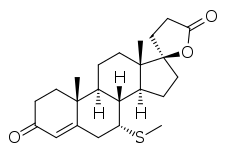
7α-Thiomethylspironolactone
7α-Thiomethylspironolactone (7α-TMS; developmental code name SC-26519) is a steroidal antimineralocorticoid and antiandrogen of the spirolactone group and the major active metabolite of spironolactone.[1] Other important metabolites of spironolactone include 7α-thiospironolactone (7α-TS; SC-24813), 6β-hydroxy-7α-thiomethylspironolactone (6β-OH-7α-TMS), and canrenone (SC-9376).[2][3][1][4]
 | |
| Clinical data | |
|---|---|
| Other names | 7α-TMS; SC-26519; 17α-Hydroxy-7α-(methylthio)-3-oxopregn-4-ene-21-carboxylic acid γ-lactone |
| Drug class | Antimineralocorticoid |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C23H32O3S |
| Molar mass | 388.57 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Spironolactone is a prodrug with a short terminal half-life of 1.4 hours.[5][6][7] The active metabolites of spironolactone have extended terminal half-lives of 13.8 hours for 7α-TMS, 15.0 hours for 6β-OH-7α-TMS, and 16.5 hours for canrenone, and accordingly, these metabolites are responsible for the therapeutic effects of the drug.[5][6]
7α-TS and 7α-TMS have been found to possess approximately equivalent affinity for the rat ventral prostate androgen receptor (AR) relative to that of spironolactone.[8] The affinity of 7α-TS, 7α-TMS, and spironolactone for the rat prostate AR is about 3.0 to 8.5% of that of dihydrotestosterone (DHT).[8]
| Compound | Cmax (day 1) | Cmax (day 15) | AUC (day 15) | t1/2 |
|---|---|---|---|---|
| Spironolactone | 72 ng/mL (173 nmol/L) | 80 ng/mL (192 nmol/L) | 231 ng•hour/mL (555 nmol•hour/L) | 1.4 hours |
| Canrenone | 155 ng/mL (455 nmol/L) | 181 ng/mL (532 nmol/L) | 2,173 ng•hour/mL (6,382 nmol•hour/L) | 16.5 hours |
| 7α-TMS | 359 ng/mL (924 nmol/L) | 391 ng/mL (1,006 nmol/L) | 2,804 ng•hour/mL (7,216 nmol•hour/L) | 13.8 hours |
| 6β-OH-7α-TMS | 101 ng/mL (250 nmol/L) | 125 ng/mL (309 nmol/L) | 1,727 ng•hour/mL (4,269 nmol•hour/L) | 15.0 hours |
| Sources: See template. | ||||
7α-TMS has been found to account for around 80% of the potassium-sparing effect of spironolactone,[6][9][10] whereas canrenone accounts for the remaining approximate 10 to 25% of the potassium-sparing effect of the drug.[11]
References
- Yang J, Young MJ (2016). "Mineralocorticoid receptor antagonists-pharmacodynamics and pharmacokinetic differences". Curr Opin Pharmacol. 27: 78–85. doi:10.1016/j.coph.2016.02.005. PMID 26939027.
- Parthasarathy HK, MacDonald TM (2007). "Mineralocorticoid receptor antagonists". Curr. Hypertens. Rep. 9 (1): 45–52. doi:10.1007/s11906-007-0009-3. PMID 17362671.
- Kolkhof P, Bärfacker L (2017). "30 YEARS OF THE MINERALOCORTICOID RECEPTOR: Mineralocorticoid receptor antagonists: 60 years of research and development". J. Endocrinol. 234 (1): T125–T140. doi:10.1530/JOE-16-0600. PMC 5488394. PMID 28634268.
- Doggrell SA, Brown L (2001). "The spironolactone renaissance". Expert Opin Investig Drugs. 10 (5): 943–54. doi:10.1517/13543784.10.5.943. PMID 11322868.
- Sica DA (2005). "Pharmacokinetics and pharmacodynamics of mineralocorticoid blocking agents and their effects on potassium homeostasis". Heart Fail Rev. 10 (1): 23–9. doi:10.1007/s10741-005-2345-1. PMID 15947888.
- Maron BA, Leopold JA (2008). "Mineralocorticoid receptor antagonists and endothelial function". Curr Opin Investig Drugs. 9 (9): 963–9. PMC 2967484. PMID 18729003.
- Oxford Textbook of Medicine: Vol. 1. Oxford University Press. 2003. pp. 1–. ISBN 978-0-19-262922-7.
- Cutler GB, Pita JC, Rifka SM, Menard RH, Sauer MA, Loriaux DL (1978). "SC 25152: A potent mineralocorticoid antagonist with reduced affinity for the 5 alpha-dihydrotestosterone receptor of human and rat prostate". J. Clin. Endocrinol. Metab. 47 (1): 171–5. doi:10.1210/jcem-47-1-171. PMID 263288.
- International Agency for Research on Cancer; World Health Organization (2001). Some Thyrotropic Agents. World Health Organization. pp. 325–. ISBN 978-92-832-1279-9.
- Agusti G, Bourgeois S, Cartiser N, Fessi H, Le Borgne M, Lomberget T (2013). "A safe and practical method for the preparation of 7α-thioether and thioester derivatives of spironolactone". Steroids. 78 (1): 102–7. doi:10.1016/j.steroids.2012.09.005. PMID 23063964.
- Pere Ginés; Vicente Arroyo; Juan Rodés; Robert W. Schrier (15 April 2008). Ascites and Renal Dysfunction in Liver Disease: Pathogenesis, Diagnosis, and Treatment. John Wiley & Sons. p. 229. ISBN 978-1-4051-4370-7.
Further reading
- Gardiner P, Schrode K, Quinlan D, Martin BK, Boreham DR, Rogers MS, Stubbs K, Smith M, Karim A (1989). "Spironolactone metabolism: steady-state serum levels of the sulfur-containing metabolites". J Clin Pharmacol. 29 (4): 342–7. doi:10.1002/j.1552-4604.1989.tb03339.x. PMID 2723123.