Arteriovenous fistula
An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein.[1] It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm.[2]
| Arteriovenous fistula | |
|---|---|
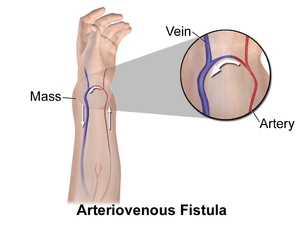 | |
| Illustration of an arteriovenous fistula | |
| Specialty | Cardiology |
Presentation
Associated conditions
Complications
Just like berry aneurysm, an intracerebral arteriovenous fistula can rupture causing subarachnoid hemorrhage.[3]
Causes
- Congenital (developmental defect)
- Rupture of arterial aneurysm into an adjacent vein
- Penetrating injuries
- Inflammatory necrosis of adjacent vessels
- Intentionally created (for example, Cimino fistula as vascular access for hemodialysis). Blood must be aspirated from the body of the patient, and since arteries are not easy to reach compared to the veins, blood may be aspirated from veins. The problem is that the walls of the veins are thin compared to those of the arteries. The AV fistula is the solution for this problem because, after 4-6 weeks, the walls of the veins become thicker due to the high arterial pressure. Thus, this vein can now tolerate needles during hemodialysis sessions.
Mechanism
When an arteriovenous fistula is formed involving a major artery like the abdominal aorta, it can lead to a large decrease in peripheral resistance. This lowered peripheral resistance causes the heart to increase cardiac output to maintain proper blood flow to all tissues. The physical manifestations of this typically consist of a relatively normal systolic blood pressure accompanied by decreased diastolic blood pressure, resulting in a wider pulse pressure.
Normal blood flow in the brachial artery is 85 to 110 milliliters per minute (mL/min). After the creation of a fistula, the blood flow increases to 400–500 mL/min immediately, and 700–1,000 mL/min within 1 month. A brachiocephalic fistula above the elbow has a greater flow rate than a radiocephalic fistula at the wrist. Both the artery and the vein dilate and elongate in response to the greater blood flow and shear stress, but the vein dilates more and becomes "arterialized". In one study, the cephalic vein increased from 2.3 mm to 6.3 mm diameter after 2 months. When the vein is large enough to allow cannulation, the fistula is defined as "mature".[4]
An arteriovenous fistula can increase preload.[5] AV shunts also decrease the afterload of the heart. This is because the blood bypasses the arterioles which results in a decrease in the total peripheral resistance (TPR). AV shunts increase both the rate and volume of blood returning to the heart.
See also
References
- "Arteriovenous Fistulas: Background, Pathophysiology, Etiology". 2017-01-07. Cite journal requires
|journal=(help) - "Arteriovenous fistula - Symptoms and causes". Mayo Clinic. Retrieved 2019-12-05.
- Park, Myung K. (2002). Pediatric cardiology for practitioners. With a contribution by R. George Troxler (4th ed.). St. Louis: Mosby. ISBN 978-0-323-01444-1.
- Vascular, Vol. 14, Supl. 1, Nov. 2006, p. S1
- "Pulmonary: Heart Failure". Archived from the original on 1 February 2009. Retrieved 2008-12-21.
External links
| Classification | |
|---|---|
| External resources |