Eosinophilic esophagitis
Eosinophilic esophagitis (EoE, also spelled eosinophilic oesophagitis), also known as allergic oesophagitis, is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. Symptoms are swallowing difficulty, food impaction, vomiting, and heartburn.[1]
| Eosinophilic esophagitis | |
|---|---|
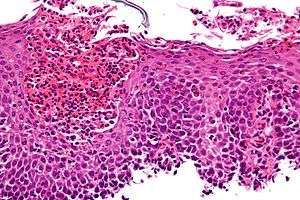 | |
| Micrograph showing eosinophilic esophagitis. H&E stain. | |
| Specialty | Gastroenterology |
Eosinophilic esophagitis was first described in children but also occurs in adults. The condition is not well understood, but food allergy may play a significant role.[2] The treatment may consist of removal of known or suspected triggers and medication to suppress the immune response. In severe cases, it may be necessary to enlarge the esophagus with an endoscopy procedure.
Signs and symptoms
EoE often presents with difficulty swallowing, food impaction, regurgitation or vomiting, and decreased appetite. In addition, young children with EoE may present with feeding difficulties and poor weight gain. It is more common in males, and affects both adults and children.[1]
Many people with EoE have other autoimmune and allergic diseases such as asthma[1] and celiac disease.[3] Mast cell disorders such as Mast Cell Activation Syndrome or Mastocytosis are also frequently associated with it.
Pathophysiology
EoE is a relatively poorly understood disease of which awareness is rising.
At a tissue level, EoE is characterized by a dense infiltrate with white blood cells of the eosinophil type into the epithelial lining of the esophagus. This is thought to be an allergic reaction against ingested food, based on the important role eosinophils play in allergic reactions. Eosinophils are inflammatory cells that release a variety of chemical signals which inflame the surrounding esophageal tissue. This results in the signs and symptoms of pain, visible redness on endoscopy, and a natural history that may include stricturing.[1]
Diagnosis


The diagnosis of EoE is typically made on the combination of symptoms and findings on diagnostic testing.[1]
Prior to the development of the EE Diagnostic Panel, EoE could only be diagnosed if gastroesophageal reflux did not respond to a six-week trial of twice-a-day high-dose proton-pump inhibitors (PPIs) or if a negative ambulatory pH study ruled out gastroesophageal reflux disease (GERD).[4][5]
Endoscopically, ridges, furrows, or rings may be seen in the esophageal wall. Sometimes, multiple rings may occur in the esophagus, leading to the term "corrugated esophagus" or "feline esophagus" due to similarity of the rings to the cat esophagus. Presence of white exudates in esophagus is also suggestive of the diagnosis.[6] On biopsy taken at the time of endoscopy, numerous eosinophils can be seen in the superficial epithelium. A minimum of 15 eosinophils per high-power field are required to make the diagnosis. Eosinophilic inflammation is not limited to the esophagus alone, and does extend through the whole gastrointestinal tract. Profoundly degranulated eosinophils may also be present, as may microabcesses and an expansion of the basal layer.[1][4]
Radiologically, the term "ringed esophagus" has been used for the appearance of eosinophilic esophagitis on barium swallow studies to contrast with the appearance of transient transverse folds sometimes seen with esophageal reflux (termed "feline esophagus").[7]
Treatment
Treatment strategies may include medication, dietary modification to exclude food allergens, and mechanical dilatation of the esophagus.
Dietary treatment can be effective, as there does appear to be a role of allergy in the development of EOE. Allergy testing is not particularly effective in predicting which foods are driving the disease process. Various approaches have been tried, where either six food groups (cow's milk, wheat, egg, soy, nuts and fish/seafood), four groups (animal milk, gluten-containing cereals, egg, legumes) or two groups (animal milk and gluten-containing cereals) are excluded for a period of time, usually six weeks. Endoscopy is required to measure the response to the dietary measure. A "top down" (starting with six foods, then reintroducing) approach may be very restrictive. Four- or even two-group exclusion diets may be less difficult to follow and reduce the need for many endoscopies if the response to the limited restriction is good.[8]
Endoscopic dilatation is sometimes required if there is significant narrowing of the esophagus. This is effective in 84% of people who require this procedure.[9]
See also
References
- Nurko, Samuel; Furuta, G T (2006). "Eosinophilic esophagitis". GI Motility Online. doi:10.1038/gimo49 (inactive 2019-12-05).
- Blanchard C, Rothenberg ME (January 2008). "Basic pathogenesis of eosinophilic esophagitis". Gastrointestinal Endoscopy Clinics of North America. 18 (1): 133–43, x. doi:10.1016/j.giec.2007.09.016. PMC 2194642. PMID 18061107.
- Stewart MJ, Shaffer E, Urbanski SJ, Beck PL, Storr MA (1 January 2013). "The association between celiac disease and eosinophilic esophagitis in children and adults". BMC Gastroenterology. 13 (1): 96. doi:10.1186/1471-230X-13-96. PMC 3682941. PMID 23721294.
- Noel RJ, Putnam PE, Rothenberg ME (August 2004). "Eosinophilic esophagitis". The New England Journal of Medicine. 351 (9): 940–1. doi:10.1056/NEJM200408263510924. PMID 15329438.
- Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, Bonis P, Hassall E, Straumann A, Rothenberg ME, First International Gastrointestinal Eosinophil Research Symposium Subcommittees (October 2007). "Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment". Gastroenterology. 133 (4): 1342–63. doi:10.1053/j.gastro.2007.08.017. PMID 17919504.
- Samadi F, Levine MS, Rubesin SE, Katzka DA, Laufer I (April 2010). "Feline esophagus and gastroesophageal reflux". AJR. American Journal of Roentgenology. 194 (4): 972–6. doi:10.2214/AJR.09.3352. PMID 20308499.
- Zimmerman SL, Levine MS, Rubesin SE, Mitre MC, Furth EE, Laufer I, Katzka DA (July 2005). "Idiopathic eosinophilic esophagitis in adults: the ringed esophagus". Radiology. 236 (1): 159–65. doi:10.1148/radiol.2361041100. PMID 15983073.
- Molina-Infante, J; Gonzalez-Cordero, PL; Arias, A; Lucendo, AJ (February 2017). "Update on dietary therapy for eosinophilic esophagitis in children and adults". Expert Review of Gastroenterology & Hepatology. 11 (2): 115–123. doi:10.1080/17474124.2017.1271324. PMID 27998193.
- Moole, Harsha; Jacob, Kavitha; Duvvuri, Abhiram; Moole, Vishnu; Dharmapuri, Sowmya; Boddireddy, Raghuveer; Uppu, Achuta; Puli, Srinivas R. (April 2017). "Role of endoscopic esophageal dilation in managing eosinophilic esophagitis". Medicine. 96 (14): e5877. doi:10.1097/MD.0000000000005877. PMC 5411180. PMID 28383396.
External links
- CURED Foundation - Non-Profit for EGID Research
- American Partnership for Eosinophilic Disorders
- Families Affected By Eosinophilic Disorders
- Canadian Council of Eosinophilic Disorders
- Australian Support for Eosinophilic Disorders
- AEDESEO Asociación Espanola de Esofagitis Eosinofílica
| Classification | |
|---|---|
| External resources |