Artesunate
Artesunate (AS) is a medication used to treat malaria.[3][4] The intravenous form is preferred to quinidine for severe malaria.[3] Often it is used as part of combination therapy, such as artesunate plus mefloquine.[4] It is not used for the prevention of malaria.[4] Artesunate can be given by injection into a vein, injection into a muscle, by mouth, and by rectum.[4][5][6]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | ahr-tez′ŭ-nāt[1] |
| Trade names | many[2] |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | by mouth, intravenous, intramuscular |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number |
|
| PubChem CID | |
| ChemSpider | |
| UNII | |
| ChEMBL | |
| NIAID ChemDB | |
| PDB ligand | |
| ECHA InfoCard | 100.106.898 |
| Chemical and physical data | |
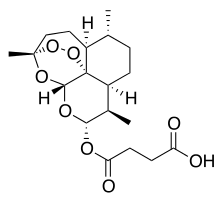
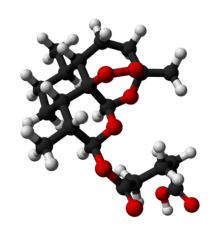
| Formula | C19H28O8 |
| Molar mass | 384.421 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Artesunate is generally well tolerated.[5] Side effects may include a slow heartbeat, allergic reaction, dizziness, and low white blood cell levels.[4] During pregnancy it appears to be a safer option, even though animal studies have found harm to the baby.[7] Use is likely okay during breastfeeding.[8] It is in the artemisinin class of medication.[3]
Artesunate was developed by Liu Xu in 1977.[9] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[10] The wholesale cost in the developing world is US$2.09 to US$2.57 a dose.[11] It is not commercially available in the United States; however, it can be obtained via the Centers for Disease Control.[3][12] It was originally made from the sweet wormwood plant.[3]
Medical uses
Artesunate is the first line treatment for children or adults with severe malaria,[13][12] usually in combination with another antimalarial drug. There is moderate-quality evidence that treatment with artesunate plus mefloquine is superior to treatment with artesunate plus amodiaquine or artesunate plus sulfadoxine-pyrimethamine.[14] Artemisinin-based combination therapy may be used by mouth in persons that can tolerate it after 24 hours by injection. In facilities where long-term care is not appropriate, initial treatment with artesunate may be given as a single intramuscular injection or by rectal route (children < 6 years) prior to transferring care to a higher level facility.
Artesunate is preferred over parenteral quinine for severe malaria treatment.[3] Artesunate was shown to prevent more deaths from severe malaria than quinine in two large multicentre randomized controlled trials from Africa[15] and Asia.[16] A subsequent systematic review of seven randomized controlled trials found this improvement in survival rates to be consistent across all trials.[17]
Artesunate is also used to treat less severe forms of malaria when it can be given orally.[13] It has activity against P. ovale, P. malariae, and severe P. knowlesi.[13]
Artesunate + sulfadoxine/pyrimethamine for treatment of P. vivax is not recommended due to high rates of resistance.
While artesunate is used primarily as treatment for malaria, there is some evidence that it may also have some beneficial effects in Schistosoma haematobium infection,[18] but has not been evaluated in large randomized trials.
Although not FDA-approved for use in the United States, artesunate is used as the treatment of choice for severe malaria by the World Health Organization (WHO) over quinidine.[3]
Pregnancy
When given in the second or third trimesters of pregnancy, no artesunate-related adverse pregnancy outcomes have been reported.[19] However, there is insufficient evidence regarding the safety of artesunate use in the first trimester of pregnancy. The WHO recommends that artesunate use for severe malaria in the first trimester should be based on the individual risks versus benefits. In absence of other viable treatment options, artesunate may be used.
Children
Artesunate is safe for use in children. Artesunate + sulfadoxine/pyrimethamine should be avoided in the newborns due to sulfadoxine/pyrmethamine effects on bilirubin.[13] Parenteral artesunate dosing for treatment of severe malaria in children less than 20 kg should be higher than that of adults in order to increase exposure.[13] When artesunate cannot be given orally or intramuscularly due to an individual's weakness or inability to swallow, rectal administration may be given as pre-referral treatment as long as parenteral administration is initiated after transfer to a more advanced facility.
Adverse effects
Artesunate is generally safe and well-tolerated. Artesunate-based regimens are less likely to cause vomiting and tinnitus than quinine plus anti-malarial antibiotic therapy.[20] The best recognised adverse effect of the artemisinins is that they lower reticulocyte counts.[21] This is not usually of clinical relevance.
With increased use of I.V. artesunate, there have been reports of post-artesunate delayed haemolysis (PADH).[22] Delayed haemolysis (occurring around two weeks after treatment) has been observed in patients treated with artesunate for severe malaria.[23]
Contraindications
Artesunate is typically a well tolerated medicine. Known contraindications include a previous severe allergic reaction to artesunate.[24]
Drugs that should be avoided while on artesunate are the drugs that inhibit the liver enzyme CYP2A6. These drugs include amiodarone, desipramine, isoniazid, ketoconazole, letrozole, methoxsalen, tranylcypromine.[25]
Mechanisms of action
The mechanisms of action of artesunate remains unclear and debatable. Artesunate is a prodrug that is rapidly converted to its active form dihydroartemisinin (DHA). This process involves hydrolysis of the 4-carbon ester group via plasma esterase enzyme.[26] It is hypothesized that the cleavage of endoperoxide bridge in the pharmacophore of DHA generates reactive oxygen species (ROS), which increases oxidative stress and causes malarial protein damage via alkylation.[26] In addition, Artesunate potently inhibits the essential Plasmodium falciparum exported protein 1 (EXP1), a membrane glutathione S-transferase.[27] As a result, the amount of glutathione in the parasite is reduced.
In 2016, artemisinin has been shown to bind to a large number targets, suggesting that it acts in a promiscuous manner.[28] There is evidence suggesting DHA inhibition of calcium-dependent ATPase on endoplasmic membrane, which disrupts protein folding of parasites.[26]
Pharmacokinetics
In infected individuals, the elimination half-life of artesunate is about 0.22 hours. Its active metabolite, DHA, has a slightly longer half-life of 0.34 hours. Overall, the average half-life ranges from 0.5 to 1.5 hours.[29] Because of its short half-life, its use in malaria prevention is limited.[26]
DHA is metabolized to an inactive metabolite by the liver enzymes CYP2B6, CYP2C19, and CYP3A4.[30]
Chemical synthesis
Artesunate is made from dihydroartemisinin (DHA) by reacting it with succinic acid anhydride in a basic medium. It is one of many semi-synthetic derivatives from Artemisinin that is water-soluble.[31]
Research
In 2007, the FDA approved an Investigational New Drug (IND) protocol for intravenous artesunate.
Artesunate is under study for the treatment of cancer.[32]
References
- "Artesunate definition | Drugs.com". www.drugs.com. Archived from the original on 20 December 2016. Retrieved 7 December 2016.
- "Artesunate - Drugs.com". www.drugs.com. Archived from the original on 20 December 2016. Retrieved 7 December 2016.
- Prevention, CDC - Centers for Disease Control and. "CDC - Malaria - Diagnosis & Treatment (United States) - Treatment (U.S.) - Artesunate". www.cdc.gov. Archived from the original on 2016-10-29. Retrieved 2016-10-28.
- "Artesunate" (PDF). World Health Organization. March 2013. Archived (PDF) from the original on 28 December 2013. Retrieved 7 December 2016.
- Rosenthal, Philip J. (24 April 2008). "Artesunate for the Treatment of Severe Falciparum Malaria". New England Journal of Medicine. 358 (17): 1829–1836. doi:10.1056/NEJMct0709050. PMID 18434652.
- "Rectal artesunate for pre-referral treatment of severe malaria" (PDF). WHO. October 2018. Retrieved 22 February 2019.
- Kovacs, SD; Rijken, MJ; Stergachis, A (February 2015). "Treating severe malaria in pregnancy: a review of the evidence". Drug Safety. 38 (2): 165–81. doi:10.1007/s40264-014-0261-9. PMC 4328128. PMID 25556421.
- "Artesunate use while Breastfeeding | Drugs.com". www.drugs.com. Archived from the original on 20 December 2016. Retrieved 7 December 2016.
- Li, Guoqiao; Li, Ying; Li, Zelin; Zeng, Meiyi (2017-11-28). Artemisinin-Based and Other Antimalarials: Detailed Account of Studies by Chinese Scientists Who Discovered and Developed Them. Academic Press. ISBN 9780128132111.
- "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- "Artesunate". International Drug Price Indicator Guide. Retrieved 1 January 2016.
- "CDC: Artesunate Now First-Line Treatment for Severe Malaria in the United States | CDC Online Newsroom | CDC". www.cdc.gov. 28 March 2019. Retrieved 6 April 2019.
- Guidelines for treatment of malaria (3 ed.). Geneva: World Health Organization. 2015 – via https://www.ncbi.nlm.nih.gov/books/NBK294440/.
- Peixoto HM, Marchesini PB, de Oliveira MR (December 2016). "Efficacy and safety of artesunate-mefloquine therapy for treating uncomplicated Plasmodium falciparum malaria: systematic review and meta-analysis". Trans. R. Soc. Trop. Med. Hyg. doi:10.1093/trstmh/trw077. PMID 28039388.
- Dondorp AL; et al. (2010). "Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial". The Lancet. 376 (9753): 1647–1657. doi:10.1016/S0140-6736(10)61924-1. PMC 3033534. PMID 21062666.
- South East Asian Quinine Artesunate Malaria Trial (SEAQUAMAT) (2005). "Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial". The Lancet. 366 (9487): 717–725. doi:10.1016/S0140-6736(05)67176-0. PMID 16125588.
- Sinclair, D; Donegan, S; Isba, R; Lalloo, DG (Jun 13, 2012). "Artesunate versus quinine for treating severe malaria". The Cochrane Database of Systematic Reviews. 6 (6): CD005967. doi:10.1002/14651858.CD005967.pub4. PMC 6532684. PMID 22696354.
- Boulangier D, Dieng Y, Cisse B, et al. (2007). "Antischistosomal efficacy of artesunate combination therapies administered as curative treatments for malaria attacks" (PDF). Trans R Soc Trop Med Hyg. 101 (2): 113–16. doi:10.1016/j.trstmh.2006.03.003. PMID 16765398.
- WHO (2007). Assessment of the safety of artemisinin compounds in pregnancy Archived 2010-04-14 at the Wayback Machine. World Health Organization, Geneva.
- Song T, Chen J, Huang L, Gan W, Yin H, Jiang J, He T, Huang H, Hu X (March 2016). "Should we abandon quinine plus antibiotic for treating uncomplicated falciparum malaria? A systematic review and meta-analysis of randomized controlled trials". Parasitol. Res. 115 (3): 903–12. doi:10.1007/s00436-015-4842-z. PMID 26661109.
- Clark RL (2012). "Effects of artemisinins on reticulocyte count and relationship to possible embryotoxicity in confirmed and unconfirmed malarial patients". Birth Defects Research. Part A, Clinical and Molecular Teratology. 94 (2): 61–75. doi:10.1002/bdra.22868. PMID 22125126.
- Boillat O, Spechbach H, Chalandon Y, Eperon (2015). "Post-artesunate delayed haemolysis ‒ report of four cases and review of the literature". Swiss Medical Weekly. 145 (4546): w14181. doi:10.4414/smw.2015.14181. PMID 26524733.
- Rolling T, Agbenyega T, Issifou S, et al. (2013). "Delayed hemolysis after treatment with parenteral artesunate in African children with severe malaria—a double-center prospective study". J Infect Dis. 209 (12): 1921–8. doi:10.1093/infdis/jit841. PMID 24376273.
- Hess, Karl M.; Goad, Jeffery A.; Arguin, Paul M. (2010-01-01). "Intravenous Artesunate for Severe Malaria". Ann Pharmacother. 44 (7–8): 1250–1258. doi:10.1345/aph.1M732. PMID 20551300. Archived from the original on 2016-11-10.
- "Artesunate Amodiaquine Winthrop (artesunate, amodiaquine) [summary of product characteristics]" (PDF). Sanofi-Aventis. Archived (PDF) from the original on 2016-10-24.
- Cui, Liwang; Su, Xin-zhuan (2009-10-01). "Discovery, mechanisms of action and combination therapy of artemisinin". Expert Review of Anti-infective Therapy. 7 (8): 999–1013. doi:10.1586/eri.09.68. ISSN 1478-7210. PMC 2778258. PMID 19803708.
- Lisewski, A. M.; Quiros, J. P.; Ng, C. L.; Adikesavan, A. K.; Miura, K; Putluri, N; Eastman, R. T.; Scanfeld, D; Regenbogen, S. J.; Altenhofen, L; Llinás, M; Sreekumar, A; Long, C; Fidock, D. A.; Lichtarge, O (2014). "Supergenomic Network Compression and the Discovery of EXP1 as a Glutathione Transferase Inhibited by Artesunate". Cell. 158 (4): 916–28. doi:10.1016/j.cell.2014.07.011. PMC 4167585. PMID 25126794.
- Wang J, Zhang CJ, Chia WN, Loh CC, Li Z, Lee YM, He Y, Yuan LX, Lim TK, Liu M, Liew CX, Lee YQ, Zhang J, Lu N, Lim CT, Hua ZC, Liu B, Shen HM, Tan KS, Lin Q (2015). "Haem-activated promiscuous targeting of artemisinin in Plasmodium falciparum". Nature Communications. 6: 10111. Bibcode:2015NatCo...610111W. doi:10.1038/ncomms10111. PMC 4703832. PMID 26694030.
- Morris, Carrie A.; Duparc, Stephan; Borghini-Fuhrer, Isabelle; Jung, Donald; Shin, Chang-Sik; Fleckenstein, Lawrence (2011-01-01). "Review of the clinical pharmacokinetics of artesunate and its active metabolite dihydroartemisinin following intravenous, intramuscular, oral or rectal administration". Malaria Journal. 10: 263. doi:10.1186/1475-2875-10-263. ISSN 1475-2875. PMC 3180444. PMID 21914160.
- Hess, Karl M.; Goad, Jeffery A.; Arguin, Paul M. (2010-07-01). "Intravenous Artesunate for the Treatment of Severe Malaria". Annals of Pharmacotherapy. 44 (7–8): 1250–1258. doi:10.1345/aph.1M732. ISSN 1060-0280. PMID 20551300.
- "World of Chemicals – online chemical directory, chemistry portal, articles, news". www.worldofchemicals.com. Archived from the original on 2016-11-10. Retrieved 2016-11-10.
- "Intervention Dynamic Trial Listing Page". National Cancer Institute. 2017-06-13.