AMPT
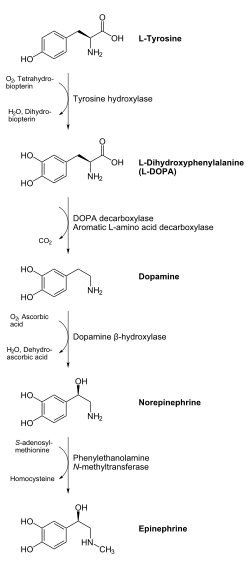
Alpha-methyl-p-tyrosine (AMPT) is a tyrosine hydroxylase enzyme inhibitor. Alpha-methyl-p-tyrosine (AMPT) is a non-endogenous drug involved in the catecholamine biosynthetic pathway.[1] AMPT inhibits tyrosine hydroxylase whose enzymatic activity is regulated through the phosphorylation of different serine residue regulatory domain sites.[1] Catecholamine biosynthesis starts with dietary tyrosine, which is hydroxylated by the enzyme tyrosine hydroxylase. It is hypothesized that AMPT competes with tyrosine at the tyrosine-binding site, causing inhibition of tyrosine hydroxylase.[2]
 | |
| Identifiers | |
|---|---|
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| ECHA InfoCard | 100.010.477 |
| Chemical and physical data | |
| Formula | C10H13NO3 |
| Molar mass | 195.215 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
It has been used in the treatment of pheochromocytoma.[2] It has been demonstrated to inhibit the production of melanin.[3]
Pharmacology
Effect on catecholamine biosynthesis
AMPT inhibits catecholamine biosynthesis at the first step—the hydroxylation of tyrosine.[4] Reduction in catecholamines and their metabolites (normetanephrine, metanephrine, and 4-hydroxy-3-methoxymandelic acid) result from the inhibition of tyrosine using AMPT.[4] AMPT doses of 600 to 4,000 mg per day cause a 20 to 79 percent reduction in total catecholamines in Pheochromocytoma patients.[4] Increase in dosage increases the magnitude of catecholamine synthesis inhibition.[4] This increasing inhibitory effect is seen in dosages up to 1500 mg per day; at higher doses, the inhibitory effect of AMPT decreases.[4] The maximum effect of orally administered AMPT occurs 48 to 72 hours after administration of the drug.[5] Catecholamine production levels return to normal 72 to 96 hours after administration of the drug ceases.[6] Dosages as low as 300 mg per day have been found to have an effect on catecholamine production, which can be measured through urinary excretion analysis and cerebral spinal fluid assays.[4] AMPT is successful at inhibiting catecholamine production in humans whether the rate of synthesis is high, as in pheochromocytoma, or normal as in patients with hypertension.[5]
Pharmacokinetics
Absorption AMPT is minimally metabolized by the body and absorbed well after oral ingestion making its bioavailability high.[4] Single-dose studies have shown that a 1,000 mg dose results in AMPT levels in the plasma of 12-14 µg/mL after 1 to 3 hours of ingestion.[6] Maintenance-dose studies have shown that absorption of AMPT is overall the same in all individuals taking doses in the range of 300-4,000 mg per day.[6]
Half-life
The half-life of AMPT in normal patients is 3.4 to 3.7 hours.[4] In amphetamine addicts the half-life is 7.2 hours.[4]
Elimination
Small amounts of metabolites (alpha-methyldopa and alpha-methyldopamine) were found after the administration of both single-doses and maintenance-doses of AMPT.[5] Small amounts of methyltyramine and alpha-methylnoradrenaline were found in patients undergoing AMPT therapy.[5] Urine analysis also recovered 45 to 88 percent of unchanged AMPT after drug ingestion.[4] Of the total AMPT excreted, 50 to 60 percent appeared in urine within the first 8 hours and 80 to 90 percent appeared within 24 hours of oral administration.[4]
Medical Use
Pheochromocytoma
Pheochromocytoma is a rare neuroendocrine tumor that results in the release of too much epinephrine and norepinephrine, hormones that control heart rate, metabolism, and blood pressure.[7] AMPT was used in the 1960s for preoperative pharmacological control of catecholamine overexpression that causes hypertension and other arterial and cardiac abnormalities.[8] The use of AMPT to treat Pheochromocytoma prior to surgery was discontinued due to its extensive side effects.[8]
Drug Interactions
Psychosis- Phosphorylation of tyrosine hydroxylase at Ser31 or Ser40 can increase dopamine biosynthesis; therefore an increase in pSer31 or pSer40 elevates dopamine synthesis in DA neurons.[2] Excessive dopamine in the mesolimbic pathways of the brain produces psychotic symptoms.[1] Antipsychotic medications block dopamine D2 receptors in the caudate and putamen as well as in limbic target areas, they can also block or partially block serotonin.[1] Therapy with AMPT could prove to be more specific to dopamine and therefore eliminate some of the negative side effects of antipsychotic drugs.
Cocaine and Methamphetamines- The dopamine transporter (DAT) is a principal site of action for cocaine. Cocaine inhibits DAT function and vesicular dopamine transport (VMAT).[9] Cocaine administration abruptly and reversibly increases both the Vmax of dopamine uptake and the Bmax of vesicular monoamine transporter-2 (VMAT-2) ligand (dihydrotetrabenazine) binding.[9] Dopamine depletion resulting from administration of AMPT had similar neuropharmacological effects as cocaine.[9] Administration of methamphetamine, a dopamine-releasing agent, rapidly decreased vesicular uptake.[9] A relationship between cytoplasmic dopamine concentration and VMAT activity was established using cocaine, methamphetamines, and AMPT. Although it is not well understood, this relationship allows for AMPT’s inhibitory property, which blocks tyrosine hydroxylase, to increase dopamine transport by the vesicle monoamine transporter-2.[9] This leads to a reduction in the newly synthesized pool of dopamine from replenished tyrosine.[10] AMPT’s effect on dopamine concentration and transport is reversible and short-lived. If methamphetamine is administered while cytoplasmic dopamine is depleted to about 50% of the control levels, its neurotoxic effects are averted (Thomas et al., 2008). The recovery of dopamine to normal levels after AMPT administration takes about 2 to 7 days, and this repletion of dopamine is not changed by methamphetamine.[10] For these reasons AMPT seems to be a better treatment drug in methamphetamine addicts than reserpine, which is also being researched as a possible methamphetamine treatment drug. Reserpine causes almost full loss of dopamine from the striatum by disrupting vesicle storage. The repletion of dopamine after reserpine administration is slower than AMPT.[10] Additionally, administration of reserpine when dopamine is maximally depleted causes neurotoxic effects, which does not occur with AMPT treatment.[10] AMPT’s role in addiction has also been studied via changes in dopamine binding to D2 and D3 receptors in the striatum (caudate, putamen, and ventral striatum) after the administration of AMPT.[11] Findings revealed that cocaine-dependent subjects exhibited lower levels of endogenous dopamine relative to healthy subjects after AMPT administration. Similar positive effects were found in the role of AMPT in methamphetamine-addicted subjects.
Dystonia and Dyskinesia- Dystonias and dyskinesias onset seems to derive from inconsistent regulation of dopamine in dopamine pathways.[2] AMPT’s ability to deplete dopamine in the CNS makes it a promising target for treatment of dopamine related disorders.
Side-effects
AMPT administration in healthy subjects has shown to cause increased sleepiness, decreased calmness, increased tension and anger, and a trend for increased depression.[4] Sedation was also reported as a side effect of AMPT ingestion. However, sedation was not seen in AMPT doses of less than 2g per day.[6] Patients have reported insomnia as a withdrawal symptom post AMPT exposure.[5] When L-dopa is administered following AMPT administration, the effects of AMPT are reversed.[12] These findings suggest that AMPT's effect on alertness and anxiety is catecholamine-specific and further supports that catecholamines are involved in the regulation of normal states of arousal and pathological anxiety symptoms.[12] Patients have reported hand, leg, and trunk tremors as well as tightening of the jaw post AMPT drug therapy. These Parkinson like side effects are supported by the lack of dopamine in the brain as in Parkinson’s patients.[4] Tourette syndrome patients treated with AMPT developed akinesia, akathisia, and oculogyric crisis.[13] Most severe of all, patients developed crystalluria (crystals in the urine) after undergoing AMPT drug treatments.[13]
Prolonged administration can have an impact upon the circadian rhythm.[14]
Mechanism
As a competitive inhibitor of tyrosine hydroxylase, it prevents the conversion of tyrosine to L-DOPA, the precursor to dopamine. This results in lowered systematic catecholamine (dopamine, epinephrine and norepinephrine) levels.
References
- Nestler, Eric J.; Hyman, Steven E.; Malenka, Robert C. (2008). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience, Second Edition. McGraw Hill Professional. ISBN 9780071641197.
- Ankenman, Ralph; Salvatore, Michael F. (2007). "Low Dose Alpha-Methyl-Para-Tyrosine (AMPT) in the Treatment of Dystonia and Dyskinesia". The Journal of Neuropsychiatry and Clinical Neurosciences. 19 (1): 65–69. doi:10.1176/jnp.2007.19.1.65. ISSN 0895-0172. PMID 17308229.
- Drago, Filippo (2002), Use of α-methyl-p-tyrosine to inhibit melanin production in iris melanocytes, retrieved November 6, 2016
- Brogden, R. N.; Heel, R. C.; Speight, T. M.; Avery, G. S. (1981). "alpha-Methyl-p-tyrosine: a review of its pharmacology and clinical use". Drugs. 21 (2): 81–89. doi:10.2165/00003495-198121020-00001. ISSN 0012-6667. PMID 7009139.
- Engelman, Karl; Horwitz, David; Jéquier, Eric; Sjoerdsma, Albert (1968). "Biochemical and pharmacologic effects of α-methyltyrosine in man". Journal of Clinical Investigation. 47 (3): 577–594. doi:10.1172/JCI105754. ISSN 0021-9738. PMC 297204. PMID 5637145.
- Engelman, K; Sjoerdsma, A (1966). "Inhibition of Catecholamine Biosynthesis in Man". Circulation Research. 18 (S6): I–104–I–109. doi:10.1161/01.RES.18.S6.I-104. ISSN 0009-7330.
- [Encyclopedia, A.D.A.M. "Causes, Incidence, and Risk Factors." Pheochromocytoma. U.S. National Library of Medicine, 18 Nov. 0000. Web. 11 May 2012.].
- Prys‐Roberts, C. (2000). "Phaeochromocytoma—recent progress in its management". British Journal of Anaesthesia. 85 (1): 44–57. doi:10.1093/bja/85.1.44. ISSN 0007-0912. PMID 10927994.
- Brown, Jeffrey M.; Hanson, Glen R.; Fleckenstein, Annette E. (2001). "Regulation of the Vesicular Monoamine Transporter-2: A Novel Mechanism for Cocaine and Other Psychostimulants". Journal of Pharmacology and Experimental Therapeutics. 296 (3): 762–767. ISSN 0022-3565. PMID 11181904.
- Thomas, David M.; Francescutti-Verbeem, Dina M.; Kuhn, Donald M. (2016). "The newly synthesized pool of dopamine determines the severity of methamphetamine-induced neurotoxicity". Journal of Neurochemistry. 105 (3): 605–616. doi:10.1111/j.1471-4159.2007.05155.x. ISSN 0022-3042. PMC 2668123. PMID 18088364.
- Martinez, Diana; Greene, Kaitlin; Broft, Allegra; Kumar, Dileep; Liu, Fei; Narendran, Rajesh; Slifstein, Mark; Van Heertum, Ronald; Kleber, Herbert D. (2016). "Lower Level of Endogenous Dopamine in Patients With Cocaine Dependence: Findings From PET Imaging of D2/D3 Receptors Following Acute Dopamine Depletion". The American Journal of Psychiatry. 166 (10): 1170–1177. doi:10.1176/appi.ajp.2009.08121801. ISSN 0002-953X. PMC 2875882. PMID 19723785.
- McCann, Una D.; Thorne, David; Hall, Martica; Popp, Kathy; Avery, Warren; Sing, Helen; Thomas, Maria; Belenky, Gregory (1995). "The Effects of L-Dihydroxyphenylalanine on Alertness and Mood in α-Methyl-Para-Tyrosine-Treated Healthy Humans" (PDF). Neuropsychopharmacology. 13 (1): 41–52. doi:10.1016/0893-133X(94)00134-L. ISSN 0893-133X. PMID 8526970.
- Sweet, Richard D.; Bruun, Ruth; Shapiro, Elaine; Shapiro, Arthur K. (1974). "Presynaptic Catecholamine Antagonists as Treatment for Tourette Syndrome: Effects of Alpha Methyl Para Tyrosine and Tetrabenazine". Archives of General Psychiatry. 31 (6): 857–61. doi:10.1001/archpsyc.1974.01760180095012. ISSN 0003-990X. PMID 4613321.
- Zimmermann RC, Krahn LE, Klee GG, Ditkoff EC, Ory SJ, Sauer MV (2001). "Prolonged inhibition of presynaptic catecholamine synthesis with alpha-methyl-para-tyrosine attenuates the circadian rhythm of human TSH secretion". J. Soc. Gynecol. Investig. 8 (3): 174–178. doi:10.1016/S1071-5576(01)00104-6. PMID 11390253.