167] In 2007, lisdexamfetamine (Vyvanse) became the first prodrug[168] for ADHD to receive FDA approval.[169] In March 2019, a Purdue Pharma subsidiary received approval from the FDA for Adhansia XR, a methylphenidate medication to treat ADHD.[170]
Cost-effectiveness
Combined medical management and behavioral treatment is the most effective ADHD management strategy, followed by medication alone, and then behavioral treatment.[20] In terms of cost-effectiveness, management with medication has been shown to be the most cost-effective, followed by behavioral treatment, and combined treatment.[20] The individually most effective and cost-efficient way is with stimulant medication. Additionally, long-acting medications for ADHD, in comparison to short-acting varieties, generally seem to be cost-effective.[171] Comorbid (relating to two diseases that occur together, e.g. depression and ADHD) disorders makes finding the right treatment and diagnosis much more costly than when comorbid disorders are absent.
Alternative medicine
Most alternative therapies do not have enough supporting evidence to recommend them.[172][173] Moreover, when only the best conducted studies are taken into account results tend to be similar to placebo.[173]
Neurofeedback
Neurofeedback (NF) or EEG biofeedback is a treatment strategy used for children, adolescents and adults with ADHD.[174] The human brain emits electrical energy which is measured with electrodes. Neurofeedback alerts the patient when beta waves are present. This theory believes that those with ADHD can train themselves to decrease ADHD symptoms.
No serious adverse side effects from neurofeedback have been reported.[175] Research into neurofeedback has been mostly limited and of low quality.[175] While there is some indication on the effectiveness of biofeedback it is not conclusive: several studies have yielded positive results, however the best designed ones have either shown reduced effects or non-existing ones.[175][176] In general no effects have been found in the most blinded ADHD measures, which could be indicating that positive results are due to the placebo effect.[177]
Media
Preliminary studies have supported the idea that playing video games that are proven to help cognition is a form of neurofeedback, which helps those with ADHD self-regulate and improve learning.[178][179] On the other hand, ADHD may experience great difficulty disengaging from the game, which may in turn negate any benefits gained from these activities,[180] and time management skills may be negatively impacted as well.[181]
Nature
Children who spend time outdoors in natural settings, such as parks, seem to display fewer symptoms of ADHD, which has been dubbed "Green Therapy".[182]
Diet
There is insufficient evidence to support dietary changes in ADHD and thus they are not recommended by the American Academy of Pediatrics as of 2019.[183] Perhaps the best known of the dietary alternatives is the Feingold diet which involves removing salicylates, artificial colors and flavors, and certain synthetic preservatives from children's diets.[184] However, studies have shown little if any effect of the Feingold diet on the behavior of children with ADHD.[185]
Results of studies regarding the effect of eliminating artificial food coloring from the diet of children with ADHD have been very varied. It has been found that it might be effective in some children but as the published studies have been of low quality results can be more related to research problems such as publication bias.[186] The UK Food Standards Agency (FSA) has called for a ban on the use of six artificial food colorings[187] and the European Union (EU) has ruled that some food dyes must be labeled with the relevant E number as well as this warning: "may have an adverse effect on activity and attention in children."[188] Nevertheless, existing evidence neither refutes nor supports the association between ADHD and food colouring.[189]
Dietary supplements and specialized diets are sometimes used by people with ADHD with the intent to mitigate some or all of the symptoms. However a 2009 article in the Harvard Mental Health Letter states, "Although vitamin or mineral supplements [micronutrients] may help children diagnosed with particular deficiencies, there is no evidence that they are helpful for all children with ADHD. Furthermore, megadoses of vitamins, which can be toxic, must be avoided."[190] In the United States, no dietary supplement has been approved for the treatment for ADHD by the FDA.[191]
Some popular supplements used to manage ADHD symptoms:
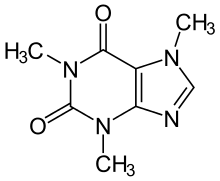
- Caffeine – ADHD is associated with increased caffeine consumption, and caffeine's stimulant effects on cognition may have some benefits for ADHD.[192] Limited evidence suggests a small therapeutic effect that is markedly inferior to standard treatments like methylphenidate and dextroamphetamine while still producing similar or greater side effects.[192][193]
- Nicotine – The association between ADHD and nicotine intake is well known, and limited evidence suggests that nicotine may help improve some of the symptoms of ADHD, although the effect is generally small.[194][195][196]
- Omega-3 fatty acids – A 2012 Cochrane review found little evidence that supplementation with omega-3 or other polyunsaturated fatty acids provides any improvement in the symptoms of ADHD in children or adolescents.[197] A 2011 meta analysis found a "small but significant benefit", with benefits being "modest compared to the efficacy of currently available pharmacological treatments for ADHD".[198] The review concluded that supplementation may be worth consideration as an augmentative treatment in combination with medication due to its "relatively benign side-effect profile", but not as a primary treatment.[198] Most research on Omega-3 fatty acids is considered to be of very poor quality with widespread methodological weaknesses.[197][198]
- Zinc – Although the role of zinc in ADHD has not been elucidated, there is a small amount of limited evidence that lower tissue zinc levels may be associated with ADHD.[199] In the absence of a demonstrated zinc deficiency (which is rare outside of developing countries), zinc supplementation is not recommended as a treatment option for ADHD.[200]
- In the 1980s vitamin B6 was promoted as a helpful remedy for children with learning difficulties including inattentiveness; however, a study of large doses of vitamins with ADHD children showed that they were ineffective in changing behavior.[201]
Comorbid disorders
Because ADHD comorbidities are diverse and the rate of comorbidity is high, special care must dedicated to certain comorbidities. The FDA is not set up to address this issue, and does not approve medications for comorbidities, nonetheless certain such topics have been extensively researched.
Tic disorders
Patients with Tourette syndrome who are referred to specialty clinics have a high rate of comorbid ADHD. Patients who have ADHD along with tics or tic disorders may also have problems with disruptive behaviors, overall functioning, and cognitive function, accounted for by the comorbid ADHD.[202]
The treatment of ADHD in the presence of tic disorders has long been a controversial topic. Past medical practice held that stimulants could not be used in the presence of tics, due to concern that their use might worsen tics;[203] however, multiple lines of research have shown that stimulants can be cautiously used in the presence of tic disorders.[204][162] Several studies have shown that stimulants do not exacerbate tics any more than placebo does, and suggest that stimulants may even reduce tic severity.[205] A 2011 Cochrane Collaboration review concluded that most major ADHD medications were effective in children with tics, and that stimulants did not generally worsen tics outside of individual cases.[206] Methylphenidate, guanfacine, clonidine, and desipramine were associated with improvement of tic symptoms.[206] Controversy remains, and the PDR continues to carry a warning that stimulants should not be used in the presence of tic disorders, so physicians may be reluctant to use them. Others are comfortable using them and even advocate for a stimulant trial when ADHD co-occurs with tics, because the symptoms of ADHD can be more impairing than tics.[203][207]
The stimulants are the first line of treatment for ADHD, with proven efficacy, but they do fail in up to 20% of cases, even in patients without tic disorders.[208] Current prescribed stimulant medications include: methylphenidate, dextroamphetamine, and mixed amphetamine salts (Adderall). Other medications can be used when stimulants are not an option. These include the alpha-2 agonists (clonidine and guanfacine), tricyclic antidepressants (desipramine and nortriptyline), and newer antidepressants (bupropion and venlafaxine). There have been case reports of tics worsening with bupropion. There is good empirical evidence for short-term safety and efficacy for the use of desipramine, bupropion and atomoxetine.[208]
References
- Wolraich, M.; Brown, L.; Wolraich, RT.; Brown, G.; Brown, M.; Dupaul, HM.; Earls, TG.; Feldman, B.; et al. (November 2011). Steering Committee on Quality Improvement Management. "ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents". Pediatrics. 128 (5): 1007–22. doi:10.1542/peds.2011-2654. PMC 4500647. PMID 22003063.
- Stein MA (July 2004). "Innovations in attention-deficit/hyperactivity disorder pharmacotherapy: long-acting stimulant and nonstimulant treatments". American Journal of Managed Care. 10 (4 Suppl): S89–98. PMID 15352535.
- Christman AK, Fermo JD, Markowitz JS (August 2004). "Atomoxetine, a novel treatment for attention-deficit-hyperactivity disorder". Pharmacotherapy. 24 (8): 1020–36. doi:10.1592/phco.24.11.1020.36146. PMID 15338851.
- Hazell, P (October 2005). "Do adrenergically active drugs have a role in the first-line treatment of attention-deficit/hyperactivity disorder?". Expert Opinion on Pharmacotherapy. 6 (12): 1989–98. doi:10.1517/14656566.6.12.1989. PMID 16197353.
- Waxmonsky, James (October 2003). "Assessment and treatment of attention deficit hyperactivity disorder in children with comorbid psychiatric illness". Current Opinion in Pediatrics. 15 (5): 476–482. doi:10.1097/00008480-200310000-00006. PMID 14508296.
- American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder and Committee on Quality Improvement. (October 2001). "Clinical practice guideline: treatment of the school-aged child with attention-deficit/hyperactivity disorder". Pediatrics. 108 (4): 1033–44. doi:10.1542/peds.108.4.1033. PMID 11581465.CS1 maint: uses authors parameter (link)
- King, S; Griffin, S; Hodges, Z (July 2006). "A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents". Health Technology Assessment. 10 (23): iii–iv, xiii–146. doi:10.3310/hta10230. PMID 16796929. Archived from the original on 15 August 2009.
- Murphy, Kevin R; Barkley, Russell A (2005). Attention-Deficit Hyperactivity Disorder: A Clinical Workbook (Third ed.). New York: Guilford Press. ISBN 978-1-59385-227-6.
- Lerner M, Wigal T (January 2008). "Long-term safety of stimulant medications used to treat children with ADHD". Pediatric Annals. 37 (1): 37–45. doi:10.3928/00904481-20080101-11. PMID 18240852.
- Stern HP, Stern TP (September 2002). "When children with attention-deficit/hyperactivity disorder become adults". South. Med. J. 95 (9): 985–91. doi:10.1097/00007611-200209000-00011. PMID 12356139.
- Kazdin, Alan E. Parent management training : treatment for oppositional, aggressive, and antisocial behavior in children and adolescents. Oxford University Press, 2005
- Melby-Lervåg M, Hulme C (February 2013). "Is working memory training effective? A meta-analytic review". Dev Psychol. 49 (2): 270–91. CiteSeerX 10.1.1.281.7759. doi:10.1037/a0028228. PMID 22612437.
- Sonuga-Barke, E; Brandeis, D; Holtmann, M; Cortese, S (October 2014). "Computer-based Cognitive Training for ADHD: A Review of Current Evidence". Child and Adolescent Psychiatric Clinics of North America. 23 (4): 807–824. doi:10.1016/j.chc.2014.05.009. PMID 25220088.
- Sulzer D, Sonders MS, Poulsen NW, Galli A (April 2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Progress in Neurobiology. 75 (6): 406–33. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
- Howland RH (August 2008). "Lisdexamfetamine: a prodrug stimulant for ADHD". Journal of Psychosocial Nursing and Mental Health Services. 46 (8): 19–22. doi:10.3928/02793695-20080801-05. PMID 18777964.
- National Toxicology Program (July 2005). "NTP-CERHR monograph on the potential human reproductive and developmental effects of amphetamines". NTP Cerhr Mon (16): vii–III1. PMID 16130031.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapters 10 and 13". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 266, 318–323. ISBN 978-0-07-148127-4.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 148, 154–157. ISBN 978-0-07-148127-4.
- "Full U.S. CONCERTA® Prescribing Information". Janssen Pharmaceuticals, Inc. 15 July 2014. Archived from the original on 26 November 2014. Retrieved 6 September 2014.
- Jensen; Garcia, JA; Glied, S; Crowe, M; Foster, M; Schlander, M; Hinshaw, S; Vitiello, B; Arnold, LE (2005). "Cost-Effectiveness of ADHD Treatments: Findings from the Multimodal Treatment Study of Children With ADHD". American Journal of Psychiatry. 162 (9): 1628–1636. doi:10.1176/appi.ajp.162.9.1628. hdl:1811/51178. PMID 16135621.
- Weiss MD, Gadow K, Wasdell MB (2006). "Effectiveness outcomes in attention-deficit/hyperactivity disorder". J Clin Psychiatry. 67 Suppl 8: 38–45. PMID 16961429.
- Ruiz-Goikoetxea, Maite; Cortese, Samuele; Aznarez-Sanado, Maite; Magallón, Sara; Alvarez Zallo, Noelia; Luis, Elkin O.; de Castro-Manglano, Pilar; Soutullo, Cesar; Arrondo, Gonzalo (2018). "Risk of unintentional injuries in children and adolescents with ADHD and the impact of ADHD medications: A systematic review and meta-analysis". Neuroscience & Biobehavioral Reviews. 84: 63–71. doi:10.1016/j.neubiorev.2017.11.007. ISSN 0149-7634. PMID 29162520.
- Dalsgaard, Søren; Leckman, James F.; Mortensen, Preben Bo; Nielsen, Helena Skyt; Simonsen, Marianne (1 August 2015). "Effect of drugs on the risk of injuries in children with attention deficit hyperactivity disorder: a prospective cohort study". The Lancet. Psychiatry. 2 (8): 702–709. doi:10.1016/S2215-0366(15)00271-0. ISSN 2215-0374. PMID 26249301.
- Arnold LE (2000). "Methylphenidate vs Amphetamine: Comparative Review". Journal of Attention Disorders. 3 (4): 200–211. doi:10.1177/108705470000300403.
- Rapoport JL, Inoff-Germain G (2002). "Responses to methylphenidate in Attention-Deficit/Hyperactivity Disorder and normal children: update 2002". J Atten Disord. 6 Suppl 1: S57–60. doi:10.1177/070674370200601s07. PMID 12685519.
- Dusan Kolar; Amanda Keller; Maria Golfinopoulos; Lucy Cumyn; Cassidy Syer; Lily Hechtman (February 2008). "Treatment of adults with attention-deficit/hyperactivity disorder". Neuropsychiatr Dis Treat. 4 (1): 107–121. doi:10.2147/ndt.s1747. PMC 2515906. PMID 18728812.
- Spencer TJ. (April 2007). "Pharmacology of adult ADHD with stimulants". CNS Spectr. 12 (4(supplement 6)): 8–11. doi:10.1017/S1092852900026018. PMID 17715564.
- Rostain, Anthony L. (September 2008). "ADHD in Adults: Attention-Deficit/Hyperactivity Disorder in Adults: Evidence-Based Recommendations for Management". Postgraduate Medicine. 120 (3): 27–38. doi:10.3810/pgm.2008.09.1905. PMID 18824823.
- Spencer, Thomas; Biederman, Joseph; Wilens, Timothy (June 2004). "Stimulant treatment of adult attention-deficit/hyperactivity disorder". Psychiatric Clinics of North America. 27 (2): 361–372. doi:10.1016/j.psc.2003.12.002. PMID 15064002.
- Higgins ES (January 1999). "A comparative analysis of antidepressants and stimulants for the treatment of adults with attention-deficit hyperactivity disorder". J Fam Pract. 48 (1): 15–20. PMID 9934377.
- Verbeeck W, Tuinier S, Bekkering GE (February 2009). "Antidepressants in the treatment of adult attention-deficit hyperactivity disorder: a systematic review". Adv Ther. 26 (2): 170–184. doi:10.1007/s12325-009-0008-7. PMID 19238340.
- Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present – a pharmacological and clinical perspective". J. Psychopharmacol. 27 (6): 479–496. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
- "National Drug Code Amphetamine Search Results". National Drug Code Directory. United States Food and Drug Administration. Archived from the original on 16 December 2013. Retrieved 16 December 2013.
- "Mydayis Prescribing Information" (PDF). United States Food and Drug Administration. Shire US Inc. June 2017. pp. 1–21. Retrieved 8 August 2017.
- "Adzenys XR-ODT Prescribing Information" (PDF). United States Food and Drug Administration. Neos Therapeutics, Inc. January 2017. p. 16. Retrieved 10 August 2017.
ADZENYS XR-ODT (amphetamine extended-release orally disintegrating tablet) contains a 3 to 1 ratio of d- to l-amphetamine, a central nervous system stimulant.
- "Adzenys XR-ODT". United States Food and Drug Administration. Retrieved 7 March 2016.
- "Evekeo Prescribing Information" (PDF). Arbor Pharmaceuticals LLC. April 2014. pp. 1–2. Retrieved 11 August 2015.
- "Evekeo". United States Food and Drug Administration. Retrieved 11 August 2015.
- "Vyvanse Prescribing Information" (PDF). United States Food and Drug Administration. Shire US Inc. January 2017. pp. 18–21. Retrieved 16 February 2017.
- Punja, Salima (February 2016). "Amphetamines for attention deficit hyperactivity disorder (ADHD) in children and adolescents". Cochrane Database of Systematic Reviews. 2: CD009996. doi:10.1002/14651858.CD009996.pub2. PMID 26844979.
- Glaser; Thomas, TC; Joyce, BM; Castellanos, FX; Gerhardt, GA; et al. (2005). "Differential Effects of Amphetamine Isomers on Dopamine in the Rat Striatum and Nucleus Accumbens Core". Psychopharmacology. 178 (2–3): 250–258 (Page: 255). doi:10.1007/s00213-004-2012-6. PMID 15719230.
- Schepers, RJ (2003). "Methamphetamine and Amphetamine Pharmacokinetics in Oral Fluid and Plasma after Controlled Oral Methamphetamine Administration to Human Volunteers". Clinical Chemistry. 49 (1): 121–132 [121, 130]. doi:10.1373/49.1.121. PMID 12507968.
- Shoblock; Sullivan, EB; Maisonneuve, IM; Glick, SD; et al. (2003). "Neurochemical and Behavioral Differences Between D-Methamphetamine and D-Amphetamine in Rats". Psychopharmacology. 165 (4): 359–369 (Page:366). doi:10.1007/s00213-002-1288-7. PMID 12491026.
- "Education/Training » Clinical Resources". Illinois DocAssist website. University of Illinois at Chicago. Archived from the original on 1 January 2013. Retrieved 26 July 2012.
Ritalin‑SR, methylphenidate SR, Methylin ER, and Metadate ER are the same formulation and have the same drug delivery system
- "Apo‑Methylphenidate SR product monograph" (PDF). Apotex Inc. 31 March 2005. "Comparative Bioavailability" section. Retrieved 26 July 2012. If the monograph link doesn't work, visit Health Canada's Drug Product Database query form one time, then click the monograph link again.
- "New product: Sandoz Methylphenidate SR 20 mg" (PDF). Sandoz Canada Inc. 5 May 2009. Retrieved 26 July 2012.
An alternative to Ritalin‑SR from Novartis
- "Drugs@FDA: FDA Approved Drug Products". Drugs@FDA: FDA Approved Drug Products. US Food and Drug Administration. Retrieved 1 October 2016.
- Sugrue, D; Bogner, R; Ehret, MJ (15 July 2014). "Methylphenidate and dexmethylphenidate formulations for children with attention-deficit/hyperactivity disorder". American Journal of Health-System Pharmacy. 71 (14): 1163–70. doi:10.2146/ajhp130638. PMID 24973373.
- Hosenbocus, S; Chahal, R (November 2009). "A review of long-acting medications for ADHD in Canada". Journal of the Canadian Academy of Child and Adolescent Psychiatry / Journal de l'Academie Canadienne de Psychiatrie de l'Enfant et de l'Adolescent. 18 (4): 331–9. PMC 2765387. PMID 19881943.
- "Aptensio XR Prescribing Information" (PDF). Retrieved 15 April 2017.
- Moses, Scott (26 July 2009). "Methylphenidate". Family Practice Notebook. Retrieved 7 August 2012.
- "Daytrana transdermal". WebMD. Retrieved 11 June 2015.
- "QUILLICHEW ER™ (Methylphenidate HCl extended-release chewable tablets CII) | Pfizer Medical Information – US". www.pfizermedicalinformation.com. Pfizer. Archived from the original on 16 April 2017. Retrieved 16 April 2017.
- Markowitz, JS; Patrick, KS (June 2008). "Differential pharmacokinetics and pharmacodynamics of methylphenidate enantiomers: does chirality matter?". Journal of Clinical Psychopharmacology. 28 (3 Suppl 2): S54–61. doi:10.1097/JCP.0b013e3181733560. PMID 18480678.
- Heal DJ, Pierce DM (2006). "Methylphenidate and its isomers: their role in the treatment of attention-deficit hyperactivity disorder using a transdermal delivery system". CNS Drugs. 20 (9): 713–738 (Page:730). doi:10.2165/00023210-200620090-00002. PMID 16953648.
- "Atomoxetine (marketed as Strattera) Information". U.S. Food and Drug Administration. Archived from the original on 9 July 2009. Retrieved 12 July 2009.
- "Strattera Prescribing Information" (PDF). Eli Lilly and Company. February 2014. Retrieved 6 September 2014.
- "Atomoxetine (marketed as Strattera) Information". FDA Center for Drug Evaluation and Research. 22 February 2007. Archived from the original on 11 May 2009.
- Allen AJ, Kurlan RM, Gilbert DL, Coffey BJ, Linder SL, Lewis DW, Winner PK, Dunn DW, et al. (December 2005). "Atomoxetine treatment in children and adolescents with ADHD and comorbid tic disorders". Neurology. 65 (12): 1941–9. doi:10.1212/01.wnl.0000188869.58300.a7. PMID 16380617.
- Arnsten AF (2010). "The use of alpha-2A adrenergic agonists for the treatment of attention-deficit/hyperactivity disorder". Expert Rev Neurother. 10 (10): 1595–605. doi:10.1586/ern.10.133. PMC 3143019. PMID 20925474.
- Frazin, Natalie (2 April 2002). "Methylphenidate and Clonidine Help Children With ADHD and Tics". National Institute of Neurological Disorders and Stroke. Archived from the original on 27 April 2007. Retrieved 15 April 2007.
- Lakhan, SE; Hagger-Johnson, G (20 October 2007). "The impact of prescribed psychotropics on youth". Clinical Practice and Epidemiology in Mental Health. 3 (1): 21. doi:10.1186/1745-0179-3-21. PMC 2100041. PMID 17949504.

- "Wellbutrin: Prescribing Information" (PDF). (170 KB). GlaxoSmithKline (September 2006). Retrieved 15 April 2007.
- Stahl S, Pradko J, Haight B, Modell J, Rockett C, Learned-Coughlin S (2004). "A Review of the Neuropharmacology of Bupropion, a Dual Norepinephrine and Dopamine Reuptake Inhibitor". Prim Care Companion J Clin Psychiatry. 6 (4): 159–166. doi:10.4088/PCC.v06n0403. PMC 514842. PMID 15361919.
- Biederman J, Swanson JM, Wigal SB, Boellner SW, Earl CQ, Lopez FA (May 2006). "A comparison of once-daily and divided doses of modafinil in children with attention-deficit/hyperactivity disorder: a randomized, double-blind, and placebo-controlled study". The Journal of Clinical Psychiatry. 67 (5): 727–35. doi:10.4088/JCP.v67n0506. PMID 16841622.
- Greenhill LL, Biederman J, Boellner SW (May 2006). "A randomized, double-blind, placebo-controlled study of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 45 (5): 503–11. doi:10.1097/01.chi.0000205709.63571.c9. PMID 16601402.
- Cephalon, Inc. (21 December 2007). "Modavigil Product Information". healthlinks.net. healthlinks.net Pty. Ltd. Archived from the original (PDF) on 21 July 2008. Retrieved 2 July 2008.
- Kumar, R (2008). "Approved and investigational uses of modafinil : an evidence-based review". Drugs. 68 (13): 1803–39. doi:10.2165/00003495-200868130-00003. PMID 18729534.
- Linton, D; Barr, AM; Honer, WG; Procyshyn, RM (May 2013). "Antipsychotic and psychostimulant drug combination therapy in attention deficit/hyperactivity and disruptive behavior disorders: a systematic review of efficacy and tolerability". Current Psychiatry Reports. 15 (5): 355. doi:10.1007/s11920-013-0355-6. PMID 23539465.
- Loy, JH; Merry, SN; Hetrick, SE; Stasiak, K (12 September 2012). "Atypical antipsychotics for disruptive behaviour disorders in children and youths". The Cochrane Database of Systematic Reviews. 9 (9): CD008559. doi:10.1002/14651858.CD008559.pub2. hdl:11343/59236. PMID 22972123.
- Gorman, DA; Gardner, DM; Murphy, AL; Feldman, M; Bélanger, SA; Steele, MM; Boylan, K; Cochrane-Brink, K; Goldade, R; Soper, PR; Ustina, J; Pringsheim, T (February 2015). "Canadian guidelines on pharmacotherapy for disruptive and aggressive behaviour in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder". Canadian Journal of Psychiatry. 60 (2): 62–76. doi:10.1177/070674371506000204. PMC 4344948. PMID 25886657.
CONCLUSION: When severe disruptive or aggressive behaviour occurs with ADHD, medications for ADHD should be used first. Other medications have major adverse effects and, with the exception of risperidone, very limited evidence to support their use.
- Elbe, D; Barr, AM; Honer, WG; Procyshyn, RM (May 2014). "Managing ADHD and disruptive behaviour disorders with combination psychostimulant and antipsychotic treatment". Journal of Psychiatry & Neuroscience. 39 (3): E32–3. doi:10.1503/jpn.130288. PMC 3997610. PMID 24758945.
- Birnbaum ML, Saito E, Gerhard T, Winterstein A, Olfson M, Kane JM, Correll CU (2013). "Pharmacoepidemiology of antipsychotic use in youth with ADHD: trends and clinical implications". Curr Psychiatry Rep. 15 (8): 382. doi:10.1007/s11920-013-0382-3. PMC 4010184. PMID 23881713.
Most importantly, antipsychotics are not approved for the treatment of symptoms of ADHD and limited, if any, evidence exists to suggest their utility for the core symptoms of inattention and hyperactivity. Although, aripiprazole and risperidone are approved for irritability and aggression associated with autistic disorder (age 5 or 6–17 years) (6), and data exist for their utility in disruptive behavior disorders and aggression (37,40), antipsychotics should be the last resort for the treatment of impulsivity, oppositionality and aggression (6,37,41).
- Brunton, L; Chabner, B; Knollman, B (2010). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill Professional. ISBN 978-0-07-162442-8.
- Gozal, David; Molfese, Dennis L (2005). ATTENTION DEFICIT HYPERACTIVITY DISORDER. Contemporary Clinical Neuroscience. Humana Press. ISBN 978-1-58829-312-1.
- Childress, AC; Berry, SA (February 2012). "Pharmacotherapy of Attention-Deficit Hyperactivity Disorder in Adolescents". Drugs. 72 (3): 309–325. doi:10.2165/11599580-000000000-00000. PMID 22316347. (subscription required)
- Santosh, PJ; Sattar, S; Canagaratnam, M (September 2011). "Efficacy and Tolerability of Pharmacotherapies for Attention-Deficit Hyperactivity Disorder in Adults". CNS Drugs. 25 (9): 737–763. doi:10.2165/11593070-000000000-00000. PMID 21870887. (subscription required)
- Faraone, SV; Glatt, SJ (June 2010). "A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes". Journal of Clinical Psychiatry. 71 (6): 754–763. doi:10.4088/JCP.08m04902pur. PMID 20051220. (subscription required)
- "amphetamine/dextroamphetamine (Rx) – Adderall XR, Adderall". Medscape Drugs & Diseases.
- Faraone, SV (December 2009). "Using Meta-analysis to Compare the Efficacy of Medications for Attention-Deficit/Hyperactivity Disorder in Youths". Pharmacy and Therapeutics. 34 (12): 678–694. PMC 2810184. PMID 20140141.
- Faraone, SV; Biederman, J; Spencer, TJ; Aleardi, M (October 2006). "Comparing the Efficacy of Medications for ADHD Using Meta-analysis". MedGenMed. 8 (4): 4. PMC 1868385. PMID 17415287.
- "lisdexamfetamine (Rx) – Vyvanse". Medscape Drugs & Diseases.
- "methamphetamine (Rx) – Desoxyn". Medscape Drugs & Diseases.
- "methylphenidate (Rx) – Ritalin, Ritalin SR". Medscape Drugs & Diseases.
- "dexmethylphenidate (Rx) – Focalin, Focalin XR". Medscape Drugs & Diseases.
- "atomoxetine (Rx) – Strattera". Medscape Drugs & Diseases.
- "modafinil (Rx) – Provigil". Medscape Drugs & Diseases.
- "clonidine (Rx) – Catapres, Catapres-TTS". Medscape Drugs & Diseases.
- Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- "guanfacine (Rx) – Intuniv, Tenex". Medscape Drugs & Diseases.
- "amitriptyline (Rx) – Elavil, Levate". Medscape Drugs & Diseases.
- Guardiola, A; Terra, AR; Ferreira, LT; Londero, RG (September 1999). "[Use of amitriptyline in attention deficit hyperactivity disorder]". Arq Neuropsiquiatr (in Portuguese). 57 (3A): 599–605. doi:10.1590/S0004-282X1999000400010. PMID 10667283.
- "bupropion (Rx) – Wellbutrin, Zyban". Medscape Drugs & Diseases.
- Maneeton, N; Maneeton, B; Srisurapanont, M; Martin, SD (December 2011). "Bupropion for adults with attention-deficit hyperactivity disorder: Meta-analysis of randomized, placebo-controlled trials". Psychiatry and Clinical Neurosciences. 65 (7): 611–617. doi:10.1111/j.1440-1819.2011.02264.x. PMID 22176279.
- "buspirone (Rx) – BuSpar, Buspirex". Medscape Drugs & Diseases.
- Malhotra, S; Santosh, PJ (April 1998). "An open clinical trial of buspirone in children with attention-deficit/hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 37 (4): 364–371. doi:10.1097/00004583-199804000-00013. PMID 9549956.
- Mohammadi, MR; Hafezi, P; Galeiha, A; Hajiaghaee, R; Akhondzadeh, S (November 2012). "Buspirone versus Methylphenidate in the Treatment of Children with Attention- Deficit/ Hyperactivity Disorder: Randomized Double-Blind Study". Acta Medica Iranica. 50 (11): 723–728. PMID 23292622.
- Sutherland, SM; Adler, LA; Chen, C; Smith, MD; Feltner, DE (2012). "An 8-Week, Randomized Controlled Trial of Atomoxetine, Atomoxetine Plus Buspirone, or Placebo in Adults With ADHD". The Journal of Clinical Psychiatry. 73 (4): 445–450. doi:10.4088/JCP.10m06788. PMID 22313788.
- Davari-Ashtiani, R; Shahrbabaki, ME; Razjouyan, K; Amini, H; Mazhabdar, H (2010). "Buspirone Versus Methylphenidate in the Treatment of Attention Deficit Hyperactivity Disorder: A Double-Blind and Randomized Trial". Child Psychiatry and Human Development. 41 (6): 641–648. doi:10.1007/s10578-010-0193-2. PMID 20517641.
- Bortolozzi, A; Masana, M; Díaz-Mataix, L; Cortés, R; Scorza, MC; Gingrich, JA; Toth, M; Artigas, F (November 2010). "Dopamine release induced by atypical antipsychotics in prefrontal cortex requires 5-HT1A receptors but not 5-HT2A receptors". The International Journal of Neuropsychopharmacology. 13 (10): 1299–1314. doi:10.1017/S146114571000009X. PMC 6112770. PMID 20158933.
- Díaz-Mataix, L; Scorza, MC; Bortolozzi, A; Toth, M; Celada, P; Artigas, F (November 2005). "Involvement of 5-HT1A receptors in prefrontal cortex in the modulation of dopaminergic activity: role in atypical antipsychotic action". The Journal of Neuroscience. 25 (47): 10831–10843. doi:10.1523/JNEUROSCI.2999-05.2005. PMC 6725886. PMID 16306396.
- Garfinkel, BD; Wender, PH; Sloman, L; O'Neill, I (July 1983). "Tricyclic antidepressant and methylphenidate treatment of attention deficit disorder in children". Journal of the American Academy of Child Psychiatry. 22 (4): 343–8. doi:10.1016/s0002-7138(09)60669-5. PMID 6875128.
- "desipramine (Rx) – Norpramin". Medscape Drugs & Diseases.
- Otasowie, J; Castells, X; Ehimare, UP; Smith, CH (19 September 2014). "Tricyclic antidepressants for attention deficit hyperactivity disorder (ADHD) in children and adolescents". The Cochrane Database of Systematic Reviews. 9 (9): CD006997. doi:10.1002/14651858.CD006997.pub2. PMID 25238582.
- "duloxetine (Rx) – Cymbalta". Medscape Drugs & Diseases.
- Bilodeau, M; Simon, T; Beauchamp, MH; Lespérance, P; Dubreucq, S; Dorée, JP; Tourjman, SV (May 2012). "Duloxetine in Adults With ADHD: A Randomized, Placebo-Controlled Pilot Study". Journal of Attention Disorders. 18 (2): 169–75. doi:10.1177/1087054712443157. PMID 22582349.
- "imipramine (Rx) – Tofranil, Tofranil-PM". Medscape Drugs & Diseases.
- Biederman, J; Spencer, T (November 1999). "Attention-Deficit/Hyperactivity Disorder (ADHD) as a Noradrenergic Disorder". Biological Psychiatry. 46 (9): 1234–1242. doi:10.1016/S0006-3223(99)00192-4. PMID 10560028.
- "milnacipran (Rx) – Savella". Medscape Drugs & Diseases.
- Kako, Y; Niwa, Y; Toyomaki, A; Yamanaka, H; Kitagawa, N; Denda, K; Koyama, T (April 2007). "A case of adult attention-deficit/hyperactivity disorder alleviated by milnacipran". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 31 (3): 772–775. doi:10.1016/j.pnpbp.2006.12.017. PMID 17300859.
- Priest, R. G.; Gimbrett, R.; Roberts, M. and Steinert, J. (April 1995). "Reversible and selective inhibitors of monoamine oxidase A in mental and other disorders". Acta Psychiatrica Scandinavica. 91: 40–43. doi:10.1111/j.1600-0447.1995.tb05923.x. PMID 7717094.CS1 maint: uses authors parameter (link)
- "nortriptyline (Rx) – Pamelor, Aventyl". Medscape Drugs & Diseases.
- Wilens, TE; Biederman, J; Geist, DE; Steingard, R; Spencer, T (March 1993). "Nortriptyline in the treatment of ADHD: a chart review of 58 cases". Journal of the American Academy of Child and Adolescent Psychiatry. 32 (2): 343–349. doi:10.1097/00004583-199303000-00015. PMID 8444763.
- Spencer, T; Biederman, J; Wilens, T; Steingard, R; Geist, D (January 1993). "Nortriptyline treatment of children with attention-deficit hyperactivity disorder and tic disorder or Tourette's syndrome". Journal of the American Academy of Child and Adolescent Psychiatry. 32 (1): 205–210. doi:10.1097/00004583-199301000-00029. PMID 8428873.
- Ghanizadeh, A (May 2015). "A systematic review of reboxetine for treating patients with attention deficit hyperactivity disorder". Nordic Journal of Psychiatry. 69 (4): 241–8. doi:10.3109/08039488.2014.972975. PMID 25415763.
- Rubinstein, S; Malone, MA; Roberts, W; Logan, WJ (August 2006). "Placebo-controlled study examining effects of selegiline in children with attention-deficit/hyperactivity disorder". Journal of Child and Adolescent Psychopharmacology. 16 (4): 404–15. doi:10.1089/cap.2006.16.404. PMID 16958566.
- "venlafaxine (Rx) – Effexor, Effexor XR". Medscape Drugs & Diseases.
- Ahmad Ghanizadeh; Roger D. Freeman; Michael Berk (March 2013). "Efficacy and adverse effects of venlafaxine in children and adolescents with ADHD: a systematic review of non-controlled and controlled trials". Reviews on Recent Clinical Trials. 8 (1): 2–8. doi:10.2174/1574887111308010002. PMID 23157376.
- "amantadine (Rx) – Endantadine, Symmetrel". Medscape Drugs & Diseases.
- Mohammadi, MR; Kazemi, MR; Zia, E; Rezazadeh, SA; Tabrizi, M; Akhondzadeh, S (2010). "Amantadine versus methylphenidate in children and adolescents with attention deficit/hyperactivity disorder: a randomized, double-blind trial". Human Psychopharmacology. 25 (7–8): 560–565. doi:10.1002/hup.1154. PMID 21312290.
- "carbamazepine (Rx) – Tegretol, Equetro". Medscape Drugs & Diseases.
- Silva, RR; Munoz, DM; Alpert, M (March 1996). "Carbamazepine Use in Children and Adolescents with Features of Attention-Deficit Hyperactivity Disorder: A Meta-Analysis". Journal of the American Academy of Child and Adolescent Psychiatry. 35 (3): 352–358. doi:10.1097/00004583-199603000-00017. PMID 8714324.
- Popper, CW (July 2000). "Pharmacologic alternatives to psychostimulants for the treatment of attention-deficit/hyperactivity disorder". Child and Adolescent Psychiatric Clinics of North America. 9 (3): 605–46, viii. doi:10.1016/S1056-4993(18)30109-3. PMID 10944659.
- "memantine (Rx) – Namenda XR". Medscape Drugs & Diseases.
- Surman, CB; Hammerness, PG; Petty, C; Spencer, T; Doyle, R; Napolean, S; Chu, N; Yorks, D; Biederman, J (May 2013). "A pilot open label prospective study of memantine monotherapy in adults with ADHD". The World Journal of Biological Psychiatry. 14 (4): 291–298. doi:10.3109/15622975.2011.623716. PMID 22436083.
- Name, LM; Gameroff, M; Marcus, MJ; Jensen, SC; Jensen, PS. (2003). "National trends in the treatment of attention deficit hyperactivity disorder". American Journal of Psychiatry. 160 (6): 1071–1077. doi:10.1176/appi.ajp.160.6.1071. PMID 12777264.
- Visser, SN; Danielson, ML; Bitsko, RH; Holbrook, JR; Kogan, MD; Ghandour, RM; Perou, R; Blumberg, SJ (January 2014). "Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011". Journal of the American Academy of Child and Adolescent Psychiatry. 53 (1): 34–46.e2. doi:10.1016/j.jaac.2013.09.001. PMC 4473855. PMID 24342384.
- "Attention-Deficit / Hyperactivity Disorder: Data & Statistics". Centers for Disease Control and Prevention. 13 November 2013. Retrieved 6 September 2014.
- Singh, Ilina (2008). "Beyond polemics: science and ethics of ADHD" (PDF). Nature Reviews Neuroscience. 9 (12): 957–964. doi:10.1038/nrn2514. PMID 19020513.
- Greenhill, L.; Kollins, S.; Abikoff, H.; McCracken, J.; Riddle, M.; Swanson, J.; McGough, J.; Wigal, S.; et al. (November 2006). "Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD". J Am Acad Child Adolesc Psychiatry. 45 (11): 1284–93. doi:10.1097/01.chi.0000235077.32661.61. PMID 17023867.
- Freudenheim, Milt (17 May 2004). "Behavior Drugs Lead in Sales For Children". The New York Times. Retrieved 25 April 2010.
- "Medco Settles Fraud, Kickback Charges for $155 Million". ConsumerAffairs. Consumers Unified LLC. 24 October 2006. Retrieved 26 October 2013.
- Chung, Jaeah (2013). "Medication Management of Preschool ADHD by Pediatric Sub-Specialists: Non-Compliance with AAP Clinical Guidelines". Archived from the original on 28 May 2013. Retrieved 26 October 2013.
- Manos, Michael J (2006). "Treating Severe ADHD in Very Young Children". Medscape Psychiatry. 11 (1).
- Cortese, S; Holtmann, M; Banaschewski, T; Buitelaar, J; Coghill, D; Danckaerts, M; Dittmann, RW; Graham, J; Taylor, E; Sergeant, J; European ADHD Guidelines, Group (March 2013). "Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 54 (3): 227–46. doi:10.1111/jcpp.12036. PMID 23294014.
- Bhandari, Smitha. "Tips to Ease ADHD Drug Side Effects in Adults". WebMD. WebMD. Retrieved 16 October 2015.
- Gelperin, Kate (9 February 2006). "Studying Cardiovascular Risk with Drug Treatments of ADHD: Feasibility of Available Study Methods in Children and Adults" (PDF). Food and Drug Administration (US).
- Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, Murray KT, Quinn VP, Stein CM, Callahan ST, Fireman BH, Fish FA, Kirshner HS, O'Duffy A, Connell FA, Ray WA (November 2011). "ADHD drugs and serious cardiovascular events in children and young adults". N. Engl. J. Med. 365 (20): 1896–1904. doi:10.1056/NEJMoa1110212. PMC 4943074. PMID 22043968.
- "FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in adults". United States Food and Drug Administration. 15 December 2011. Retrieved 4 November 2013.
- Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, Arbogast PG, Cheetham TC, Quinn VP, Dublin S, Boudreau DM, Andrade SE, Pawloski PA, Raebel MA, Smith DH, Achacoso N, Uratsu C, Go AS, Sidney S, Nguyen-Huynh MN, Ray WA, Selby JV (December 2011). "ADHD medications and risk of serious cardiovascular events in young and middle-aged adults". JAMA. 306 (24): 2673–2683. doi:10.1001/jama.2011.1830. PMC 3350308. PMID 22161946.
- "FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in children and young adults". United States Food and Drug Administration. 20 December 2011. Retrieved 4 November 2013.
- "ADHD Drug Labels" (PDF). Food and Drug Administration (US). 2006.
- Silver, Larry (February 2006). "ADHD Medications: Say No to Side Effects". ADDitude magazine. New Hope Media LLC.
- Kraemer M, Uekermann J, Wiltfang J, Kis B (July 2010). "Methylphenidate-induced psychosis in adult attention-deficit/hyperactivity disorder: report of 3 new cases and review of the literature". Clin Neuropharmacol. 33 (4): 204–6. doi:10.1097/WNF.0b013e3181e29174. PMID 20571380.
- Wingo, AP; Ghaemi, SN (2008). "Frequency of stimulant treatment and of stimulant-associated mania/hypomania in bipolar disorder patients". Psychopharmacology Bulletin. 41 (4): 37–47. PMID 19015628.
- Kimko HC, Cross JT, Abernethy DR (December 1999). "Pharmacokinetics and clinical effectiveness of methylphenidate". Clin Pharmacokinet. 37 (6): 457–70. doi:10.2165/00003088-199937060-00002. PMID 10628897.
- Mosholder, Andrew D.; Gelperin, Kate (1 February 2009). "Hallucinations and Other Psychotic Symptoms Associated With the Use of Attention-Deficit/Hyperactivity Disorder Drugs in Children". Pediatrics. 123 (2): 611–616. doi:10.1542/peds.2008-0185. PMID 19171629. Retrieved 23 October 2013.
- Carvalho M, Carmo H, Costa VM, Capela JP, Pontes H, Remião F, Carvalho F, Bastos Mde L (August 2012). "Toxicity of amphetamines: an update". Arch. Toxicol. 86 (8): 1167–1231. doi:10.1007/s00204-012-0815-5. PMID 22392347.
- Berman S, O'Neill J, Fears S, Bartzokis G, London ED (2008). "Abuse of amphetamines and structural abnormalities in the brain". Ann. N. Y. Acad. Sci. 1141 (1): 195–220. Bibcode:2008NYASA1141..195B. doi:10.1196/annals.1441.031. PMC 2769923. PMID 18991959.
- Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K (February 2013). "Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects". JAMA Psychiatry. 70 (2): 185–198. doi:10.1001/jamapsychiatry.2013.277. PMID 23247506.
- Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, Faraone SV, Biederman J (September 2013). "Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies". J. Clin. Psychiatry. 74 (9): 902–917. doi:10.4088/JCP.12r08287. PMC 3801446. PMID 24107764.
- Frodl T, Skokauskas N (February 2012). "Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects". Acta Psychiatrica Scand. 125 (2): 114–126. doi:10.1111/j.1600-0447.2011.01786.x. PMID 22118249.
Basal ganglia regions like the right globus pallidus, the right putamen, and the nucleus caudatus are structurally affected in children with ADHD. These changes and alterations in limbic regions like ACC and amygdala are more pronounced in non-treated populations and seem to diminish over time from child to adulthood. Treatment seems to have positive effects on brain structure.
- Millichap JG (2010). "Chapter 3: Medications for ADHD". In Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York: Springer. pp. 111–113. ISBN 978-1-4419-1396-8.
- Huang YS, Tsai MH (July 2011). "Long-term outcomes with medications for attention-deficit hyperactivity disorder: current status of knowledge". CNS Drugs. 25 (7): 539–554. doi:10.2165/11589380-000000000-00000. PMID 21699268.
- Millichap JG (2010). "Chapter 3: Medications for ADHD". In Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York: Springer. pp. 121–123. ISBN 978-1-4419-1396-8.
- Fusar-Poli P, Rubia K, Rossi G, Sartori G, Balottin U (March 2012). "Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis". Am J Psychiatry. 169 (3): 264–72. doi:10.1176/appi.ajp.2011.11060940. PMID 22294258.
- Kooij, SJ.; Bejerot, S.; Blackwell, A.; Caci, H.; Casas-Brugué, M.; Carpentier, PJ.; Edvinsson, D.; Fayyad, J.; et al. (2010). "European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD". BMC Psychiatry. 10: 67. doi:10.1186/1471-244X-10-67. PMC 2942810. PMID 20815868.
- Brown, TE. (October 2008). "ADD/ADHD and Impaired Executive Function in Clinical Practice". Curr Psychiatry Rep. 10 (5): 407–11. doi:10.1007/s11920-008-0065-7. PMID 18803914.
- Garland EJ (1998). "Pharmacotherapy of adolescent attention deficit hyperactivity disorder: challenges, choices and caveats". J. Psychopharmacol. (Oxford). 12 (4): 385–95. doi:10.1177/026988119801200410. PMID 10065914.
- Nolan EE, Gadow KD, Sprafkin J (April 1999). "Stimulant medication withdrawal during long-term therapy in children with comorbid attention-deficit hyperactivity disorder and chronic multiple tic disorder". Pediatrics. 103 (4 Pt 1): 730–7. doi:10.1542/peds.103.4.730. PMID 10103294.
- Ackerman, Todd (1 July 2005). "Closer look for possible Ritalin, cancer link". Houston Chronicle. Retrieved 10 July 2011.
- Walitza, Susanne; et al. (June 2007). "Does Methylphenidate Cause a Cytogenetic Effect in Children with Attention Deficit Hyperactivity Disorder?". Environmental Health Perspectives. 115 (6): 936–940. doi:10.1289/ehp.9866. PMC 1892117. PMID 17589603.
- Lange, KW.; Reichl, S.; Lange, KM.; Tucha, L.; Tucha, O. (December 2010). "The history of attention deficit hyperactivity disorder". Atten Defic Hyperact Disord. 2 (4): 241–55. doi:10.1007/s12402-010-0045-8. PMC 3000907. PMID 21258430.
- Brown, Walter A. (July 1998). "Charles Bradley, M.D., 1902–1979". American Journal of Psychiatry. 155 (7): 968. doi:10.1176/ajp.155.7.968.
- "Straterra" (PDF). FDA. Retrieved 22 May 2019.
- "Vyvance Approval" (PDF). FDA. Retrieved 22 May 2019.
- "Vyvance". FDA. Retrieved 22 May 2019.
- "Sacklers quit Purdue Pharma board amid shifts for OxyContin maker". Stamford Advocate. 7 April 2019. Retrieved 22 May 2019.
- Schlander (2007). "Long-acting medications for the hyperkinetic disorders: a note on cost-effectiveness". European Child & Adolescent Psychiatry. 16 (7): 421–429 (Page:421). doi:10.1007/s00787-007-0615-2. PMID 17401606. Archived 14 October 2007 at the Wayback Machine
- Bader, A; Adesman, A (December 2012). "Complementary and alternative therapies for children and adolescents with ADHD". Current Opinion in Pediatrics. 24 (6): 760–9. doi:10.1097/mop.0b013e32835a1a5f. PMID 23111680.
- Sonuga-Barke, EJ; Brandeis, D; Cortese, S; Daley, D; Ferrin, M; Holtmann, M; Stevenson, J; Danckaerts, M; van der Oord, S; Döpfner, M; Dittmann, RW; Simonoff, E; Zuddas, A; Banaschewski, T; Buitelaar, J; Coghill, D; Hollis, C; Konofal, E; Lecendreux, M; Wong, IC; Sergeant, J; European ADHD Guidelines, Group (1 March 2013). "Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments". The American Journal of Psychiatry. 170 (3): 275–89. doi:10.1176/appi.ajp.2012.12070991. PMID 23360949.
- Greydanus, DE; Pratt, HD; Patel, DR (February 2007). "Attention deficit hyperactivity disorder across the lifespan: the child, adolescent, and adult". Disease-a-month. 53 (2): 70–131. doi:10.1016/j.disamonth.2007.01.001. PMID 17386306.
- Moriyama TS, Polanczyk G, Caye A, Banaschewski T, Brandeis D, Rohde LA (July 2012). "Evidence-based information on the clinical use of neurofeedback for ADHD". Neurotherapeutics. 9 (3): 588–98. doi:10.1007/s13311-012-0136-7. PMC 3441929. PMID 22930416.
- Lofthouse N, Arnold LE, Hurt E (October 2012). "Current status of neurofeedback for attention-deficit/hyperactivity disorder". Curr Psychiatry Rep. 14 (5): 536–42. doi:10.1007/s11920-012-0301-z. PMID 22890816.
- Holtmann, M; Sonuga-Barke, E; Cortese, S; Brandeis, D (October 2014). "Neurofeedback for ADHD: A Review of Current Evidence". Child and Adolescent Psychiatric Clinics of North America. 23 (4): 789–806. doi:10.1016/j.chc.2014.05.006. hdl:1854/LU-5841198. PMID 25220087.
- Jenks, Susan (9 March 2006). "ADHD patients play video games as part of treatment". USA Today.
- Butnik S.M. (2005). "Neurofeedback in adolescents and adults with attention deficit hyperactivity disorder". Journal of Clinical Psychology. 61 (5): 621–625. doi:10.1002/jclp.20124. PMID 15723361.
- Shaw R.; Grayson A.; Lewis V. (2000). "Inhibition, ADHD, and computer games: The inhibitory performance of children and ADHD on computerized tasks and games". Journal of Attention Disorders. 8 (4): 160–168. doi:10.1177/1087054705278771. PMID 16110046.
- Tolchinsky A.; Jefferson, S.D. (2011). "Problematic video game play in a college sample and its relationship to time management skills and Attention-Deficit/Hyperactivity disorder symptomology". Cyberpsychology, Behavior, and Social Networking. 14 (9): 489–496. doi:10.1089/cyber.2010.0315. PMID 21288135.
- Rojas, NL; Chan, E (2005). "Old and new controversies in the alternative treatment of attention-deficit hyperactivity disorder". Mental Retardation and Developmental Disabilities Research Reviews. 11 (2): 116–30. doi:10.1002/mrdd.20064. PMID 15977318.
- Wolraich, ML; Hagan JF, Jr; Allan, C; Chan, E; Davison, D; Earls, M; Evans, SW; Flinn, SK; Froehlich, T; Frost, J; Holbrook, JR; Lehmann, CU; Lessin, HR; Okechukwu, K; Pierce, KL; Winner, JD; Zurhellen, W; SUBCOMMITTEE ON CHILDREN AND ADOLESCENTS WITH ATTENTION-DEFICIT/HYPERACTIVE, DISORDER. (October 2019). "Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents". Pediatrics. 144 (4). doi:10.1542/peds.2019-2528. PMID 31570648.
- Schnoll R, Burshteyn D, Cea-Aravena J (March 2003). "Nutrition in the treatment of attention-deficit hyperactivity disorder: a neglected but important aspect". Applied Psychophysiology and Biofeedback. 28 (1): 63–75. doi:10.1023/A:1022321017467. PMID 12737097.
- Krummel DA, Seligson FH, Guthrie HA (1996). "Hyperactivity: is candy causal?". Critical Reviews in Food Science and Nutrition. 36 (1–2): 31–47. doi:10.1080/10408399609527717. PMID 8747098.
- Nigg JT, Lewis K, Edinger T, Falk M (January 2012). "Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives". J Am Acad Child Adolesc Psychiatry. 51 (1): 86–97.e8. doi:10.1016/j.jaac.2011.10.015. PMC 4321798. PMID 22176942.
- "Food coloring ban in the UK but usage continues for USA". BioHealthBase BRC Team. 23 October 2014.
- "Modernising the Rules on Food Additives and Labelling of Azo Dyes". FLEXNEWS: Business News for the Food Industry. Global Data Systems. 9 July 2008.
- Kleinman RE, Brown RT, Cutter GR, Dupaul GJ, Clydesdale FM (June 2011). "A research model for investigating the effects of artificial food colorings on children with ADHD". Pediatrics. 127 (6): e1575–84. doi:10.1542/peds.2009-2206. PMID 21576306.
- "Diet and attention deficit hyperactivity disorder". Harvard Mental Health Letter. 25 (12): 4–5. June 2009. PMID 19582942.
- "FDA Asks Attention-Deficit Hyperactivity Disorder (ADHD) Drug Manufacturers to Develop Patient Medication Guides". Food and Drug Administration. 21 September 2007. Archived from the original on 21 February 2008. Retrieved 13 April 2009.
- Ioannidis, K; Chamberlain, SR; Müller, U (September 2014). "Ostracising caffeine from the pharmacological arsenal for attention-deficit hyperactivity disorder—was this a correct decision? A literature review". Journal of Psychopharmacology (Oxford, England). 28 (9): 830–6. doi:10.1177/0269881114541014. PMID 24989644.
- Schechter, MD; Timmons, GD (1985). "Objectively measured hyperactivity—II. Caffeine and amphetamine effects". Journal of Clinical Pharmacology. 25 (4): 276–80. Bibcode:1991JClP...31..928S. doi:10.1002/j.1552-4604.1985.tb02838.x. PMID 4008672.
- Toledano A, Alvarez MI, Toledano-Díaz A (September 2010). "Diversity and variability of the effects of nicotine on different cortical regions of the brain – therapeutic and toxicological implications". Cent Nerv Syst Agents Med Chem. 10 (3): 180–206. doi:10.2174/1871524911006030180. hdl:10261/61750. PMID 20528766.
- McClernon, FJ; Kollins, SH (October 2008). "ADHD and smoking: from genes to brain to behavior". Annals of the New York Academy of Sciences. 1141 (1): 131–47. Bibcode:2008NYASA1141..131M. doi:10.1196/annals.1441.016. PMC 2758663. PMID 18991955.
- Potter, AS; Schaubhut, G; Shipman, M (December 2014). "Targeting the nicotinic cholinergic system to treat attention-deficit/hyperactivity disorder: rationale and progress to date". CNS Drugs. 28 (12): 1103–13. doi:10.1007/s40263-014-0208-9. PMC 4487649. PMID 25349138.
- Gillies D, Sinn JK, Lad SS, Leach MJ, Ross MJ (2012). "Polyunsaturated fatty acids (PUFA) for attention deficit hyperactivity disorder (ADHD) in children and adolescents". Cochrane Database Syst Rev. 7 (7): CD007986. doi:10.1002/14651858.CD007986.pub2. PMC 6599878. PMID 22786509.
- Bloch MH, Qawasmi A (October 2011). "Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis". J Am Acad Child Adolesc Psychiatry. 50 (10): 991–1000. doi:10.1016/j.jaac.2011.06.008. PMC 3625948. PMID 21961774.
- Arnold LE, DiSilvestro RA (2005). "Zinc in attention-deficit/hyperactivity disorder". Journal of Child and Adolescent Psychopharmacology. 15 (4): 619–27. doi:10.1089/cap.2005.15.619. hdl:1811/51593. PMID 16190793.
- Bloch, MH; Mulqueen, J (October 2014). "Nutritional supplements for the treatment of ADHD". Child and Adolescent Psychiatric Clinics of North America. 23 (4): 883–97. doi:10.1016/j.chc.2014.05.002. PMC 4170184. PMID 25220092.
- Haslam RH, Dalby JT, Rademaker AW (1984). "Effects of megavitamin therapy on children with attention deficit disorders". Pediatrics. 74 (1): 103–111. PMID 6234505.
- Sukhodolsky DG, Scahill L, Zhang H, et al. (January 2003). "Disruptive behavior in children with Tourette's syndrome: association with ADHD comorbidity, tic severity, and functional impairment". J Am Acad Child Adolesc Psychiatry. 42 (1): 98–105. doi:10.1097/00004583-200301000-00016. PMID 12500082.
Hoekstra PJ, Steenhuis MP, Troost PW, et al. (August 2004). "Relative contribution of attention-deficit hyperactivity disorder, obsessive-compulsive disorder, and tic severity to social and behavioral problems in tic disorders". J Dev Behav Pediatr. 25 (4): 272–9. doi:10.1097/00004703-200408000-00007. PMID 15308928.
Carter AS, O'Donnell DA, Schultz RT, et al. (February 2000). "Social and emotional adjustment in children affected with Gilles de la Tourette's syndrome: associations with ADHD and family functioning. Attention Deficit Hyperactivity Disorder". J Child Psychol Psychiatry. 41 (2): 215–23. doi:10.1111/1469-7610.00602. PMID 10750547.
Spencer T, Biederman J, Harding M, O'Donnell D, Wilens T, Faraone S, Coffey B, Geller D (October 1998). "Disentangling the overlap between Tourette's disorder and ADHD". J Child Psychol Psychiatry. 39 (7): 1037–44. doi:10.1111/1469-7610.00406. PMID 9804036. - Freeman, Roger D. "Tourette's Syndrome: minimizing confusion". Archived from the original on 11 April 2006. Retrieved 8 February 2006. RD Freeman, MD, is Clinic Head of Neuropsychiatry Clinic at British Columbia Children's Hospital, Vancouver, professional advisory board member of Tourette Syndrome Foundation of Canada, and former member of the Tourette Syndrome Association Medical Advisory Board. Freeman has over 180 journal-published articles on PubMed.
- Palumbo D, Spencer T, Lynch J, Co-Chien H, Faraone SV (Summer 2004). "Emergence of tics in children with ADHD: impact of once-daily OROS methylphenidate therapy". Journal of Child and Adolescent Psychopharmacology. 14 (2): 185–94. doi:10.1089/1044546041649138. PMID 15319016.
Kurlan R (July 2003). "Tourette's syndrome: are stimulants safe?". Current Neurology and Neuroscience Reports. 3 (4): 285–8. doi:10.1007/s11910-003-0004-2. PMID 12930697.
Law SF, Schachar RJ (August 1999). "Do typical clinical doses of methylphenidate cause tics in children treated for attention-deficit hyperactivity disorder?". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (8): 944–51. doi:10.1097/00004583-199908000-00009. PMID 10434485. - Tourette's Syndrome Study Group (February 2002). "Treatment of ADHD in children with tics: a randomized controlled trial". Neurology. 58 (4): 527–36. doi:10.1212/WNL.58.4.527. PMID 11865128.
- Pringsheim, T; Steeves, T (13 April 2011). "Pharmacological treatment for Attention Deficit Hyperactivity Disorder (ADHD) in children with comorbid tic disorders". The Cochrane Database of Systematic Reviews (4): CD007990. doi:10.1002/14651858.CD007990.pub2. PMID 21491404.
- Zinner SH (November 2000). "Tourette disorder". Pediatrics in Review. 21 (11): 372–83. doi:10.1542/pir.21-11-372. PMID 11077021.
- Scahill L, Erenberg G, Berlin CM, Budman C, Coffey BJ, Jankovic J, Kiessling L, King RA, Kurlan R, Lang A, Mink J, Murphy T, Zinner S, Walkup J (April 2006). Tourette Syndrome Association Medical Advisory Board: Practice Committee. "Contemporary assessment and pharmacotherapy of Tourette syndrome". NeuroRx. 3 (2): 192–206. doi:10.1016/j.nurx.2006.01.009. PMC 3593444. PMID 16554257.
External links
